1. Background
Overweight and obesity are health risks resulting from a cumulative positive energy balance that slowly occurs over many years. The energy imbalance leads to life-threatening metabolic conditions, including atherosclerosis and diabetes (1). The prevalence of overweight and obesity is highest in middle and older people in both Western (2) and Asian countries (3-5). Despite this, incidences of overweight in children, adolescents, and young adults have progressively risen and should be of concern (2, 3, 6). NCD Risk Factor Collaboration (NCD-RisC) reported that between 1975 and 2016, there was a 10-fold increase in the number of girls with obesity and a 12-fold increase in the number of boys with obesity (7). A systemic review in 2018 demonstrated that 14.6% of 353,513 adolescents from Asian countries were overweight (8), while the prevalence of overweight and obesity in South Asian adults ranged from 22.4 to 52.4% (9). Interestingly, the cohort study in Australia also revealed that the proportion of overweight individuals increased from 20% in mid-adolescence to 33% at the age of 24 years (10). A recent study also reported a strong association between high Body Mass Index (BMI) and the risk of cardiovascular disease (CVD) in young obesity (11). Consequently, becoming overweight during early years can potentially lead to obesity development in middle age. Since the growth rate declines in young adults, body weight gain should be controlled. Overconsumption of calories and insufficient physical activity must be considered during this period (12-14). Reduction of calorie intake and adiposity with appropriate exercise is thus greatly recommended for this population (15, 16).
Many distinctive exercise training programs have been developed for weight management. Training at high intensity has been proven to increase the success rate of weight loss (17). High-intensity interval training (HIIT) is perceived to be very exciting (18) and yields a time-efficient effect when compared to a moderate-intensity continuous program (19). Unfortunately, HIIT is quite limited for persons at a high risk of musculoskeletal injuries and cardiopulmonary risk, including obese persons (20). For obese people, maximal exercise was intolerable compared to moderate-intensity exercise (21). Obese people also have a greater risk of musculoskeletal pain in the lower extremities (22, 23). Therefore, the chosen exercise must be developed to be suitable for obese persons. Recently, moderate-intensity interval training (MIIT) has been introduced, and its beneficial effect on improving blood lipids and cardiovascular functions in obesity has been confirmed (21, 24, 25). MIIT also provided weight loss in less time than moderate-intensity continuous training (26). With a lower intensity than HIIT, MIIT is expected to be friendly and accessible for all overweight people. However, little information is known regarding the effect of moderate-interval intensity exercise on physiological response.
2. Objectives
In the present study, we, therefore, aimed to evaluate the physiological alteration upon a single bout of MIIT exercise with overweight young adults. Participants with a BMI between 25 to 29.9 kg/m2 performed six-interval cycling alternated between three intervals of low-intensity exercise (20 - 40% of heart rate reserve) and three intervals of moderate-intensity exercise (50 - 60% of heart rate reserve). The low to moderate intensity duration ratio was 1: 1 (5 minutes in each interval). Changes in heart rate, oxygen consumption, and respiratory exchange ratio were recorded before and during exercise and upon recovery. Total energy utilization was then summarised. The relationship between heart rate and oxygen consumption was compared among exercise phases. In addition, we proposed that the physiological characteristics of MIIT exercise would initiate the appropriate exercise prescription in weight management for overweight and obese persons.
3. Methods
3.1. Participants
Participants were recruited through online advertisements. The inclusion criteria included young adults (18 to 25 years old) with a BMI between 25 to 29.9 kg/m2; waist circumference over 85 cm in males and over 80 cm in females; or percentage of fat mass more than 22% in males and 32% in females. Participants must have had a low physical activity level (insufficiently active) classified by the International Physical Activity Questionnaire – Short Form (IPAQ-SF). Exclusion criteria included smoking, having a clinical diagnosis of chronic diseases such as hypertension, diabetes mellitus, cancer, endocrine disorders, neurological disorders, heart disease, respiratory disease, kidney failure, severe orthopedic conditions, or other major health problems that may reduce safe cooperation in exercise.
Sample size was calculated by using G*Power program (version 3.1.9.4). According to previously published data (27), the effect size (f2) was 3.0 by using the regression of oxygen consumption versus heart rate as a primary outcome calculation. The total sample size calculation indicated 15 participants to yield a power of 0.95 in linear multiple regression: Fixed model, R square (r2) increase with a 5% significance level.
3.2. Study Design
A quasi-experimental design aimed to determine physiological responses during and after MIIT in overweight young adults. Oxygen consumption (V̇O2) and heart rate (HR) were monitored. The relationship between heart rate and oxygen consumption (HR-V̇O2) and respiratory exchange ratio (RER) were analyzed. The participants were informed regarding the aims, risks, benefits, and procedures, which conformed with the Helsinki Declaration. All participants were provided a written consent form before the beginning of the study procedures. The study protocol was approved by the Ethical Committee of Srinakharinwirot University (approval number: SWUEC/E-351/2565).
3.3. Anthropometric Measurements
Body weight and percentage of fat mass were measured by using a bioelectrical impedance analyser (MC-780 MA TANITA, Japan). Height was measured with a height measure ruler for adults, and waist circumference was measured with a measuring tape while participants were standing. All measurements were performed according to the manufacturer's instructions.
3.4. Determination of Exercise Intensity
Each participant first had their cycling intensity determined at their target heart rate for low and moderate intensities using the Astrand-rhyming cycle ergometer test (28). Participants were instructed to refrain from exercise for at least 2 hours and from caffeine for 24 hours before the test. The resting heart rate was measured before the test using the Karvonen formula to calculate the heart rate reserve. Their target heart rate ranges between 20 - 40% and 50 - 60% were calculated based on heart rate reserve. Then, participants were instructed to perform lower limb stretching for 10 minutes, followed by a 10-minute rest. After resting, participants performed cycling ergometry with a gradually increasing workload (50 watts every 3 minutes) until reaching their target heart rate range of moderate intensity. Participants rested for at least one hour before testing the MIIT protocol. Individual workloads at 20 - 40% and 50 - 60% of heart rate reserve were recorded and used for MIIT exercise. The Borg rating of 6 to 20 on the scale of perceived exertion was recorded during moderate exercise.
3.5. Measurement of Oxygen Consumption (V̇O2) and Heart Rate (HR)
Oxygen consumption and carbon dioxide production (V̇CO2) were measured throughout the experiment using a gas analyzer (Vmax® Encore system 29n, Viasys Health Care Inc.). Resting condition was recorded 5 minutes before the start of exercise. Parameters were recorded during 45 minutes of moderate-intensity interval protocol. Heart rate was monitored throughout the test by limb lead ECG. The relationship between heart rate and oxygen consumption was calculated using linear regression analysis.
3.6. Moderate-Intensity Interval Training (MIIT) Exercise Protocol
After resting for at least one hour, moderate-intensity interval exercise was started by a cycling ergometer (Monark 818E Ergomedic bike, Varberg, Sweden) for 45 minutes, followed by 30 minutes of recovery. The exercise protocol included a warm-up with no load for five minutes followed by six low and moderate-intensity alternations and then a cool down. Each exercise interval was performed for 5 minutes. After the warm-up, the workload was increased to reach 20-40% of heart rate reserve in the low-intensity session. Then, the workload was adjusted to reach 50 - 60% of the heart rate reserve for the moderate-intensity sessions. Participants alternately undertook three intervals of 5-minute low intensity and three intervals of 5-minute moderate intensity. Participants then received uncontrolled freeload cycling for 10 minutes as a cool down and sitting in a chair with armrests for 30 minutes in a recovery phase.
3.7. Statistical Analysis
Data was expressed as mean ± SD. SPSS Statistical software version 23.0 was used to perform the statistical analysis. The V̇O2-HR relationship was computed by linear regression analysis and represented by R square. Shapiro-Wilk test was used to test normal distribution. A normality of the distribution was found in this study. Moreover, the V̇O2-HR relationship was show as the mean of RER. For all analyses, a P-value less than 0.01 was considered statistically significant.
4. Results
4.1. Participant Characteristics
Fifteen young adult participants (8 males and 7 females) aged between 19 to 25 years old (male 20.9 ± 2.6 years; female 20.0 ± 2.2 years) who were overweight and had low physical activity levels voluntarily joined the study. Body mass index and waist circumference were characterized in males and females (Table 1). Resting oxygen consumption and the summative amount of oxygen consumption throughout the MIIT exercise period were also demonstrated, in which oxygen consumption was increased around threefold during the 45 minutes of workout protocol. The rate of perceived exercise (RPE) significantly increased at the first interval of moderate-intensity exercise (M1) compared to the warm-up and further increased during the second and third moderate intervals, respectively (Table 1). The increase in RPE seemed to be higher in the male group than in the female participants.
| Variables | Total (N = 15) | Male (N = 8) | Female (N = 7) |
|---|---|---|---|
| Age, y | 20.5 ± 2.4 | 20.9 ± 2.6 | 20.0 ± 2.2 |
| Body weight, kg | 78.2 ± 12.0 | 80.3 ± 9.9 | 75.9 ± 14.6 |
| Height, cm | 168 ± 8 | 173 ± 6 | 162 ± 6 |
| BMI, kg/m2 | 27.6 ± 3.0 | 26.7 ± 2.1 | 28.6 ± 3.7 |
| Waist circumference, cm | 91.9 ± 7.1 | 94.4 ± 4.9 | 89.1 ± 8.6 |
| Percentage of fat mass, % | 32.4 ± 10.4 | 24.7 ± 5.7 | 41.2 ± 6.5 |
| Fat-free mass, kg | 52.5 ± 9.4 | 60.1 ± 4.8 | 43.9 ± 4.0 |
| Resting heart rate, beats/min | 86.8 ± 8.6 | 85.5 ± 7.7 | 88.2 ± 9.9 |
| Resting V̇O2, l/min | 0.180 ± 0.104 | 0.192 ± 0.088 | 0.166 ± 0.126 |
| Summative V̇O2 during MIIT and cool down, l/45 min | 25.1 ± 8.1 | 27.4 ± 7.9 | 22.5 ± 8.1 |
| RPE Warm-up | 7.40 ± 1.55 | 7.63 ± 1.51 | 7.14 ± 1.68 |
| RPE M1 | 13.1 ± 2.4 | 14.1 ± 2.4 | 12.0 ± 2.1 |
| RPE M2 | 13.9 ± 2.1 | 14.9 ± 1.6 | 12.9 ± 2.1 |
| RPE M3 | 14.9 ± 2.4 | 16.5 ± 1.6 | 13.1 ± 1.8 |
Abbreviation: BMI, Body Mass Index; V̇O2, oxygen consumption; V̇O2max, maximal oxygen consumption; M1, 1st moderate intensity; M2, second moderate intensity; M3, 3rd moderate intensity; RPE, rate perceived exertion was measured by the original category scale (6 to 20 scale).
a Values are expressed as Mean ± SD.
4.2. Effect of MIIT Exercise on Heart Rate
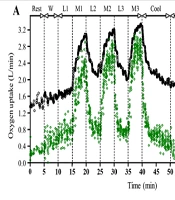
Figure 1 is representative data of changes in heart rate and oxygen consumption upon MIIT exercise. Heart rate was slightly increased during warm-up and further increased during the first low-intensity exercise (L1). Following moderate-intensity exercise (M1), the heart rate gradually raised and hit the target heart rate as calculated (Table 2). Upon shifting to low intensity, the heart rate dropped but did not completely return to the heart rate zone throughout 5 minutes in both the second (L2) and the third low-intensity exercise (L3). Interestingly, the peak heart rate found during the second moderate intensity (M2) was higher than the peak of the first moderate-intensity exercise (M1). Moreover, with the same workload, the peak heart rate of the third moderate-intensity exercise (M3) raised beyond the desired target heart rate zone in both male and female participants (Table 2). This finding suggests that the MIIT exercise protocol in this study activated more effort in overweight persons than expected from the volume load. During the cool-down period, the heart rate gradually decreased. However, the level after 10 minutes was still significantly higher than levels during L1. The percentage of heart rate recovery after one minute was 16.2 ± 5.1% in all participants.
A, scatter plot of HR (black) and V̇O2 (green) for a participant during MIIT to recovery. Low-intensity workloads at 20 - 40% and moderate-intensity workloads at 50 - 60% of heart rate reserve with HR and V̇O2 were recorded throughout the experiment; B, scatter plot of V̇CO2 for a participant during exercise. Abbreviations: W; warm up, L1; 1st low intensity, M1; 1st moderate intensity, L2; 2nd low intensity, M2; 2nd moderate intensity, L3; 3rd low intensity, M3; 3rd moderate intensity, Cool; cool down.
| Variables | Total; (N = 15) | Male; (N = 8) | Female; (N = 7) |
|---|---|---|---|
| Target heart rate zone during low intensity, beats/min | 106 - 129 | 104 - 128 | 108 - 131 |
| Target heart rate zone during moderate intensity, beats/min | 141 - 153 | 140 - 152 | 143 - 154 |
| Highest heart rate at M1, beats/min | 149 ± 9 | 149 ± 11 | 150 ± 8 |
| Highest heart rate at M2, beats/min | 155 ± 7 | 155 ± 10 | 155 ± 3 |
| Highest heart rate at M3, beats/min | 163 ± 10 | 163 ± 13 | 162 ± 5 |
| Percentage of HRR at 1 min, % | 16.2 ± 5.1 | 18.4 ± 3.5 | 13.6 ± 5.6 |
Abbreviation: M1, 1st moderate intensity; M2, 2nd moderate intensity; M3, 3rd moderate intensity; HRR, heart rate recovery; V̇O2, Oxygen consumption.
a Values are expressed as Range or Mean ± SD.
4.3. The Effect of MIIT on V̇O2 and V̇CO2
Figure 1 also demonstrated changes in V̇O2 and V̇CO2 during the MIIT exercise. V̇O2 increased gradually during the warm-up and the first interval of low-intensity exercise (L1). At the first moderate intensity interval (M1), V̇O2 markedly raised 3 to 4-fold of L1 and then dropped suddenly in the second low intensity (L2). Unlike heart rate, V̇O2 during L2 almost completely returned to the same level detected during L1. Similar to the change in heart rate, peak V̇O2 in the second (M2) and the third moderate-intensity exercise (M3) became higher than the first (M1), respectively. V̇O2 then suddenly decreased and approached near the resting levels within 10 minutes of the cool-down period. The percentage of V̇O2 recovery after one minute was 27.7 ± 10.6% in all participants.
Similar to the V̇O2 response, V̇CO2 changed similarly (Figure 1B). V̇CO2 markedly increased during moderate-intensity exercise and immediately declined upon changing to low-intensity exercise. Peak V̇CO2 slightly increased in the second and third intervals of moderate-intensity exercise, respectively. Interestingly, the rate of V̇CO2 decline upon switching from moderate to low intensity was slower than that of the rate of V̇O2 decline, in which the V̇CO2 during the second and the third intervals of low-intensity exercise did not completely return to the same level of the first interval (L1). V̇CO2 rapidly reduced to the resting levels at the end of the cool-down period.
4.4. Oxygen Consumption-Heart Rate Relationship
To determine whether the change in heart rate indicates a change in oxygen consumption during MIIT exercise, the relationship between oxygen consumption and heart rate was calculated based on linear regression analysis. The total R square (r2) was 0.761 ± 0.090. Additionally, the r2 and beta coefficient were separately calculated among three phases of low-intensity exercise (L1, L2, and L3), three phases of moderate-intensity exercise (M1, M2, and M3), and the cooldown (Table 3). The results demonstrate that the r2 of the V̇O2-HR relationship during low-intensity exercise was lower than during moderate-intensity exercise and cooldown. This difference could be due to the lower rate of heart rate decline than the rate of V̇O2 decline during low-intensity exercise.
| Variables | R square; (N = 15) | Beta coefficient; (N = 15) | RER; (N = 15) |
|---|---|---|---|
| Combined low intensity 15 min | 0.549 ± 0.161 | 0.016 ± 0.018 | 1.04 ± 0.09 |
| Combined moderate intensity 15 min | 0.658 ± 0.105 | 0.016 ± 0.004 | 1.06 ± 0.07 |
| Cool down for 10 min | 0.643±0.190 | 0.018±0.005 | 1.04 ± 0.11 |
a Variables are expressed as Mean ± SD.
4.5. The Effect of MIIT on Respiratory Exchange Ratio
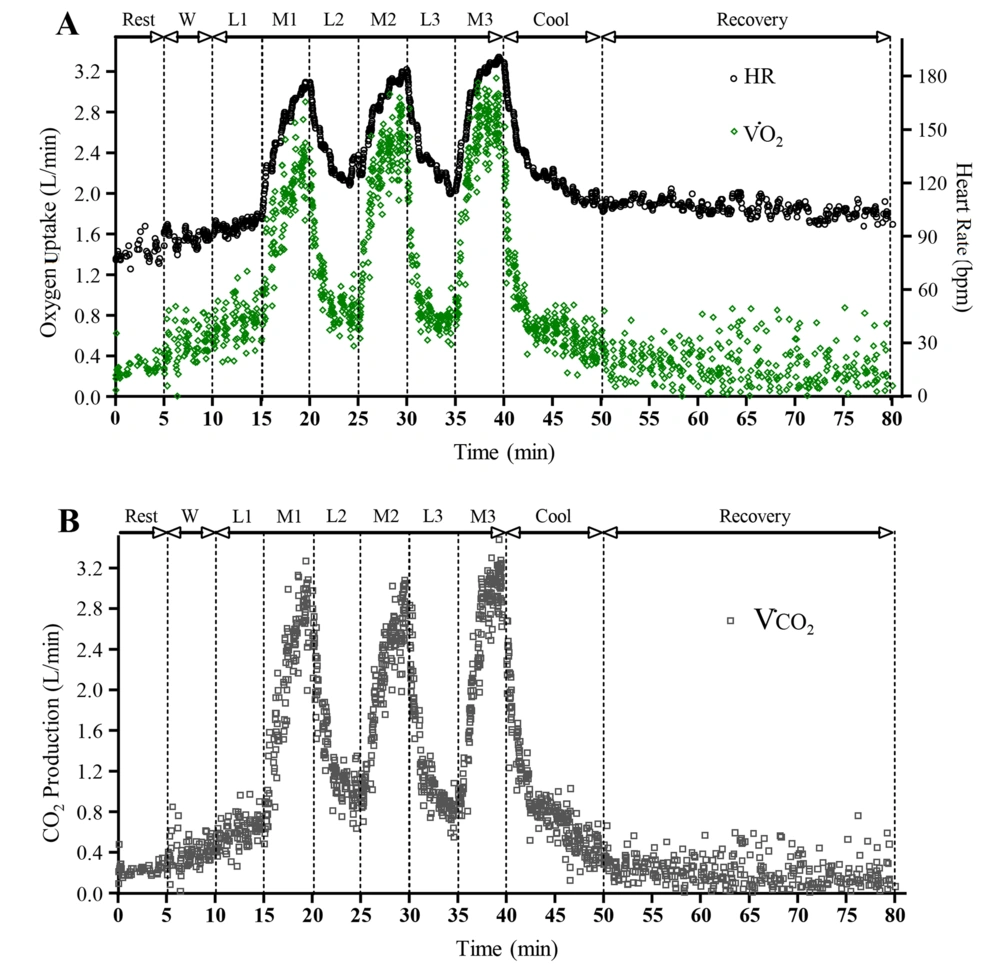
The characteristics of changes in Respiratory Exchange Ratio (RER) during moderate-intensity interval training are shown in Figure 2A and B. The RER of the 15 participants was 0.826 ± 0.094 in the resting state. RER was slightly increased to the end of the first low intensity (L1) and raised during the first moderate intensity interval (M1). All participants' peak RER during the first interval of moderate-intensity exercise was 1.48 ± 0.35. Unexpectedly, RER kept increasing in the second low intensity (L2) for a few minutes. RER immediately declined upon shifting to the second moderate intensity interval (M2) before increasing again. The overshoot of RER, once returned to low-intensity exercise, was found again at the third interval (L3) and cooling down. Lastly, the overshoot of RER gradually decreased during the cool-down to the resting level at a recovery state.
Scatter plot of respiratory exchange ratio during MIIT to recovery in the example of male (A); and female (B) participants. The ratio between V̇CO2 and V̇O2 were analyzed the respiratory exchange ratio during the experiment as shown in the V̇O2 - V̇CO2 relationship of male (C); and female (D) during MIIT exercise for 30 min (from L1 to M3).
The relationship between V̇O2 and V̇CO2, represented by the slope, is shown in Figure 2C and D for males and females, respectively. The total slope of all participants was 1.06 ± 0.07. There was no significant difference in graph slope between low and moderate intensities (1.05 ± 0.124 and 1.05 ± 0.084, respectively).
5. Discussion
The present study aimed to evaluate the cardiorespiratory responses during moderate intensity-interval exercise in overweight young adults. We proposed that MIIT could be the starting program for overweight and obese persons to increase energy utilization and reduce weight gain. To the best of our knowledge, the present study is the first to examine the effects of MIIT on cardiorespiratory in overweight young adults. The results demonstrate that the 45-min MIIT exercise protocol consumed 25.1 ± 8.1 L, equal to approximately 530 ± 171 kJ (1 L of V̇O2 = 21.1 kJ). As expected, heart rate, V̇O2, and V̇CO2 increased during moderated-intensity exercise and declined during low-intensity exercise. A low to moderate duration ratio of 1:1 was sufficient to return both V̇O2 and V̇CO2 to their stage level. However, the rate of change was different among them, in which rates of heart rate and V̇CO2 decline were slower than the rate of V̇O2 decline. Although there was a very linear relationship between V̇O2 and heart rate for the overall period, the correlation was less when selectively computed during low or moderate exercises. This finding suggests that changes in heart rate during interval exercise may not truly reflect the change in oxygen consumption. A greater increase in heart rate and V̇O2 in the second and third intervals of moderate exercise than in the first interval suggested more cardiorespiratory demand in the following intervals. Additionally, RER being larger than one indicated the possibility of high acid accumulation during exercise, in which the rate of carbon dioxide production was higher than the rate of oxygen consumption.
In practice, heart rate has been used as a simple indicator of aerobic exercise intensity. Overall, all participants demonstrated a closed relationship between V̇O2 and heart rate. However, the correlation reduced when derived only during low or moderate-intensity interval exercise. This change might be the effect of exercise transition from low to moderate intensity or moderate to low intensity (29, 30). The correlation during transition exercise is lower than steady-state conditions in overweight young adults, and this result was also reported in healthy persons and athletes (29). Since the MIIT exercise comprised many transition periods, the prediction of oxygen consumption from the average V̇O2-HR relationship might not be valid. The possible mechanism of difference in the V̇O2-HR relationship during exercise transition could be due to excess sympathetic stimulation even in the low intensity of the exercise period. A previous study demonstrated that an increased low-to-high-frequency ratio (LF/HF) of heart rate variability (HRV), indicating sympathetic dominance, was found after high-intensity interval exercise but not in continuous exercise (31). Excessive sympathetic stimulation could delay the heart rate decline during low-intensity exercise intervals.
RER is generally indicated as the source of energy utilization. An increase in RER during exercise indicates an increase in carbohydrate utilization, while RER greater than one suggests anaerobic respiration (32). A high level of RER during M1 indicates that overweight persons thus used anaerobic energy during moderate-intensity exercise derived from maximum heart rate. Moderate intensity of exercise leads to the accumulation of acid and carbon dioxide. This finding suggests that MIIT exercise could be strenuous for overweight beginners. The increase in RPE in the last interval also supported this implication. Similar to our finding, an acute effect of MIIT, but unequal interval (3 min: 2 min × 5 intervals) increased both RPE and muscle pain scores at later intervals (33). Notably, the strength pattern of RER change during exercise transition, either from low to moderate intensity or from moderate to low intensity, could need to be more reliable to indicate the source of energy utilization. The time lag between the rate of change in oxygen consumption versus the change in carbon dioxide production might cause that unusual pattern. The HIIT protocol also reported a similar finding (34).
Many previous MIIT studies in overweight young adults mostly reported the effects of long-term exercise (24, 25, 35). However, the MIIT protocol used in their study was varied. Racil et al., in 2013, studied short sprint MIIT (work: rest: 30 sec: 30 sec × 6 to 8 sessions for 12 weeks) and reported that the MIIT program could reduce the percentage of body fat and enhance peak oxygen consumption (24). Another progressive MIIT, by increasing exercise duration (15 sec:15 sec with 4 to 8 min × 3 sessions for 12 weeks), also decreased the percentage of body fat and increased maximal oxygen uptake (35). Another group of investigators reported that the maintained MIIT protocol (1 min :1 min × 5 intervals, twice a week, for 12 weeks) significantly increased maximal oxygen uptake but showed no difference in total fat after 12 weeks (25). The total exercise duration, then, must be a factor affecting the fat burn. We then speculated that our present protocol used in the study was high enough to lose body fat and improve oxygen consumption in long-term training.
A previous study revealed that females appear to be more resistant to fatigue and have a faster ability to recover during repeated bouts of HIIT sessions (36), in which the interchangeability of HIIT protocols between males and females must be reconsidered. This suggests that females have a significantly lower rate of perceived exertion than males during MIIT exercise. Nevertheless, besides the rate of perceived exertion, cardiorespiratory responses to the MIIT protocol were similar. Therefore, the present protocol can be identical for overweight males and females. Unfortunately, the small sample size in male and female subgroups limited the statistical power to confirm the significant difference in gender comparison. Thus, further investigation regarding the effects of MIIT on males and females is interesting.
5.1. Limitation of Study
The present study aimed to observe only the cardiovascular response to a single bout of MIIT exercise. First, no other protocols, such as continuous exercise at moderate intensity, were performed in comparison. The result was that RER rises more than once within five minutes of exercise, and participants might be too exhausted to keep moderate exercise for more than ten minutes in actual practice. Second, since the study was curious about an exercise protocol for overweight and obese populations, the effect of MIIT bout in the average weight population was not the target. Third, the exercise mode in the present study was cycling ergometry, which is less affected by body weight. The response might be affected if the study was performed with body weight-dependent exercise such as running. Lastly, our results suggest a potential effect after only one MIIT session, and whether these responses would be repeated regularly remains to be determined. A long-term study could inform those responsible for designing and implementing physical activity interventions for overweight populations.
5.2. Implication of Finding
The present study aimed to evaluate the cardiopulmonary response to MIIT exercise bout in young adult overweight persons. We expected to verify whether the MIIT protocol used in this study is suitable or not for young adult overweight persons as a beginner. According to potential MIIT protocol limitations in which the 1: 1 ratio of moderate to low-intensity intervals induced a potentially excessive anaerobic response (RER > 1.0) to vigorous intensity (RPE > 12) (37), the exercise protocol must be accommodated for them. The shorter period of moderate intensity and/or the longer period of low intensity was suggested at the beginning of the program. Therefore, increasing the time of moderate intensity interval while shortening the time of low-intensity interval can be the exercise progression.
5.3. Conclusions
The present study revealed cardiorespiratory change during 45 minutes of MIIT exercise in low-active, overweight persons, which burns approximately 100 kcal. Cardiovascular effort was higher after repeat intervals, resulting in more physiological stress in both males and females. Like a high-intensity interval, MIIT exercise activated anaerobic metabolism but was less aggressive. Therefore, MIIT could be a suitable starting exercise protocol for all overweight persons.