1. Context
At the end of the 20th century, dysfunction of the transversus abdominis (TrA), a deep-local-abdominal muscle of the core, was linked to insufficient muscular stabilization of the lumbar spine (1). As a result, retraining of the TrA was recommended for lumbopelvic stabilization using the abdominal hollowing maneuver (AHM), also known as the abdominal drawing-in maneuver (ADIM) (2, 3). Since then, several studies have supported the benefits of ADIM for lumbar stabilization and core strengthening (4), enhancing TrA activity (5-8), selectively strengthening TrA (9), improving lumbopelvic stability (10, 11), and enhancing overall body stability (12).
Although some papers emphasize that ADIM, which selectively activates local core muscles and increases the activation ratio between local and global core muscles, improves pelvic stability (13, 14), other studies suggest that global muscle coactivation techniques, like the abdominal bracing maneuver (ABM), are more effective for controlling trunk stability (15, 16). Proponents of global muscle activation argue that all core muscles contribute to stability and that focusing on isolated activation of one muscle, such as the TrA, may hinder overall function. Those supporting ADIM maintain that the TrA is the cornerstone of lumbopelvic stability, but this viewpoint has been contested by others who do not believe that one muscle is more important than others for core stability (17, 18).
The objective of ADIM is to activate deep-local-abdominal muscles with minimal global muscle activation (16). Electromyography studies show that ADIM decreases rectus abdominis (RA) activation (a global core muscle) while increasing TrA activation (16, 19, 20), indicating a competitive relationship between the two. However, during high-load tasks (HLT) like the "Front Plank" or "Double Leg Raise," global muscle EMG input is greater than local muscle input (21), highlighting the importance of global muscles in providing stability during HLT. For instance, during the high-load Pilates exercise "Leg Pull Front," ADIM was less effective in controlling pelvic rotation (22). While local core muscles are essential for lumbopelvic stability, they are insufficient for controlling the orientation of the spine. In contrast, RA plays a critical role in controlling anterior pelvic tilt and transmitting loads from the thorax to the pelvis (23). With its large lever arm, RA is considered the most important muscle for correcting lumbar lordosis (24) and is crucial for increasing intra-abdominal pressure (IAP), which helps unload the spine (25) and support spinal extension (26, 27). RA also controls pelvic orientation when the thorax is fixed (28, 29). Therefore, reducing RA activity by favoring TrA through ADIM may negatively affect core stability during HLT.
In contrast, some authors argue that the body naturally selects an appropriate muscle activation pattern to achieve sufficient spinal stability, and conscious adjustments to this natural activation may reduce the safety margin of stability (30). Some studies even suggest that interventions without conscious muscle activation stabilize the core more effectively than those involving conscious activation (31, 32).
Given this ongoing debate—some advocating for ADIM and others against it—there is still a lack of clarity about its efficacy, particularly during HLT. We previously hypothesized that ADIM should not be used when training core stability and strength in high-load scenarios due to the excessive activation of TrA and the resulting inhibition of global core muscles like RA, which is crucial for pelvic directional control (33). This leads to the central question: Could ADIM impair core stability function during HLT? Despite concerns from top trainers in strength conditioning and weightlifting who believe that "the more strongly your abdominals are pulled in, the less stable your trunk can be during lifting" (34), no study has systematically analyzed the effectiveness of ADIM considering the load criterion used in tasks or exercises.
2. Objectives
Consequently, the main objective of this article is to systematically review the relevant literature to evaluate the effectiveness of ADIM compared to not using ADIM for stabilizing the core during various tasks or exercises. These tasks will be analyzed based on the load used, following the high- and low-load classification criteria established by Mottram and Comerford (35). Also, we will assess the impact of ADIM on core stability by examining the type of perturbation that challenges core stability and the exercise position used during the task.
3. Data Sources
3.1. Search Strategy
The literature was obtained through a systematic search in the PUBMED databases, covering the period from January 1981 to March 31, 2024. The review adhered to the PRISMA checklist. The search terms included the following keywords, combined as indicated: Abdominal drawing-in, abdominal hollowing, abdominal drawing-in + lumbo-pelvic stability, abdominal drawing-in + core stability, abdominal hollowing + lumbo-pelvic stability, abdominal hollowing + core stability, abdominal hollowing + abdominal bracing, pilates + core stability, pilates + lumbopelvic stability. The term Pilates was included because ADIM is commonly used within Pilates practice (36).
3.2. Study Selection and Eligibility Criteria
The main question was whether using ADIM versus not using ADIM could improve core stability during various tasks. Studies were eligible for inclusion if they met the following criteria:
(1) Manuscripts that involved a comparative study of interventions using tasks or exercises with ADIM, compared to interventions using the same tasks or exercises without ADIM or with another abdominal activation maneuver.
(2) Only studies that included a kinematic assessment were included.
Inclusion and exclusion criteria were based on specific insights. Much of the literature relies on EMG or muscle thickness analysis to assess core muscles. Studies correlating EMG activity to stability suggest that increased muscle activity leads to improved stabilization. However, some studies show no correlation between muscle activity and pelvic stability (22, 31), indicating that EMG may not be directly linked to function. Electromyography information alone does not reveal whether muscles contract concentrically, eccentrically, or isometrically, leaving us uncertain about whether joint segments are stable or moving. This limitation means that EMG data, while important, does not provide a complete picture. For instance, some studies suggest that ADIM selectively activates the TrA but is less effective for pelvic stabilization (22). Therefore, studies using only EMG or thickness analysis without kinematic assessment were excluded.
Other articles employ within-subject repeated-measures design protocols that compare pre- and post-training program results. However, these studies do not compare interventions using ADIM versus those without ADIM. For instance, Saiklang et al. demonstrated an evident improvement in sitting posture and a decrease in muscle fatigue after an exercise program incorporating ADIM (37). In this exercise program, participants not only performed ADIM exercises in prone and supine positions but also trained in a sitting position while being instructed to maintain a neutral alignment of the pelvis and spine. It is unclear whether the improvements in posture and muscle fatigue resulted from ADIM itself or from the postural guidance and training sessions.
On the other hand, some studies compare intervention programs that involve entirely different exercises, movement patterns, and stimuli. For example, Puntumetakul et al. compared the effects of core stabilization exercises with ADIM to general strengthening exercises (38). The group practicing core stabilization with ADIM performed the drawing-in maneuver in various positions, such as sitting, supine, four-point kneeling, and standing, all with neutral lumbar spine and pelvis alignment. In contrast, the general strengthening exercises group engaged in exercises involving spinal flexion and extension, such as full abdominal crunches and back extensions on a Swiss ball. Sagittal translation of L4-L5 and L5-S1 was evaluated using X-rays in positions of full flexion and extension of the spine.
In such cases, it is difficult to determine whether the change in lumbar vertebrae sagittal translation was due to the absence of ADIM or the flexion and extension exercises performed. These studies do not allow for a direct comparison of interventions because they evaluate entirely different exercises, joint positions, movement patterns, and goals. As a result, it cannot be concluded whether the outcomes of exercise programs with ADIM were due to ADIM itself or the specific movement characteristics of the exercises performed. Therefore, studies that did not compare interventions using the same exercises or tasks with and without ADIM were excluded.
3.3. Data Extraction and Quality Assessment
A single reviewer conducted the study selection and data extraction. The review process focused on extracting the following information: (a) description of the exercises and tasks evaluated; (b) type of load imposed on the subject; (c) objective of the kinematic assessment; (d) postural or joint alignment requirements; (e) type of abdominal activation maneuver; (f) the main conclusion of each study regarding which intervention conditions were best for improving core stability.
All this information is summarized in Table 1. Due to the heterogeneity of study designs, assessment methodologies, and statistical analyses, the results are presented descriptively. This review did not analyze the quality of the included studies; instead, the objective was to compile the conclusions drawn from these studies to calculate the success rate of each intervention.
| Study | Task or Exercise | Type of Load | Objective of the Kinematic Assessment | Postural Requirements Specified for the Intervened Groups | Types of Abdominal Activation Maneuver | Intervention with Better Results: ADIM, Vs, OC |
|---|---|---|---|---|---|---|
| Jeong and Chung (39) | Effect of a task-oriented training in sitting position | LLT | Trunk control, balance functional reaching test, Berg Balance Scale | Task-oriented training combined with ADIM was instructed to maintain pelvis in a neutral position. | ADIM, Vs, no activation | ADIM |
| Park et al. (32) | Prone hip extension | LLT | Pelvic anterior tilting and rotation angles | ADIM, Vs, no activation | OC, (no activation) | |
| Ko et al. (40) | Prone knee flexion | LLT | Pelvis rotation | ADIM, Vs, no activation | ADIM | |
| de Oliveira et al. (41) | legged and semi-tandem stances on force platform. | LLT | Trunk postural control | ADIM, Vs, no activation, Vs, orthosis | Inconclusive | |
| Kadri et al. (42) | Semi-tandem and unipodal balance | LLT | Center of pressure parameters | ADIM, Vs, no activation, Vs, orthosis | Inconclusive | |
| Saiklang et al. (43) | Sitting | LLT | Stature change | Both groups were asked to sit in neutral sitting posture. | ADIM, Vs, no activation | ADIM |
| Larivière et al. (44) | Standing plus trunk sudden perturbations | HLT | Lumbar stiffness | ADIM, Vs, ABM | OC (ABM) | |
| Lee and Lee (12) | Bridging exercise | LLT | Tetrax© standing balance test | ADIM, Vs, no activation | ADIM | |
| Jeon et al. (45) | Prone hip extension | LLT | Lumbopelvic kinematic: Anterior tilting and rotation | ADIM, Vs, no activation | ADIM | |
| Southwell et al. (46) | Unloaded slow repetitive spine flexion reaching task. | LLT | Spine stability during dynamic movement | ADIM, Vs, no activation | ADIM | |
| Madokoro et al. (47) | Forward step | LLT | Pelvic tilt and rotation | ADIM, Vs, no activation | ADIM | |
| Park et al. (48) | Prone knee flexion | LLT | Pelvic tilt and pelvic rotation | ADIM, Vs, no activation | ADIM | |
| Oh et al. (49) | Prone hip extension | LLT | Angle of anterior pelvic tilt | ADIM, Vs, no activation | ADIM | |
| Jung and Oh (22) | Leg pull front pilates exercise | HLT | Angle of pelvis rotation | ADIM, Vs, ABM, Vs, no activation | OC (ABM) | |
| Oh et al. (50) | Sudden perturbation seated in a chair | HLT | Thorax stability, pelvis stability | ADIM, Vs, ABM, Vs, no activation | OC (ABM), for thorax stability; ADIM, for pelvis stability; Inconclusive | |
| Lee et al. (51) | Gait ability | HLT | Timed Up and go test. 10-meter walk test. Berg Balance Scale. Functional reach test | ADIM, Vs, ABM | Inconclusive | |
| Balance ability | LLT | |||||
| Kim and Kim (15) | Side-lying hip abduction | LLT | Pelvis lateral rotation | ADIM, Vs, ABM, Vs, no activation | OC (ABM) | |
| Kim et al. (52) | Standing body sway control during sudden perturbation | HLT | Angular displacements of the trunk | For ADIM and ABM groups: Maintaining the lumbar spine in a neutral. For no activation group: No specific instructions | ADIM, Vs, ABM, Vs, no activation | ADIM = ABM, Inconclusive |
| Suehiro et al. (11) | Prone hip extension | LLT | Spine motion | ADIM, Vs, ABM, Vs, no activation | ADIM = ABM, Inconclusive | |
| Butler et al. (31) | Standing lift of 3.8 kg load in normal reach | LLT | Pelvis rotation angle; lumbar angle | ADIM, Vs, no activation | OC, (no activation) | |
| Standing lift of 3.8 kg load in maximum and extreme reaches | HLT | |||||
| Vera-Garcia et al. (16) | Sudden perturbation in semi-seated position | HLT | Lumbar displacement | ADIM and ABM groups: Lumbar spine in a neutral position | ADIM, Vs, ABM, Vs, no activation | OC (ABM) |
| Grenier and McGill (53) | In-vivo: (1) 10 Kg load in both hands, (2) no load, (3) right-hand load, and (4) left-hand load. Spine model | HLT | Lumbar Stability | The testing was performed in an anatomically neutral standing posture. | ADIM, Vs, ABM | OC (ABM) |
| Lee (14) | Flat, round and extended back knee stretch exercise using a pilates reformer | LLT | Pelvic stability and trunk stability | Flat back: Neutral pelvis; round back: Posteriorly tilted pelvis; extended back: Anteriorly tilted pelvis | Experienced pilates practitioners (ADIM), Vs, non-experienced participants, (no activation) | ADIM |
| Fayh et al. (54) | Long stretch pilates exercise using a pilates reformer | HLT | Pelvis stability | ADIM group: The activation included a imprint technique (slight posterior tilted pelvis) | ADIM, Vs, no activation | ADIM |
Information Extracted from Each of the Included Studies
4. Results
4.1. Search Results
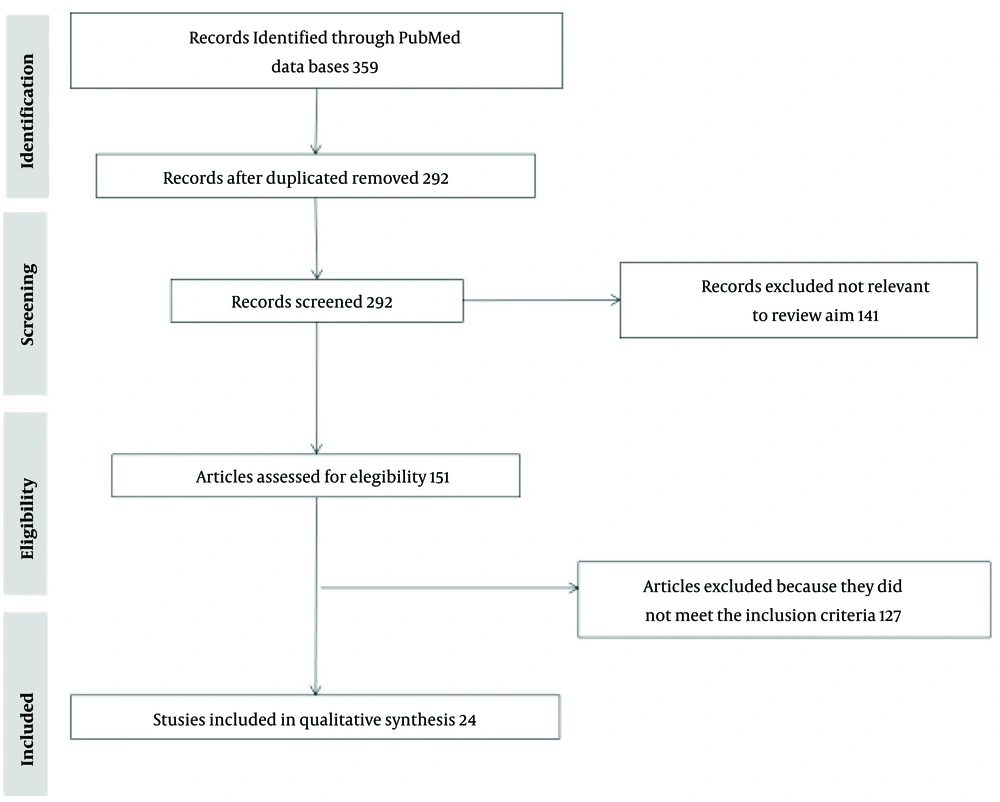
The search results are summarized in Table 2, which displays the outcomes based on each keyword combination. The literature search returned a total of 359 studies. After removing 67 duplicate studies, we reviewed the titles and abstracts of 292 remaining articles. Of these, 151 full-text articles were selected for screening. Based on our inclusion and exclusion criteria, 24 studies were included in the final review. The selection process is summarized in Figure 1.
| Keywords | = | + Lumbopelvic Stability | + Core Stability | + Abdominal Bracing | Values |
|---|---|---|---|---|---|
| Abdominal drawing-in | 157 | 9 | 12 | - | 178 |
| Abdominal hollowing | 92 | 3 | 8 | 32 | 135 |
| Pilates | - | 8 | 38 | - | 46 |
| Total | 359 |
Search Results According to Each Keyword and its Combinations
4.2. Task Analysis
To draw clear conclusions from the extracted data, only studies with conclusive results were included in the statistical analysis. Studies were classified as inconclusive (a) if they were described as such by the authors; or (b) if different interventions produced the same outcome. For example, Oh et al. (50) reported divided conclusions, so their study was categorized as inconclusive. Among the 24 included studies, 26 tasks were extracted, with 19 yielding conclusive results. Table 3 presents a description of each task with conclusive results, as well as the kinematic assessment methods used.
| Study | Task or Exercise Description | Types of Measurements Extracted from Kinematic Analysis, and, Kinematic Measurement Methods | Intervention with, Better Results |
|---|---|---|---|
| Jeong and Chung (39) | Effect of a 5 weeks task-oriented training in sitting position. The training tasks were: Arm reaching, ring stacking, and ball kicking. They were performed in a sitting position at a table with a straight back, both feet on the floor, and knee joint and hip joint angles maintained at 90 degrees. | Trunk control: Trunk Impairment Scale and the Postural Assessment Scale for Stroke, balance ability: Functional reaching test. Berg Balance Scale, and the Messen–Trainieren–Dokumentieren system, activities of daily living: Modified Barthel Index. | ADIM |
| Park et al. (32) | Prone hip extension: Participants lay in a prone position with the trunk and lower extremities supported on a table. Each participant was asked to slowly lift the dominant leg straight off the table surface into hip extension until they reached an end-range hip extension position designated by the target bar. | Pelvic anterior tilting and rotation angles: Three-dimensional electromagnetic motion analysis system. (Liberty; Polhemus; Colchester, VT, USA) | OC, (no activation) |
| Ko et al. (40) | Prone knee flexion: The participants were asked to assume a prone position on the treatment table, they actively flex the knee joint toward the buttocks as possible for each of two tibial rotation conditions. | Pelvis rotation: Smartphone inclinometer application | ADIM |
| Saiklang et al. (47) | Sitting for stature: 41 minutes sitting test in a neutral sitting posture | Stature change: Seated stadiometer device | ADIM |
| Lee and Lee (12) | Effect of 4 weeks training of Bridging exercise: From a crook lying position, according to the command of “pelvis up”, the participants raised the pelvis and maintained the raised pelvic position. | Tetrax© Standing Balance test | ADIM |
| Jeon et al. (45) | Prone hip extension: Each subject supported his trunk on the table with his pelvis at the edge of the table. During the initial phase of the exercise, the lumbar spine was positioned neutrally by adjusting the pelvis according to the subject’s height using the surface level. The subject was instructed to slowly lift his dominant leg without knee flexion until he reached the target bar. When the hip joint was extended to 5º and the leg touched the target bar, this position was maintained for 5 s. | Lumbo pelvic kinematic: Anterior tilting and rotation. Electromagnetic tracker system. polhemus liberty™ | ADIM |
| Southwell et al. (46) | Unloaded slow repetitive spine flexion reaching task: From a standing position, each participant performed two trials of 35 cycles of repetitive unloaded spine flexion with a constrained pelvis to the beat of a metronome at a rate of 15 cycles/min. | Spine stability during dynamic movement: Visual-3D (C-Motion Inc, USA), only 3D lumbar spine kinematics were analyzed | ADIM |
| Madokoro et al. (47) | Forward step. Measurements were performed in the forward step posture with the right foot. | Spine stability during dynamic movement: 3-dimensional motion analysis system (Vicon motion systems) | ADIM |
| Park et al. (48) | Prone knee flexion: The subject was asked to perform prone knee flexion comfortably. | Pelvic tilt and pelvic rotation: Three-dimensional ultrasonic motion analysis system, CMS-HS. | ADIM |
| Oh et al. (49) | Prone hip extension: The subject assumed a prone position on a therapeutic table with the upper trunk, pelvis, and lower extremities aligned in a straight line. The head was allowed to extend slightly to maintain normal breathing. The subject was asked to perform hip extension, with the dominant lower extremity in the prone position, to a predetermined target bar. | Angle of anterior pelvic tilt: Three -dimensional ultrasonic motion analysis system (CMS-HS; Zebris Med izintechnik GmbH, Isny im Allgau, Ger many) | ADIM |
| Kim and Kim (15) | Side-lying hip abduction: The subjects were asked to lie on a treatment table with a non-dominant leg against the table while straightening the trunk, pelvis, and the dominant leg. For the non-dominant leg on the table, the hip joint was bent at 45° and the knee joint was bent at 90°. With a goniometer and a target bar, the subject’s hip joint abduction angle was set at 25°. | Pelvis lateral rotation: 3-dimensional motion analysis system (CMS 70P, Zebris Medizintechnik GmbH, Isny im Allgäu, Germany) | OC (ABM) |
| Butler et al. (31) | Standing lift of 3.8 kg load in normal reach. Normal reach required the subject to stand in a slumped upright posture with the upper arm vertical and forearm horizontal forming a 900 angle at the elbow. | Pelvis rotation angle and lumbar angle: Video analysis system (HuMaNTM motion analysis system) | OC, (no activation) |
| Lee (14) | Flat, round and extended back knee stretch exercise using a pilates reformer. Knee stretch positions is a kind of short lever front plank, in this case performed with 3 different back positions. | Pelvic stability and trunk stability: 3D motion analysis system using 16 infrared cameras | ADIM |
| Larivière et al. (44) | Standing plus trunk sudden perturbations. Participants stood upright in a trunk perturbation apparatus with the immobilized pelvis and thorax in a rigid harness. Perturbations were small (4 mm) but quick (in less than 40 ms) front and back disturbances of the trunk/harness, delivered randomly and repeatedly (n = 275 perturbations) within a 75-s period. | Lumbar stiffness: Total lumbar stiffness was separated into intrinsic and reflexive components based on the delay between the perturbation and the resultant force and calculated through a mathematical equation | OC (ABM) |
| Jung and Oh (22) | Leg pull front pilates exercise. The subject assumed a front plank position and performs a hip extension with the dominant leg to a predetermined target bar. | Angle of pelvis rotation: Smart phone-based measurement tool | |
| Butler et al. (31) | Standing lift of 3.8 kg load in maximum and extreme reaches. The maximum reach required the upper extremity to be straight and flexed at the shoulder. For the extreme reach the subjects were required to bend forward comfortably with their upper extremity similar to maximum reach. | Pelvis rotation angle and lumbar angle: Video analysis system (HuMaNTM motion analysis system) | OC (no activation) |
| Vera-Garcia et al. (16) | Sudden perturbation in semi-seated position. Participants were placed in a semi-seated position in a wooden apparatus that restricted hip motion while leaving the trunk free to move in all directions. Participants were rapidly and posteriorly loaded with a steel cable attached to a harness to load the trunk with a 6.8 kg weight. | Lumbar displacement: Electromagnetic tracking instrument | OC (ABM) |
| Grenier and McGill (53) | In-vivo: 10 Kg load in hands, right-hand load, and left-hand load. The testing was performed in an anatomically neutral standing posture, with a 10 kg load in either or both hands, depending on the condition. | Lumbar Stability: Three Space Isotrak unit | OC (ABM) |
| Fayh et al. (54) | Long stretch pilates exercise using a pilates reformer. Long stretch position is a kind of long lever front plank performed in a pilates machine with a spring ballasted sliding cart. | Pelvis stability: Bi-dimensional kinematics with one video camera | ADIM |
Summary Description of Tasks and Exercises, Types of Kinematic Measurements and Measurement Method of Interventions with Conclusive Results
4.2.1. Analysis of Tasks from the Load Approach
We classified each task based on the load imposed on the subject, following the criteria of Mottram and Comerford (35, 55, 56): (1) low-load tasks (LLT): Described as "normal postural control and non-fatiguing functional movements," performed at low speed, with dominance of Low threshold recruitment (LTR) of the local muscles. Low threshold recruitment is defined by the ability to perform a task slowly for 4 minutes or more without fatigue, effort, or requiring recovery time; (2) high-load tasks: Developed with high-load resistance or high speed, causing muscle fatigue and promoting co-activation of local and global muscles with the dominance of high threshold recruitment (HTR). A task is classified as HTR if it cannot be performed continuously for 2 minutes due to fatigue onset or if performed at high speed regardless of the load.
While classifying some tasks was straightforward, others were challenging, especially those involving external loads. We agree that a subject's physical conditioning can affect task classification, as the same load may be high for some but low for others. Therefore, fitness levels should be considered when selecting participants. We rigorously applied the LTR and HTR characteristics described above for task classification. Tables 4 and 5 provide detailed descriptions, classifications, and rationale for each exercise and task with conclusive results.
| Study | Task or Exercise | Type of Load, and, Rationale for Load Type Classification | Intervention with Better Results |
|---|---|---|---|
| Jeong and Chung (39) | Effect of a task-oriented training in sitting position: Arm reaching, ring stacking, ball kicking | Low load, normal postural control and non-fatiguing functional movements at low speed are considered LLT (35). | ADIM |
| Park et al. (32) | Prone hip extension | Low load, prone hip extension exercise is defined as a LLT (35). | OC (no activation) |
| Ko et al. (40) | Prone knee flexion | Low Load, Limb, spinal and pelvic control during non-fatiguing limb movements at low speed is considered LLT (35). | ADIM |
| Saiklang et al. (43) | Sitting for stature | Low load, normal postural control is considered a LLT (35). | ADIM |
| Lee and Lee (12) | Bridging exercise | Low load, bridge exercise included as a LLT (56) | ADIM |
| Jeon et al. (45) | Prone Hip Extension | Low load. prone hip extension exercise is defined as a LLT (35) | ADIM |
| Southwell et al. (46) | Unloaded slow repetitive spine flexion reaching task | Low load, normal postural control and non-fatiguing functional movements at low speed are considered LLT (35). | ADIM |
| Madokoro et al. (47) | Forward step | Low load, non-fatiguing functional movements at low speed are considered LLT (35). | ADIM |
| Park et al. (48) | Prone knee flexion | Low load, limb, spinal and pelvic control during non-fatiguing limb movements at low speed is considered LLT (35). | ADIM |
| Oh et al. (49) | Prone hip extension | Low load, prone hip extension exercise is defined as a LLT (35). | ADIM |
| Kim and Kim (15) | Side-lying hip abduction | Low load, limb, spinal and pelvic control during non-fatiguing limb movements at low speed is considered a LLT (35). | OC (ABM) |
| Butler et al. (31) | Standing lift of 3.8 kg load in normal reach | Low load, normal postural control and non-fatiguing functional movements at low speed are considered LLT (35). | OC (no activation) |
| Lee (14) | Flat, round and extended back knee stretch exercise using a pilates reformer. knee stretch positions is a kind of short lever front plank. | Low load, knee stretch exercise using a Pilates reformer is defined as a LLT (35). | ADIM |
| Study | Task or Exercise | Type of Load, and, Rationale for Load Type Classification | Intervention with Better Results |
|---|---|---|---|
| Larivière et al. (44) | Standing plus trunk sudden perturbations | High load, exercise or task that is performed at high speed will be considered a HLT (35). A sudden perturbation would be considered a HLT due to the need for a quick reaction. | OC (ABM) |
| Jung and Oh (22) | Leg pull front pilates exercise. Leg pull front position is a kind of long lever front plank. | High load, long lever front planks exercises are defined as a HLT (56). | OC (ABM) |
| Butler et al. (31) | Standing lift of 3.8 kg load in maximum and extreme reaches. | High load, A LLT should be performed without feeling of effort (35). A task requiring maximum and extreme intention would not meet this requirement and will be considered a HLT. | OC (no activation) |
| Vera-Garcia et al. (16) | Sudden perturbation in semi-seated position | High load, exercise or task that is performed at high speed will be considered a HLT (35). A sudden perturbation would be considered a HLT due to the need for a quick reaction. | OC (ABM) |
| Grenier and McGill (53) | In-vivo: 10 Kg load in both hands, right-hand load, and left-hand load. | High load, A 10 kg load could be considered a fatiguing load. An exercise that causes fatigue within the first 4 minutes will be considered HLT (56). | OC (ABM) |
| Fayh et al. (54) | Long stretch pilates exercise using a Pilates reformer. Long Stretch position is a kind of long lever front plank. | High load, long lever front planks exercises are defined as a HLT (56). | ADIM |
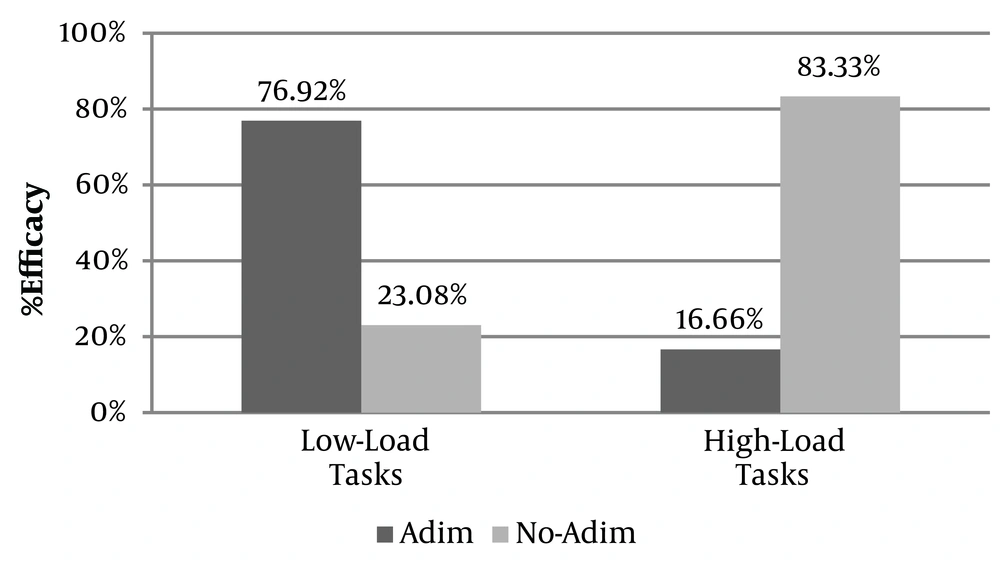
Of the 19 tasks and exercises with conclusive results, 13 were classified as low-load tasks and 6 as HLT. Abdominal drawing-in maneuver was the most effective option in 10 of the 13 LLT and only in 1 of the 6 HLT for spine, trunk, and pelvis stability, balance, and stature improvement. This indicates that ADIM, a global core muscle inhibition maneuver, performed better in 76.92% of interventions involving LLT and only 16.66% of interventions involving HLT.
In contrast, experimental conditions that did not attempt to inhibit the global muscles of the core, such as ABM and non-activation techniques, achieved better results for pelvis and lumbar stability, and lumbar stiffness in 5 of the 6 HLT and 3 of the 13 LLT. This suggests that other conditions (OC) were more effective than ADIM in 83.33% of HLT and 23.08% of LLT (Figure 2).
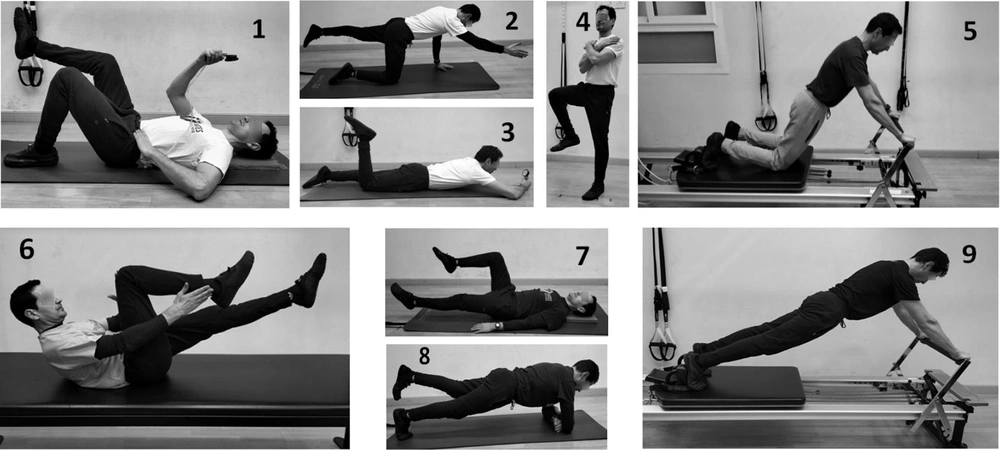
The LLT in these studies included prone hip extension, prone knee flexion, task-oriented Sitting tasks, unipodal and semi-tandem balance, bridging, unloading slow spine flexion, forward step, side lying hip abduction, and four-point kneeling scenarios. The HLT included sudden perturbations while sitting or standing, timed walking tests, long lever front planks, tasks involving a 10 kg load in the hands, and Standing Lifts with extreme reaching. Sudden perturbations are classified as HLT due to the need for a quick reaction (35), and timed-tasks also fall under this category as they require speed. Examples of different core training tasks are shown in Figure 3.
4.2.2. Other Approaches to Task Analysis
A key criterion for mechanical stability is the ability to maintain the system's state when faced with mechanical perturbation. We analyzed tasks based on the origin of the perturbation: (1) Perturbation of internal origin (PIO): Mechanical perturbations caused by the subject's own movements, such as leg raises or reaching with the hand; (2) perturbation of external origin (PEO): Perturbations from external forces, such as an external push, sudden load imposition, or base movement.
Most studies (17) used PIO, while only 2 used PEO [Lariviere et al. (44) and Vera-Garcia et al. (16)]. Results for PIO were varied: ADIM performed better in 8 cases, while OC performed better in 6. In both PEO studies, OC showed superior stabilization. While more research is needed to draw conclusive statements about PEO tasks, the initial results suggest ADIM may be less effective in these scenarios, warranting further investigation.
Another analysis criterion was the body position, specifically how it influences deep core muscle pre-activation. Richardson suggested that local muscles mainly serve antigravitational and weight-bearing functions (57). In lying positions (TrA unloading positions, TrAUP), core muscles are relatively deactivated, whereas upright positions [TrA loading positions, (TrALP)] involve greater muscle activation (58). Among the 19 conclusive tasks, 13 were performed in TrALP and 6 in TrAUP. Abdominal drawing-in maneuver performed better in 4 of the 6 TrAUP tasks, all of which were LLT. In TrALP tasks, ADIM and OC showed more equal performance, with ADIM performing better in 7 tasks and OC in 6. This suggests that ADIM’s preactivation in TrAUP tasks may be more decisive for core stability than in TrALP tasks.
4.3. Postural Guidelines and Internal Focus Effect
Of the 24 reviewed studies, only 7 described explicit postural requirements, and of those, only 3 provided guidelines to all intervention groups. We believe it is crucial to know whether postural guidelines were given, as this could impact the results by creating an internal focus effect.
Postural guidelines can direct attention to specific body regions or joints, promoting conscious control and potentially affecting movement responses. Internal focus strategies, although debated, have been shown to increase muscle activity and improve movement execution (59, 60). For example, in Fayh et al. (54), ADIM participants received a "Pelvic Imprint Technique" guideline, which promoted a slight posterior pelvic tilt. This direction-specific avoidance pattern likely conferred an advantage to the ADIM group, raising questions about whether ADIM or the postural guideline improved performance. Many studies did not specify whether postural guidelines were given, leaving room for doubt as to whether performance improvements were due to ADIM or an internal focus effect from postural instructions.
5. Discussion
5.1. Summary of Evidence
This review systematically evaluated the effectiveness of ADIM versus not using ADIM in stabilizing the core during various tasks, focusing on the load imposed during exercises. The results showed that ADIM performed better in 76.92% of interventions using low-load tasks, but only in 16.66% of HLT. Conversely, OC, including ABM and non-activation techniques, were more effective for pelvis, lumbar, and thorax stability, and lumbar stiffness in 83.33% of HLT and 23.08% of LLT.
Given that the majority of core exercises in fitness and sports conditioning involve high loads, the use of ADIM for such training should not be recommended. Furthermore, ADIM was less effective when the perturbation originated externally. Though more studies are needed, this suggests that ADIM might not be suitable for contact sports or other activities involving frequent external perturbations. Finally, ADIM preactivation was more impactful in TrA unloading positions (TrAUP) than in TrA loading positions, where extra activation was less beneficial. Many reviewed studies did not specify the use of postural guidelines, which may have influenced the results due to internal focus effects.
5.2. Transversus Abdominis vs. Rectus Abdominis
The key finding is that ADIM, a technique that selectively activates the TrA and decreases the activation of global muscles like RA, was less effective in stabilizing the core during HLT than techniques that do not inhibit global muscle activation. This aligns with the understanding that while TrA is critical for lumbopelvic stability, RA plays a vital role in controlling spinal orientation and transferring loads between the thorax and pelvis. The perpendicular alignment of TrA and RA muscle fibers may cause mechanical competition during ADIM, limiting RA's ability to assist in core stability. Electromyography studies suggest that ADIM decreases RA activation while increasing TrA activity, which could hinder stability during HLT by reducing RA's contribution to pelvic control.
5.3. Other Possible Arguments Against Abdominal Drawing-in Maneuver Use
Another possible consequence related to the mechanical imbalance between the TrA and RA muscles is the impact on Inter-Rectus Distance (IRD). It appears that contraction of the TrA, the pelvic floor muscles, or a combination of both, increases the IRD in postpartum women with diastasis rectus abdominis (DRA) (61). The activation of the TrA before a curl-up results in a relatively wider IRD compared to an automatic curl-up (without pre-activation of the TrA) in women with DRA (62). Performing a curl-up or abdominal crunch without any conscious effort to activate the TrA muscle decreases the IRD in postpartum women (63). Additionally, it has been suggested that the abdominal drawing-in maneuver (ADIM) may not be beneficial for individuals with severe abdominal DRA, hernia repair, or severe uncorrected abdominal hernia (3).
Furthermore, according to Lederman, individuals trained to use complex abdominal hollowing and bracing maneuvers should be discouraged from using them. It is argued that the continuous conscious activation of core muscles can potentially compromise the spine's structures by adding an extra level of compression (64). The reasoning is that compressive forces in the intervertebral discs are associated with low back pain (65), and it is acknowledged that compressive forces in the lumbar spine increase during abdominal muscle contraction (66). Therefore, if we consider that during regular core exercises or daily activities the abdominal muscles naturally activate due to task requirements, and if we add an extra level of contraction through conscious activation of specific core muscles, we might be subjecting the spine to additional compression. Moreover, as suggested by the findings in TrALP, the TrA muscle is already activated, and it is unclear whether further activation provides additional stability.
5.4. ADIM for Low-Load Tasks
We have already mentioned that the TrA, a local muscle of the core region, plays a significant role in the prevention and rehabilitation of low back pain (3). As a local muscle, the TrA has been characterized by its tonic activity, slow-twitch (type I) fibers with low-threshold activation, making it suited for low-load activities (6, 67). Its retraining should be performed in a specific and isolated manner from the global core muscles to restore its low-threshold tonic recruitment for low-load tasks (LLT) (68). As previously noted, the most common cue to activate the TrA is to "draw the abdominal wall in" (6). Therefore, the benefit of using this maneuver during high-load tasks (HLT) remains unclear. The results of this review show that the abdominal drawing-in maneuver (ADIM) was more effective in LLT, particularly during TrAUP, where TrA pre-activation through ADIM was more critical for core stability.
We also recognize that there is evidence suggesting that, in specific situations of low back pain or the early stages of the rehabilitation process, the TrA muscle may require an isolated retraining strategy. In these instances, a controlled and monitored ADIM could be useful. Some individuals may benefit from the use of ADIM when a low level of TrA activation is detected or as a strategy to develop awareness and control of the core muscles (17). However, we also align with the perspective that the brain focuses on movement or the goal of the movement, rather than the contraction of individual muscles (69, 70). Therefore, at some point in the motor reeducation program, it is advisable to phase out conscious muscle activation techniques.
5.5. Abdominal Drawing-in Maneuver for High-Load Tasks
Mottram and Comerford differentiate between the term "motor control stability," which includes isolated TrA muscle retraining, and "stability and core strengthening," referring to high-load stability tasks (35). Many core exercises used in fitness, sport training, and Pilates environments align more closely with the concept of "stability and core strengthening" exercises. ADIM performed worse in all HLTs except one, the study by Fayh et al. (54), where postural cues were used and the Internal Focus Effect may have influenced the result. According to the findings of this review, ADIM should not be used during "stability and core strengthening" exercises; specifically, ADIM should not be applied in HLTs.
5.6. Suggestions for Future Research
As we already pointed out in previous sections, postural guidelines generate attention on a specific joint segment, which affects the movement response during the execution of any task or exercise due to the internal focus effect. We therefore believe that it is important to specify in detail whether or not this type of guideline is used, as it can undoubtedly alter the outcome of a study. The lack of control in the application of these guidelines across different interventions makes it difficult to determine whether the improvement in stability was due to conscious muscle activation or the internal focus effect of the postural guideline.
In relation to this internal focus effect caused by alignment and postural guidelines, we propose conducting studies that compare interventions involving conscious muscle activation strategies with those that use only direction control cues. Such studies would help clarify whether muscle activation is truly responsible for improvements in stability or if the movement avoidance pattern resulting from direction control cues is the key factor.
5.7. Suggestions for Practitioners
Our suggestions and guidelines for the future of core stability training involve defining and observing different Order Parameters that describe the behavior of the system during each core stability training task. First, we must define the lumbopelvic work position during core exercises, as joint alignment will affect optimal joint loading and muscle activation (71, 72). Secondly, we must specify the site and direction to apply the direction control concepts described by Mottram and Comerford (35), with the goal of developing specific direction avoidance patterns in particular joint regions during different core stability training tasks. Third, we should pay attention to the localization of the breathing movement to define the characteristics of the ideal breathing pattern during loading tasks (73). Finally, we need to observe the effect of intra-abdominal pressure (IAP) during exercises, as inappropriate control of IAP increases can lead to an obvious bulging of the abdomen, indicating incompetent abdominal muscle function (74). Therefore, we should observe how the core muscles react to different positions, loads, and exercises in relation to IAP control to select the appropriate exercise with optimal load.
We acknowledge the methodological limitations of the present review study and the potential for bias, as it was conducted by a single reviewer. However, we also recognize the importance and novelty of the perspective and approach we provide. We encourage larger research groups to build on our analytical framework to further advance knowledge in this field.
5.8. Conclusions
The main finding of this review is related to the performance of ADIM in conjunction with high-load tasks (HLT). Conditions that employed ADIM, a technique aimed at inhibiting global core muscles, showed better performance in only 16.66% of interventions with HLT. In contrast, OC techniques, such as abdominal bracing maneuvers (ABM) and non-activation techniques, which do not aim to inhibit global core muscles, performed better in 83.33% of interventions using HLT. Therefore, if the goal is to train core stability and strength, ADIM should not be used. In tasks involving external perturbations, ADIM was less effective in stabilizing the core, and its use was also less impactful in upright positions.