1. Context
Anterior Cruciate Ligament (ACL) injury is common in dynamic sports activities and accounts for approximately 26% of all internal knee injuries (1). The annual cost of ACL injury, if treated with surgical reconstruction, is around $6.7 billion, while it amounts to approximately $17.7 billion when managed with rehabilitation treatment (2). Moreover, more than 25% of individuals who sustain ACL injuries cannot return to their previous activity levels even after surgery and successful rehabilitation. Anterior cruciate ligament injuries can have short-term or long-term physical, psychological, and vocational consequences, to the extent that they may even completely end their professional activity (3, 4). These injuries lead to prolonged and significant absence from sports for the athlete and impose heavy financial burdens on the athlete, their family, team, and club (5). The high risk of early-onset osteoarthritis and reduced quality of life also result from this injury (6, 7).
However, ACL reconstruction surgery remains a standard treatment for athletes who wish to pursue their sports careers seriously and in a pre-injury manner (8). Due to weaknesses in rehabilitation and return-to-sport programs, fewer individuals can return to their professional level after ACL reconstruction, with 45% unable to do so after 9 months (9) and 33% after 12 months (10). Additionally, one-fourth of athletes who successfully return to their professional sports will experience another injury in the knee area (11-13). Of course, after the second ACL injury, the reconstruction surgery is not likely to be as successful. Up to 55% of recurrent ACL injuries have been observed as non-contact events (14). From these statistics, it can be inferred that even after complete reconstruction and rehabilitation, there are deficiencies in the functioning of the sensory-motor system, resulting in a loss of motor control. In fact, contrary to previous assumptions, with an ACL injury, it is not only the structural stability of the knee that is compromised, as it should seemingly be restored with reconstruction surgery (15-17). The tearing of the ACL and the loss of its mechanical receptors disrupt the transmission of sensory-motor signals in the knee. Following this disruption, the individual’s motor control is compromised, with a dynamic knee valgus being a sign of it during sports activities (18).
In recent years, the use of Virtual Reality (VR) and Augmented Reality (AR) tools has significantly impacted evaluating athletes’ performance in returning to sports and for neuro-muscular training across all age groups. Athletes can train in a controlled three-dimensional simulation of their sport’s environment, using laboratory facilities to replicate reality closely (19, 20).
The VR environments have been used for rehabilitation in medical science, neuroscience, and psychology. However, their values in sports injury rehabilitation and aiding the return-to-sport process have not been adequately addressed. There is no precise definition of how VR technology can be utilized for sports injury prevention and rehabilitation. In the existing literature and research studies on “Sports Training using AR and VR Tools for Injury Prevention and Accelerating the Rehabilitation Process and Return to Sports,” only small references have been made by Düking et al. to the opportunities that AR and VR technology can provide for helping injured athletes (20).
Existing literature may exhibit three biases: Selection bias, performance bias, and reporting bias. Selection bias arises when studies do not use random participant sampling, which can lead to distorted treatment effect estimates. Performance bias can occur when interventions like VR or AR training impact participant motivation, potentially skewing treatment effects. Reporting bias arises from a greater likelihood of publishing studies with positive results, leading to overestimating treatment effects. Also, the existing literature on VR and AR training programs for injury prevention and rehabilitation has several limitations. These include a lack of standardization, limited studies, limited participant diversity, short-term follow-up, lack of comparison groups, and limited real-world application. These limitations hinder the ability to draw accurate conclusions about the effectiveness of these training programs. Most studies focus on young, healthy athletes, limiting the generalizability of findings to a broader population.
Additionally, the short-term follow-up periods restrict the assessment of long-term training efficacy. The absence of control or comparison groups makes it challenging to determine relative effectiveness compared to other interventions. Furthermore, using VR and AR training programs in real-world settings remains limited. Addressing these limitations and conducting further research is necessary to standardize and optimize the use of these training programs, promote their safe and effective application across diverse populations, and evaluate their real-world feasibility and effectiveness.
The lack of standardization in using VR and AR training programs and evaluating their outcomes, along with short treatment periods, small sample sizes, and absence of control or comparison groups, limits the interpretability and generalizability of results. Additionally, these factors hinder assessing long-term effectiveness and the ability to differentiate between treatment effects and natural recovery processes.
However, over time and with the publication of new research articles in the field of rehabilitation and prevention of sports injuries using controlled and interactive VR environments, it seems that there is a need for a comprehensive review (21) that identifies and examines up-to-date scientific evidence and research to obtain a comprehensive view and overview of methods and results of empirical studies on VR-based exercises for rehabilitation of sports injuries and speeding up the return to sports. Based on the authors’ search, no review article was found specifically summarizing and presenting a general perspective on the impact of VR exercises on the rehabilitation of sports injuries, and previous studies in this field have contradictory results. Therefore, conducting a comprehensive review of research is necessary to address the current gaps in knowledge regarding VR-based exercises for ACL injury rehabilitation. This review aims to summarize and disseminate the findings of previous research in this area (22) while also identifying areas that require further investigation. By doing so, it will provide a clearer direction for future research endeavors and enhance the vibrancy of this field. This scoping review aims to answer the question of how VR and AR exercises impact ACL injury prevention and rehabilitation.
2. Evidence Acquisition
2.1. Protocol and Registration
The present study is a scoping review based on the PRISMA-ScR reporting system (23) and the Joanna Briggs Institute guidelines for conducting various stages of work and data extraction (24). The study is registered in the PROSPERO database with the code CRD42023446354.
2.2. Eligibility Criteria
(1) Study Design: We included primary research studies, randomized controlled trials, quasi-experimental studies, and case-control studies.
(2) Participants: We focused on studies involving athletes who had experienced ACL injuries of all ages, genders, and levels of sporting activity.
(3) Type of injury: Samples should have unilateral ACL injury (primary or recurrent) not undergoing rehabilitation treatment. We also included samples with injuries that occurred together with an ACL injury.
(4) Interventions: We include studies that utilized VR and AR training interventions for injury prevention or rehabilitation purposes related to ACL injuries. This could include rehabilitation training programs, post-surgical rehabilitation protocols, and exercises to enhance neuromuscular control, proprioception, and functional tasks specific to ACL injury prevention or recovery.
(5) Outcomes: We included studies that assessed outcomes related to injury prevention or rehabilitation of ACL injury in athletes using VR and AR training. This could encompass ACL injury incidence, functional performance (e.g., balance, agility, jump performance), proprioceptive abilities, neuromuscular control, return to sport outcomes, and patient-reported results.
(6) Language and publication date: We included studies published in English without time restrictions until the end of June 2022.
2.3. Exclusion Criteria
We excluded studies:
(1) In which the participants had injuries other than ACL
(2) That did not specifically target ACL injuries or included participants without ACL injuries
(3) Focusing solely on VR or AR without direct relevance to ACL injury prevention or rehabilitation
(4) That did not report effects related to ACL injury prevention or rehabilitation using VR and AR training
(5) In gray literature (including unpublished or ongoing experiments, unfinished annual reports, letters, newspaper articles, and non-peer-reviewed journal articles)
(6) That were review articles, editorials, commentaries, and conference abstracts.
2.4. Information Sources
2.4.1. Search Strategy
Reputable electronic databases, such as PubMed, Embase, Web of Science, SPORTDiscuss, PsycINFO, CINAHL, and Cochrane, were searched. These databases provide a wide range of scientific literature across multiple disciplines. The search utilized specific keywords related to the topic: VR, AR, Simulation, Rehabilitation, Injury Prevention, Anterior Cruciate Ligament, and ACL. These keywords were selected to capture relevant ACL injury prevention and rehabilitation articles using VR and AR reality technologies. The search was limited to articles published in the English language to ensure the inclusion of accessible literature for analysis and synthesis. Articles published until the end of June 2022 were included to identify the most recent evidence in this area. A search strategy was formulated using a combination of Boolean operators (AND, OR) and truncation. The primary elements of the search strategy included the following terms: (“Virtual Reality” OR “Augmented Reality” OR “Simulation”) AND (“Rehabilitation” OR “Injury Prevention”) AND (“ACL” OR “Anterior Cruciate Ligament”). This approach aimed to capture articles that specifically addressed the use of VR and AR in ACL injury prevention and rehabilitation. Additionally, a comprehensive manual search of reference lists in the identified relevant articles was conducted to ensure coverage of the literature.
2.5. Risk of Bias
Two authors (SS and MBT) assessed the included studies for bias using the Cochrane Collaboration’s risk of bias tool (25).
2.6. Process of Data Collection (Articles)
The data extraction process involved the following steps:
(1) Systematic Search: Two authors (SS and MBT) independently conducted a systematic search in relevant databases to identify titles and abstracts of potential articles—the search strategy aimed to capture relevant literature on the topic.
(2) Removal of Duplicate Records: The search results were imported into EndNote (version X9 for Windows), and duplicate records from different databases were identified and removed to ensure the inclusion of unique articles in the review.
(3) Eligibility Assessment: Both authors (SS and MBT) reviewed the titles and abstracts of the identified articles to assess their eligibility based on predefined inclusion and exclusion criteria. Only articles that appeared to meet the criteria were considered for full-text assessment.
(4) Full-text Review: The authors independently reviewed the full texts of the selected articles to determine their suitability for inclusion in the scoping review based on the predefined criteria. Any disagreements in article inclusion between the two authors were discussed and resolved, if needed, with the involvement of other authors (HM and MSA), ensuring a consensus was reached.
(5) Reference List Review: The final stage included a manual examination of the reference lists of the articles to identify any additional potential sources that may have been missed in the initial search.
2.7. Data Analysis
To organize and summarize extracted data, statistical principles like averaging and subtraction were used in Microsoft Excel.
3. Results
3.1. Selection of Sources of Evidence
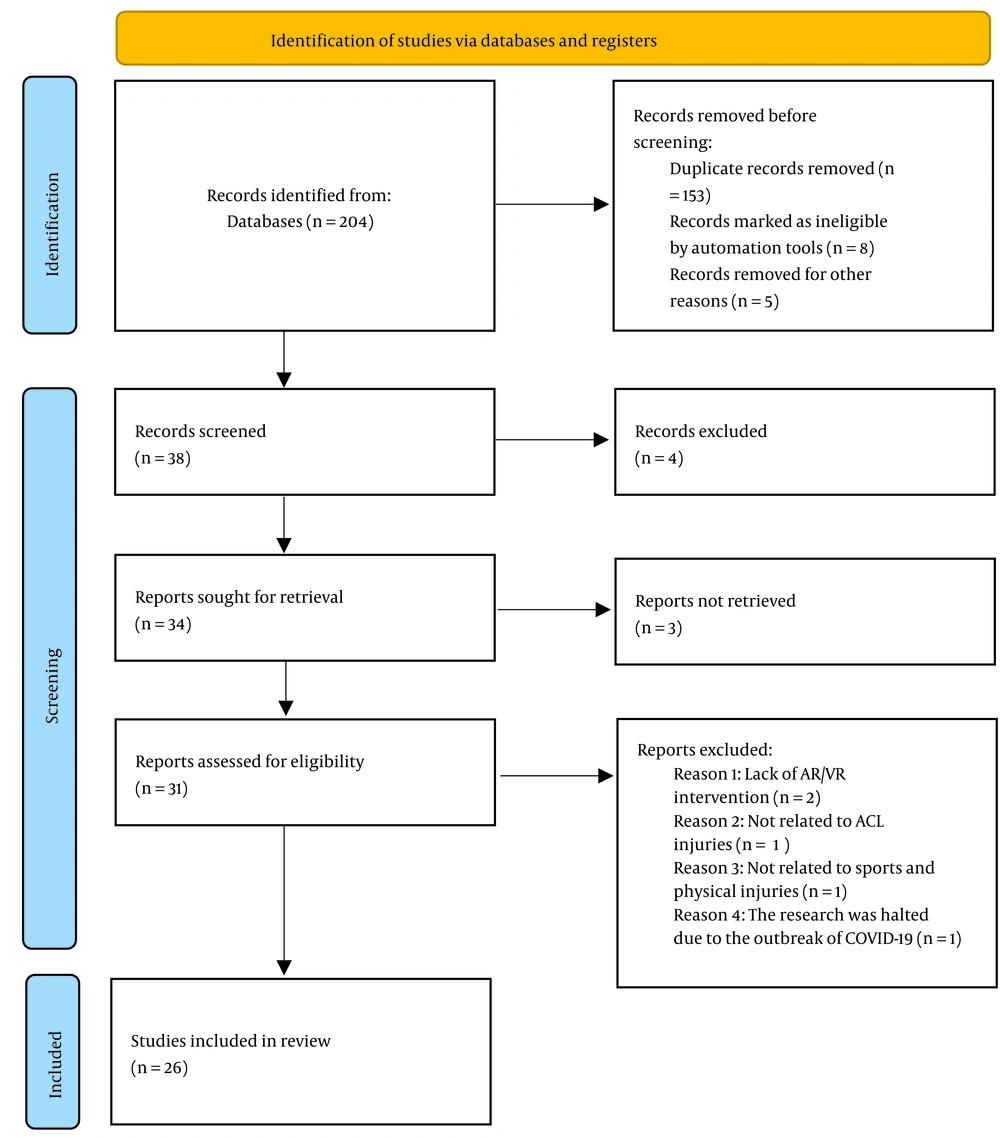
Of 204 articles found in the databases based on the keywords, 166 duplicate articles were removed. After the screening of titles and abstracts, 4 articles were excluded. Thus, thirty-four full-text papers were reviewed, and three articles were excluded. Five articles were excluded from the study according to the inclusion and exclusion criteria (Figure 1). A total of 26 articles were thoroughly reviewed. Most of the selected literature (57%; 15 out of 26) was published between 2018 and 2021. Of the 26 articles, 11 were reviews, and 15 had experimental studies using different exercise methods (Table 1). Out of this number, five studies used AR, and 10 used VR. Among the articles that included interventions or evaluations, seven focused on single-session risk assessment of ACL injury, and eight focused on exercise or evaluation in two or multiple sessions.
| First Author (y) + Journal | Authors’ Results and Conclusions About My Study | Sample Size | Target Population | Duration of Study (If Applicable) | Article Purpose | Type of Intervention (VR/AR) |
|---|---|---|---|---|---|---|
| Gérin-Lajoie et al., 2010 (26) | The potential of using ambulatory virtual environments, specifically VR, for assessing functional gait impairment and detecting mobility deficits resulting from lower extremity disabilities | Eleven young, healthy Adults (6 W, 5 M) | Study individuals with global functional gait impairment caused by lower extremity disabilities and observe how their mobility changes following injury or treatment. | One assessment session | Develop assessment tools providing a quantitative description of functional mobility and explore the potential of VR for gait assessment and rehabilitation. | Use of ambulatory virtual environments for the assessment of functional gait impairment. |
| Cortes et al., 2011 (27) | The VR protocol can have broader implications in developing diverse clinical applications for various musculoskeletal/neurological disorders. | 13 female collegiate soccer athletes | Athletes who face unanticipated ted tasks in their field of sports which are possibly associated with ACL injury | One assessment session | To assess differences between unanticipated and anticipated lower extremity biomechanics while performing a sidestep-cutting task that would recreate a soccer game situation for use in a laboratory setting. | VR environment of a soccer game + VICON motion analysis system + two force plates |
| Baltaci et al., 2013 (28) | Both groups showed similar improvements in muscle strength, dynamic balance, and functional performance. The study also suggested that engaging in Wii Fit activities, similar to conventional rehabilitation, could help achieve physical therapy goals, such as enhancing visual-perceptual processing, coordination, proprioception, and functional mobility. | 30 volunteer male subjects that had ACLR | All people who undergo ACLR | 12- week- program following ACLR for G1 and G2 | Compare the effects of Nintendo Wii Fit-based rehabilitation with conventional rehabilitation on functional performance outcomes in patients who underwent hamstring ACLR | G1: 4 Nintendo Wii games for the Wii Balance Board (WBB) G2: Conventional rehabilitation |
| Gokeler et al., 2013 (29) | Providing real-time biomechanical feedback during slow exercises can potentially benefit patients who are recovering from ACL reconstruction (ACLR) surgery, specifically by addressing persistent side-to-side asymmetries and specific movement abnormalities. | Not mentioned | Patients who undergo ACLR and are at risk of a second injury | Not mentioned | This article presents new insights gained from the motor learning domain that may improve neuromuscular training programs via increased retention from improved techniques and ultimately reduce the incidence of second ACL injuries. | (1) Various feedback techniques, (2) Practicing in Dyads, (3) Video Overlay of Ideal Movement Patterns |
| Ford et al., 2015 (30) | Using biofeedback during training sessions led to notable improvements in the knee abduction angle and moment during landing trials. This suggests that the subjects were able to effectively adjust their lower-extremity frontal plane positioning and torque as a result of the biofeedback training. | 4 female high school soccer players | Female athletes at risk of ACL injury | Single session | To determine whether the feedback provided during a squat task transfer to the more dynamic mechanics involved in a plyometric drop vertical jump (DVJ) task. | Motion and force data presented to athletes in real-time biofeedback during double-leg squats using Visual 3D + Baseline and post-training drop vertical jumps to determine transfer to another activity |
| Gokeler et al., 2016 (31) | VR had a significant impact on the knee biomechanics of patients who had undergone ACL reconstruction compared to a control group. The results suggest that engaging in a realistic VR scenario can potentially distract these patients from consciously controlling their movements. | 40 athletes, 20 men, 20 women, 20 ACLR | Patients who undergo ACLR | One session | To evaluate the influence of immersion in a VR environment on knee biomechanics in patients after ACL reconstruction (Diagnostic Research Design) | A step-down task in both a non-VR environment and aVR environment displaying a pedestrian traffic scene. |
| Karakoc et al., 2016 (32) | The intervention, likely involving the use of Wii games, led to improved lower extremity functionality and increased range of motion in the participants. | 9 male ACLR patients | Patients who had undergone ACLR | 6 weeks | Examine the effects of augmenting standard rehabilitation with virtual rehabilitation in individuals undergoing ACL reconstruction. | Conventional physiotherapy program for 6 weeks + After 3 weeks of rehabilitation, Nintendo Wii U Balance Games were added (VR) |
| Kiefer et al., 2017 (33) | The article’s conclusion underscores the positive outcomes of aNMT in terms of fostering an injury-resistant biomechanical profile that can be transferred to sport-specific contexts. Additionally, the findings support the use of VR scenarios as a reliable tool for assessing the transfer of skills acquired in laboratory settings to competitive sports environments. | 7 athletes. 5 trained and 2 untrained CTRL | Female soccer athletes | 6 weeks of aNMT 3 times per week + 2 assessment sessions of cutting scenario with VR in weeks 1 and 8 (pre and post) | To assess the skill transfer and biomechanical outcomes of incorporating a custom, wireless HMD in conjunction with a soccer-specific VR cutting task. | A biofeedback-driven augmented NMT (aNMT) was presented to athletes by a custom, wireless HMD combined with a soccer-specific VR. |
| Duking et al., 2018 (20) | The article concludes that VR systems offer promise in improving certain facets of athletic performance, such as tactics and creativity. Additionally, in diagnostic rehabilitation, VR has the potential to enhance procedures by allowing unsupervised training. | Not mentioned | Athletes | Not mentioned | This analysis is developed for strategic planning of developmental processes and to point out (SWOT) associated with the use of VR. | VR systems (bio-feedback) |
| Grooms et al., 2018 (34) | Changes in brain activity are closely related to the enhancement of landing mechanics and the reduction of injury risk. The findings highlight the importance of incorporating exercises targeting motor planning, sensory, and visual regions, as well as modifying the motor cortex activity, to promote the adaptation and transfer of injury risk-reducing movement mechanics to sports activities. | 4 healthy high school soccer athletes | Female athlete adolescents | 6 weeks of aNMT | To determine the neural mechanisms for injury risk-reducing biomechanics transfer to sport after ACL injury prevention training utilizing augmented neuromuscular training utilizing real-time visual feedback. | aNMT +pre- and post-VR sport-specific landing biomechanics testing presented for the athlete on screen + functional magnetic resonance imaging |
| Aydogdu and Sari, 2018 (35) | Wearable technology in the form of virtual rehabilitation can offer potential benefits for treating patients with anterior cruciate ligament (ACL) reconstruction. | 19 ACLR patients with ACL reconstruction | Patients with ACLR | 8 weeks | How a wearable technology in the form of virtual rehabilitation can positively influence proprioception, postural stability, and fear of re-injury in patients who have undergone ACL reconstruction | Conventional physiotherapy +a virtual rehabilitation treatment with visual and auditory stimulus |
| Shultz et al., 2019 (36) | Biofeedback techniques, which engage implicit motor-learning mechanisms, offer advantages for sensorimotor adaptation and neural adaptations associated with safer landing biomechanics. | Not mentioned | Athletes in danger of primary, secondary, and tertiary risk of ACL injury | Not mentioned | To present and discuss research advances in ACL injury risk, outcomes, and prevention (Summary statement of The ACL Research Retreat VIII) | Keynote presentations focused on: (1) ACL injury biomechanics and the motions; (2) innovative augmented neuromuscular-training approaches (3); the identification of early markers of PTOA after ACL injury |
| Bonnette et al. 2020 (37) | The article suggests that VR-based assessments offer a promising approach to bridging the gap between laboratory settings and real-world sports environments, allowing for more ecologically valid assessments of athletes’ performance and injury risk. | Not mentioned | Athletes in danger of ACL injury/re-injury | Not mentioned | Points toward shortcomings in current approaches to ACL injury prevention, rehabilitation, and risk assessment methods (narrative review) | aNMT training via AR and VR + fMRI +motion capture +force plates |
| Burcal et al., 2021 (38) | VR technologies support optimized functional performance and recovery. Incorporation of these new technologies and therapies may provide a means to reduce the high re-injury rate after ACLR, as the ACL injury event is essentially a coordination error in sensory, visual, or motor processing | Not mentioned | All athletes that undergo ACLR and are at risk of another non-contact ACL rupture | Not mentioned | Explain multimodal rehabilitation and give a theoretical case study example (narrative review) | Modalities include training with an external focus of attention, implicit feedback, differential learning, novel sensory reweighting, and VR technologies. |
| Diekfuss et al., 2021 (39) | The article emphasizes the potential of integrating technology and instructional approaches to enhance the effectiveness of injury management and exercise performance programs. | Not mentioned | Young athletes in danger of ACL injury | Not mentioned | Combines practical recommendations for incorporating the OPTIMAL PREP theory into injury prevention for youth and an overview of technological advancements supporting its application in the rehabilitation of ACL injuries | Implementation of optimal Prep training strategies by verbal/ instruction-based feedback or by automated augmented biofeedback via visual displays of computer (VR/AR, marker-less motion capture, eye tracking) |
| Bonnette, et al., 2020 (37) | There were significant improvements in heat map scores (7.7%) and drop vertical jump (DVJ) performance from pretest to posttest. These improvements indicate that participants were able to enhance multiple key biomechanical variables that are relevant across different tasks, ranging from squats to DVJ. | 11 adolescent female athletes | Athletes in danger of ACL injury | Single training session | Introduce and examine the implementation of a new biofeedback system designed to mitigate the biomechanical risk factors linked to anterior cruciate ligament (ACL) injuries. | Bodyweight squats while interacting with the real-time biofeedback (with HMD) +motion capture and force plate + pretest and posttest DVJ |
| Nambi et al., 2020 (40) | The addition of VR training to regular rehabilitation programs has been found to have positive effects on inflammatory biomarkers and minimal or no impact on bone morphogenic proteins. Moreover, the immersive virtual environment in VRT has been shown to alter pain perception levels and promote comfort. | Sixty eligible Male football players with ACL injury participants were allocated into VRT (n 20), SMT (n = 20), and control groups (n 20). | Athletes who suffer from chronic (> 3 months) PTOA following ACL injury | 4 weeks | Compare the effects of VR training (VRT) and sensory-motor training (SMT) on the expression of bone morphogenetic proteins (BMP) and inflammatory biomarkers in individuals with post-traumatic osteoarthritis (PTOA) following anterior cruciate ligament (ACL) injury. | SMT group: Sensorimotor training exercises CTRL group: The participants underwent supervised conventional exercise programs for the knee muscles. VRT group: Received training with the device |
| Diekfuss et al., 2020 (39) | Many musculoskeletal prevention and rehabilitation programs primarily concentrate on motor progression through activities like strength training, proprioceptive exercises, and range of motion exercises. However, recent data suggests that neural progression should also be taken into account as an integral component of current care standards. | 30 female athletes | Athletes in danger of ACL injury | 6 weeks | Investigate the effectiveness of a real-time biofeedback system known as aNMT (accelerated neuromuscular training) in modifying knee biomechanics during high-risk landing tasks and enhancing sensorimotor function and brain functional connectivity related to the knee | The aNMT biofeedback (AR) protocol consisted of six movements presented on screen for all: +pre/post DV pre/post fMRI |
Article Bibliography
4. Discussion
This scoping review aimed to investigate the impact of VR and AR exercises on preventing ACL injury, ACL rehabilitation, and speeding up the return to sports. Based on the specified criteria, 26 articles out of 204 studies reviewed were included. The results of the studies showed that the research methods in this scientific field were not homogeneous, and various research methods had been used depending on the available facilities and participants. However, among the 15 studies conducted on participants, biomechanical parameters related to anterior cruciate ligament injury were measured using different methods to assess the impact of biofeedback in the moment, VR, or AR, and their factors were significantly changed after exercise in VR and AR environments. The ACL injury is not simply summarized in a “simple” musculoskeletal dimension that only involves mechanical or movement dysfunction. The failure of current approaches to preventing anterior cruciate ligament injury, rehabilitation, and risk assessment methods is due to not considering the cognitive and neurological aspects of the injury, and new feedback methods such as aNMT, multidimensional rehabilitation approaches, and utilizing VR technology and AR strategies that rely on the strengths of VR and AR systems (such as optimal strategy) can compensate for this scientific and practical gap.
4.1. Virtual Reality and Augmented Reality as Biofeedback Tools
The “interaction” of the individual with the virtual environment and the “receiving feedback” or “biofeedback” are essential features of these VR and AR systems. Just as looking in the mirror allows individuals to see their position or environment and change what they need, VR and AR tools also act as a biofeedback technique and by converting signals received from motion analysis cameras and force plates into meaningful visual and auditory cues, they allow individuals to see their own body and use the feedback received to adjust their physiology or kinesiology based on instructions from a coach or trained specialist or even the designed program in the VR/AR system.
Therefore, biofeedback is a self-regulation technique through which the athlete/patient/learner learns to voluntarily and actively control what they thought they could not control (or did not know they could control) under their own will (41). The interventions examined in this comprehensive review have shown that this new technology can be effective as a complementary exercise in improving sports performance. Using momentary biofeedback, such as kinetic or kinematic biofeedback, gives us an attractive option for providing enhanced feedback and can maximize the effectiveness of traditional neuromuscular intervention programs. The studies conducted in this review indicate that individuals trained with momentary biofeedback have shown immediate improvement in the mechanical aspects related to their injury (27, 28, 30, 31, 42-44), especially with increased athlete self-awareness and understanding of risky body positions and biomechanics. However, while immediate improvements are essential, maintaining long-term appropriate motor performance is crucial for the ultimate success of an intervention, which should be reassessed in follow-up performance evaluations.
The vital feature of biofeedback systems is their ability to induce implicit motor learning strategies (i.e., without explicit, specific instructions). Implicit learning helps reorganize the motor cortex and effectively utilizes the neural plasticity feature. For example, combining ACL injury prevention methods with “external focus” (i.e., verbal or non-verbal instructions that direct the individual’s attention to the outcome of the movement rather than the movement itself) may enhance functional brain connectivity through synaptic processes. Recent evidence from EEG and fMRI suggests that adopting such motor learning techniques actually affects brain activity (34, 45).
Furthermore, identifying modifiable high-risk mechanisms allows coaches and injury specialists to start screening high-risk athletes and implementing targeted interventions more quickly. Intervention studies that have successfully reduced ACL injuries have utilized biomechanical analysis and provided appropriate feedback to athletes regarding body position and proper technique during movement execution. With the emergence of motion capture technologies and mixed reality, researchers’ and physicians’ access to enhanced feedback has increased, thus enabling visual biofeedback in fields such as sports medicine and biomechanics. Several training programs focusing on ACL injury prevention have been conducted using such technologies, which are examined in this study, and the results are reported. For example, incorporating immediate visual feedback from kinematic motion analysis can improve neuromuscular exercises. This style of biofeedback has been used for gait retraining (46-48) and is also employed in non-contact ACL injury prevention programs (30, 49, 50).
4.2. Assessing the Biomechanical Movement Patterns of Athletes in a VR Environment
Considering that traditional assessments measure an individual’s biomechanical performance based on a set of standardized and uniform tests (regardless of the sports discipline), they may not accurately reveal the risky movement patterns that an individual exhibits during real sports competitions. As a result, generalizing these patterns to sports performance is limited. Therefore, it is better to precisely assess the biomechanical movement patterns of risk in each individual within a real sports environment and, if necessary, conduct standardized assessments as validation alongside it. A promising solution that may overcome the limitations of classical assessments is simulating the specific environment of each sports discipline through VR, which allows for creating scenarios that simulate real sports competitions. Evaluating and examining the biomechanics of athletes in such an environment may provide more precise insights into the risk of injury and adaptation to training during the execution of simple and fundamental tasks of their sports discipline (such as a simple football shot). The VR technology has been implemented in biomechanics analysis in the kinematics of handball throws, rugby strategies, and football-cutting maneuvers. However, the movement patterns related to injury were only examined in the last study (from which the data was extracted in this review) (43).
“Several risk factors have been assumed as mechanisms for ACL injuries. These risk factors have primarily been studied using predicted drop-box jump, stop-jump tests, or anticipated cutting tasks. Recently, a few researchers have attempted to improve the ecological validity of the experiment by designing unpredictable tests using visual stimuli (e.g., green/red lights and pointing arrows). It is expected that these visual stimuli will create a situation similar to the conditions in which athletes must quickly respond to specific stimuli.”
“However, it cannot be said that visual stimuli are similar to a typical game and competition situation (such as markers, players, grass, and a football). Virtual reality, by simulating realistic scenarios and consequently providing high ecological validity, may offer us the optimal scientific and controlled method to evaluate and measure the transfer of training to real performance in sports. Unlike recording and analyzing sports movements in an open space, VR provides a completely standardized and controlled laboratory environment. If accompanied by freedom of movement, it can create a sense of immersion in athletes and yield more realistic motor responses. Additionally, Cortes et al. (27) interpreted from their research that using a visual scenario in VR, which closely resembles a game on a football field, resulted in differences between their research data and others, indicating improved ecological validity. This can increase the generalizability of assessment results to reality. In programs that prevent recurrent ACL injuries, VR technology can provide realistic scenario immersion for athletes in complex sports conditions similar to the playing field and facilitate better evaluation of quick decision-making skills.”
The data from one of our reviewed studies (33) indicates that a simulated cutting scenario in a sports environment is a helpful approach for evaluating the transfer of targeted training to reduce the risk of ACL injuries in simulated competitive sports. The critical point is that VR enables systematic and controlled testing of unexpected cutting, closely resembling the perceptual-motor and decision-making behaviors that athletes typically encounter on a football field.
Logically, hitting a moving football with the head in a sinking VR environment requires more attention than towards a stationary target in a controlled laboratory environment and standard jumping (51). In this way, it can be said that the movement patterns (in the mentioned research example, jumping) obtained in the simulated sports environment in VR demonstrate a more natural self-organization and coordination of the musculoskeletal system, which appears during jumping in a specific sports environment. These movement patterns in standard laboratory conditions likely provide us with more limited and less generalizable results due to the controlled and constant nature of the environment. In comparison, movement patterns in a specific sports environment (such as a football environment simulated in VR) may create more precise motor responses. These precise responses are generated in response to specific sports goals because the athlete’s attention is devoted to specific informational variables of the sport, such as other players, equipment, rules of the game, and the environment itself. In this way, incorporating movements that naturally occur in the tested sports discipline may elevate the level of screening and evaluation for prevention and rehabilitation goals.
4.3. Biomechanical Changes in Walking
It is common to observe biomechanical changes in walking after ACL reconstruction surgery (52-54), and it is highly likely to be influential in the development of post-traumatic osteoarthritis (PTOA) (55). After surgery, most patients exhibit a knee stiffening strategy during the stance phase, where the knee is slightly more extended than normal, and the torque of the quadriceps muscle is reduced. These conditions may disrupt energy absorption in the tissues surrounding the knee (56, 57). The mechanisms that lead to abnormal load distribution during walking gait after ACL reconstruction surgery are not well understood. On the other hand, other researchers have found a direct relationship between “poor proprioception” and “less load distribution” on the operated knee during walking, suggesting a possible link between unloading the operated knee and changes in somatosensory nerve function in the lower limb (36). These seemingly contradictory findings point to a complex relationship between muscle function, joint load distribution, and changes in joint tissues after ACL surgery. The lack of understanding of this relationship represents a significant gap in our knowledge of the mechanisms leading to PTOA after surgery.
However, it has been shown that VR is a useful tool for evaluating and rehabilitating gait (26), as it appears that movement behavior is similar in both physical and virtual environments (58, 59). On this basis, VR environments that allow immersion provide a good research tool for studying the relationship between perception and action. This ability to assess gait or rehabilitation using VR is important for transferring appropriate motor skills to the real world. On the other hand, the ability to accurately measure the geometry of the path and walking speed in the VR environment has been provided, as functional parameters in this environment are well-controllable. Therefore, there is potential in VR environments for evaluating the forces exerted on the knee, walking mechanics, and perhaps even some rehabilitation exercises. In one of the studies reviewed in this review, it has been shown that VR can be used for the diagnosis and quantitative description of motor impairments using a simulated disability. This study introduced a new way to bridge the gap between local evaluations (at the joint level) and biomechanical data resulting from patient performance (26).
The focus of new research is on the rehabilitation and prevention of ACL injuries using aNMT
The focus of recent research on rehabilitation and prevention of ACL injuries is on augmented neuromuscular training (aNMT) with a real-time, interactive biofeedback stimulus, abbreviated as aNMT. Biofeedback systems can be used to provide feedback to enhance existing training strategies (neuromuscular exercises) to reduce the risk of ACL injuries by improving biomechanical control and creating neural pathways. As explained in detail, common strategies for transferring injury prevention adaptations to sports have not been successful, likely due to sensory-motor errors during sports that lead to non-contact ACL injuries. Therefore, augmented neuromuscular training (aNMT) is designed to provide real-time interactive biofeedback in the form of AR from selected biomechanical variables known as risk factors for injury.
The biofeedback variables of aNMT are calculated in real-time and visually represented by creating a geometric shape that provides feedback on the participant’s movements at that moment. The shape changes during the exercise based on the targeted biomechanical variables (for example, in the reviewed research, athletes see a rectangle on an AR display while performing a squat, which interacts with the real environment around them). The desired outcome for athletes is to perform the exercise in a way that creates a completely symmetrical shape (e.g., a symmetrical rectangle), as this reflects the correct biomechanics of the intended movement, which carries the lowest risk of injury. Any deviation from the desired movement pattern during aNMT exercise systematically and specifically alters the feedback shape. Five kinematic and kinetic variables were selected for feedback in the aNMT biofeedback system based on previous research identifying them as risk factors for ACL injury. Each of these factors has a unique impact on the aNMT biofeedback display: (1) Lateral trunk flexion, (2) knee joint torque-to-hip joint torque ratio (KHMr), (3) knee adductor torque (KAM), (4) vertical ground reaction force (vGRF), and (5) center of pressure location on the foot (COP location) (42).
The instantaneous values of the above biomechanical variables are plotted for athletes during training using a geometric shape (such as a rectangle). Athletes must discover the movement pattern that brings the stimulus shape as close as possible to the target position only with the help of the simplest exercise instructions. No other external instructions are given to the athlete regarding their movement except to create the desired geometric shape with their movements. This process engages implicit motor control mechanisms through external perceptual control. Informational feedback (non-controlling), such as what exists in aNMT, can be used to enhance intrinsic motivation and deeper learning, as this feedback fulfills the need for autonomy and competence (51). Participants learn to move with optimal and low-risk movement strategies that keep them away from ACL injuries without being able to explicitly describe how they perform it. This method is more likely to create effective and transferable sensory-motor adaptations compared to traditional exercises with verbal and explicit feedback from a coach or clinical physiotherapy, which draw the athlete’s attention to their joint positions, making motor learning more difficult.
Why should we consider the principles of motor learning in rehabilitation after injury?
Motor learning refers to the process of acquiring and improving motor skills in a relatively permanent manner. To explain how motor learning and movement improvement occur after an injury, it is necessary to integrate principles from neuroscience, psychology, and rehabilitation sciences. By applying the principles of motor learning, various clinical disorders can be improved across a wide range of injuries, such as stroke, limb amputation, and certain speech disorders (60).
Traditional approaches to musculoskeletal rehabilitation do not directly employ the principles of motor learning or aim to induce neural plasticity or sensory stimulation. These approaches also do not utilize VR technologies that aid in optimal performance and recovery. Using these technologies and new treatments may reduce the high re-injury rate after ACL reconstruction surgery, as this injury is essentially a coordination error in sensory, visual, or motor processing. Additionally, recent evidence suggests changes in the central nervous system following acute knee injuries, which may affect motor control and functional outcomes in patients after ACL surgery. Therefore, motor learning strategies and other mentioned methods may potentially be a solution to reducing neuroplastic changes after injury (which hinder rehabilitation progress).
Recent evidence has shown that considering neural factors in ACL injury and rehabilitation is essential (56). Therefore, rehabilitation protocols are optimized by adding approaches that target the sensory-motor system. Incorporating principles of motor learning (external focus and differential learning, which are fully accessible in VR environments) may enhance current rehabilitation protocols and improve patient recovery.
In studies that utilized VR, it appears that participants’ attention was directed towards the goal of the movement, and positive outcomes were observed in terms of their movement patterns, suggesting a shift in participants’ focus from internal to external, which led to these positive changes as it was the only manipulated variable. Also, VR is a “distracting agent” that diverts attention and promotes external focus. The clinical significance of the present study is that motor patterns can be enhanced in patients after ACL reconstruction surgery using VR. Besides, VR appears to reduce internal focus, resulting in participants paying less attention to knee control. Reducing internal focus allows for more effective motor performance. To support this claim, we should mention the results of a recent study that utilized external focus instructions for single-leg jump testing during the return-to-sport phase. This approach was found to promote safer movement patterns compared to internal focus, thereby helping to reduce the risk of re-injury to the ACL. Participants in the external focus group demonstrated a greater range of motion and maximum knee flexion compared to the internal focus group, using both legs (31). Overall, incorporating externally-focused exercises in rehabilitation has the potential to increase its effectiveness and efficiency. It is recommended that future studies on VR and AR training programs should include long-term follow-up periods to assess the sustainability of their effects. Follow-up studies could determine the ideal duration or frequency of training sessions for sustained improvements. Comparisons between VR and AR training with traditional rehab methods for ACL injuries would help establish their relative advantages and limitations. Additionally, future research can develop protocols that adapt to the athlete’s needs, integrating real-time feedback and adaptive algorithms. Personalized VR/AR training can be a valuable approach to improve effectiveness. To enhance efficacy, optimizing VR/AR training variables such as intensity, duration, progression, and feedback is essential. Studying their impact on biomechanics, neuromuscular control, and psychology can improve rehabilitation outcomes. Furthermore, studying the combination of VR and AR training with other interventions like physical therapy, strength training, or cognitive-behavioral approaches can help optimize ACL injury prevention and rehabilitation protocols.
Integrating VR and AR training into real-world sports settings offers exciting potential for injury prevention and rehabilitation. Here are some practical considerations for integrating VR and AR training in real-world sports environments. In summary, to successfully implement VR and AR training programs, Ensure access to the necessary technical infrastructure, customize programs to align with athletes’ specific needs and sports demands, gradually increase the complexity and intensity of exercises, and integrate VR and AR as a complement to traditional training methods, focus on enhancing specific aspects like balance, coordination, and decision-making, combine VR and AR with on-field or gym-based training, use real-time audio and visual cues for immediate feedback, emphasize interactivity and engagement for athlete motivation and prioritize safety through warm-up, cool-down, and session duration regulation. The scoping review methodology, while valuable for providing an overview and identifying research gaps in a particular field, also has its limitations. Transparency and appropriate interpretation of findings require acknowledging limitations. Here are a few potential limitations associated with the scoping review methodology: Inclusion of studies, quality assessment, searching and selection process, data extraction and synthesis, and publication bias. It is important to note that these limitations are not unique to scoping reviews but are inherent to the methodology itself. Despite these limitations, scoping reviews are valuable in mapping the existing literature, identifying research trends, and informing future research directions.
Certainly, when considering the challenges and considerations for the implementation of VR and AR training in injury prevention and ACL rehabilitation for athletes, several factors need to be taken into account: Access and cost, training and familiarization, compatibility with existing rehabilitation protocols, ethical and psychological considerations and continuous evaluation and research. One of the primary challenges in implementing VR and AR technology in sports training is ensuring widespread access to the technology. Besides, VR and AR require specialized hardware and software, which can be expensive. The cost of acquiring and maintaining these technologies may pose a financial barrier for many individuals, clinics, or institutions. This can limit the accessibility of VR and AR training programs, particularly in resource-constrained settings. Affordability, availability, and potential funding sources should be considered to make these training programs accessible. Technical challenges, such as hardware setup, software integration, and system calibration, require technical expertise and support for successful implementation. Athletes and trainers need proper training and familiarization with VR and AR systems to ensure efficient usage. Individualized training programs should be designed to tailor to each athlete’s specific needs and goals, seamlessly integrating with existing rehabilitation protocols. Collaboration between healthcare professionals, coaches, and sports scientists is crucial for the seamless integration and continuity of care. Ethical considerations, such as obtaining informed consent and ensuring privacy, should be addressed, along with addressing the potential psychological impact on athletes. Continual evaluation and research are necessary to assess the effectiveness, long-term outcomes, and potential risks associated with VR and AR training. Collaborative efforts among stakeholders can provide valuable insights in refining the implementation process over time. Considering these challenges and considerations will aid in successfully implementing VR and AR training programs for injury prevention and ACL rehabilitation in athletes. By addressing these factors, practitioners can optimize the practical implications of these innovative technologies and improve athlete outcomes.
4.4. Conclusions
A key factor limiting the effectiveness of current injury prevention strategies is the failure to fully transfer learned motor patterns from intervention to sport (such as biomechanical coordination that reduces the risk of injury). Furthermore, recent evidence suggests that a neural deficit in the sensory-motor system underlies ACL injury. Still, current interventions do not target this neural activity nor promote the necessary neuroplasticity for transferring correct movement patterns to sport. However, recent research indicates that effective rehabilitation should teach athletes to move the learned motor skills from the clinic to the sports environment to prepare them for return to sport. Current research shows that after ACL surgery, patients exhibit altered movement patterns and different load distribution in the affected knee, even when deemed ready for return to sport. Comparing the movement patterns of these individuals with healthy individuals in VR fully supports this claim. Therefore, adding VR programs to clinical treatments and rehabilitation protocols may enhance motor learning assessment and recovery, which can help reduce the risk of secondary ACL injury factors.
Long-term impairments in performance and motor control, such as limb asymmetry, abnormal movements during landing and jumping, and decreased quadriceps muscle strength, indicate significant deficiencies in current rehabilitation strategies and hinder the return to play after ACL reconstruction. Furthermore, recent evidence suggests that after surgery, changes in the brain and spinal cord (negative neuroplasticity after injury) persist for years after treatment and return to sports (61).
Skeletal muscle injuries, especially ACL injuries, are structural disorders and involve damage to neural receptors, leading to disrupted afferent pathways and a form of negative and abnormal plasticity in the central nervous system (CNS). Patients after ACL surgery have reduced spinal reflexes and decreased motor cortex excitability.
Now is the time for a paradigm shift towards “brain training” in musculoskeletal rehabilitation. ANMT exercises may be beneficial for preventing ACL injuries and other painful musculoskeletal disorders (such as anterior knee pain) that result in changes in the structure and function of the central nervous system. Simple biofeedback interventions (e.g., adjusting visual and sensory information for each individual) may enhance preventive and rehabilitative interventions through neuroplastic mechanisms (45). However, three-dimensional assessment and innovative biofeedback training require specialized laboratories, which may limit the widespread dissemination of these approaches.
Functional magnetic resonance imaging (fMRI), VR for injury screening and pre-return-to-sport evaluation, and interactive neuromuscular training methods performed in AR or VR provide researchers and physicians with new approaches and tools to address this medical issue. The cost of accessing many of these technologies is gradually decreasing, and soon, such high-precision, data-driven assessment methods will be cost-effective and accessible to the majority.
4.5. Research Limitations
In most studies, the sample size was small, with only one gender and without a control/comparison group. The study did not investigate the potential of long-term biofeedback for learning, such as for 6 months, and did not include athletes in the ACL rehabilitation phase.