1. Background
With the rapid advancement of technology, the widespread use of visual display terminals (VDTs), such as smartphones, tablets, and personal computers, has led to a significant public health issue—digital eye strain, also known as computer vision syndrome (CVS) (1). The primary symptoms of CVS include eye fatigue, blurred vision, dry eyes, photophobia, red eyes, and headaches, often accompanied by non-ocular symptoms such as neck and shoulder pain (2, 3).
Visual fatigue, a central feature of CVS, involves visual impairment, eye discomfort, and systemic symptoms that hinder an individual’s ability to perform normal visual tasks (4). Prolonged use of VDTs causes excessive strain on the eye muscles and frequent adjustments in focus, which increases eye fatigue, potentially leading to pseudomyopia and poor eye focus (5, 6), and may even result in exotropia (7). According to the latest statistics from the American Optometric Association, the prevalence of digital eye strain has surged globally, with rates as high as 75% in certain high-risk groups, such as contact lens users and individuals who frequently use multiple devices (8-11).
To address this growing concern, facial massage and exercise have been proposed as non-pharmacological interventions. Facial massage has the potential to improve blood circulation and enhance the blood supply to the eyes and surrounding areas by stimulating facial skin and muscles, which may help reduce visual fatigue. Studies have shown that both acute and chronic eye massage can increase blood flow to the eyes and alleviate eye fatigue (12). Additionally, massage helps reduce anxiety and stress, which are known contributors to increased fatigue. Research indicates that chronic stress and anxiety can elevate cortisol levels, leading to an imbalance in the autonomic nervous system (ANS), which negatively affects visual health (13). Sympathetic activity in the ANS has been identified as playing a regulatory role, often inhibiting relaxation (14). Moreover, individuals who use VDTs are often more susceptible to visual symptoms linked to anxiety and stress rather than vision or refractive issues (4, 15).
Current methods for alleviating visual fatigue include adjusting the working environment, using eye drops, and undergoing regular eye examinations, combined with raising awareness about CVS, modifying behavioral habits, and improving display equipment and monitor technology (16). However, these solutions are not suitable for everyone, and visual fatigue remains prevalent. Therefore, further exploration is needed to determine whether facial massage and exercise can provide additional or superior benefits compared to traditional methods.
Expected effects of facial massage and exercise include reducing visual fatigue, enhancing blood circulation, alleviating anxiety and stress, and improving eye muscle function. A cross-sectional study suggests that improving anxiety levels can have positive effects on alleviating visual fatigue and enhancing visual function (17). Facial massage may decrease sympathetic nerve activity, promote relaxation, and further relieve visual fatigue. It can also increase skin temperature and blood flow (18, 19), while reducing anxiety (20-23), depression (23), and sympathetic activity, and boosting parasympathetic activity (24, 25). The gentle mechanical pressure applied during massage may improve muscle compliance, increase blood flow, and parasympathetic activity while lowering neuromuscular excitability and stress hormone levels, thereby inducing a relaxation response (26).
Both full-body exercises and eye yoga exercises can effectively increase blood flow and promote circulation throughout the body and the eye area. Enhanced blood flow aids in providing nutrients to eye tissues and removing metabolic waste, thereby reducing visual fatigue. Eye yoga exercises can strengthen the adjustment ability of the eye muscles, enhance their flexibility and endurance, and effectively reduce visual discomfort caused by eye muscle fatigue. Full-body exercises and eye yoga exercises improve blood circulation (27), relieve stress (28), and enhance the regulation ability of eye muscles (29).
2. Objectives
In summary, this review aims to comprehensively evaluate the effects of facial massage and exercise on visual fatigue, explore their potential mechanisms, and provide guidance for future research directions. By conducting a systematic review of existing literature, we expect to identify gaps in current research to guide subsequent studies.
3. Methods
3.1. Pre-registration Agreement
This systematic review has been pre-registered on PROSPERO (registration number: CRD42024586404). The pre-registration protocol outlines the purpose, methods, and analysis plan for the study, ensuring transparency and consistency throughout the review process.
3.2. Search Strategy and Selection Criteria
3.2.1. Literature Search
To systematically assess the effectiveness and safety of facial massage and exercise in alleviating visual fatigue, this review followed the guidelines for systematic reviews and meta-analyses, developing a comprehensive search strategy. We selected four databases: Scopus, Web of Science, PubMed, and the Cochrane Library, and searched the literature from January 2000 to July 2024. Two researchers independently conducted the literature screening to ensure comprehensiveness and accuracy in the study selection.
3.2.2. Search Strategy
The search strategy involved using a combination of keywords and their variations, including "eye massage," "facial massage," "visual fatigue," "exercise," "randomized controlled trial," "crossover trial," "systematic review," and "meta-analysis." The search was restricted to English-language literature, with studies in other languages excluded to maintain consistency in the analysis.
3.2.3. Manual Search
In addition to the database search, we manually reviewed the references of relevant reviews to ensure no eligible studies were overlooked. This dual approach enhanced the comprehensiveness of the search and increased the representativeness of the research findings.
3.3. Research Selection
3.3.1. Inclusion Criteria
We included the following types of studies: Randomized controlled trials (RCTs), randomized crossover trials, clinical trials, intervention studies, and systematic reviews. Interventions could involve facial massage, eye massage, or various types of exercise (e.g., yoga, gymnastics). The participants in the included studies were either adults or children who reported symptoms of visual fatigue, and each study provided a clear description of the method used to assess visual fatigue symptoms. Comparison groups in the studies could include a placebo, usual care, or a control group without any intervention.
3.3.2. Exclusion Criteria
We excluded studies that were non-randomized controlled trials, non-randomized crossover trials, case reports, single-arm experiments, or those lacking a control group. Interventions that were not clearly stated or unrelated to visual fatigue were also excluded. Additionally, studies in languages other than English and conference abstracts were not included, ensuring data comparability. By establishing clear and detailed selection criteria, we ensured the quality and consistency of the included studies, thereby enhancing the reliability of the systematic review results.
3.4. Data Extraction and Quality Assessment
We extracted basic information from each study, including the study design, sample size, interventions, control groups, outcome measures, and results. The quality and risk of bias for each study were assessed using the Cochrane Risk of Bias Assessment Tool. For eligible studies, both quantitative and qualitative analyses were conducted.
3.5. Literature Screening Process
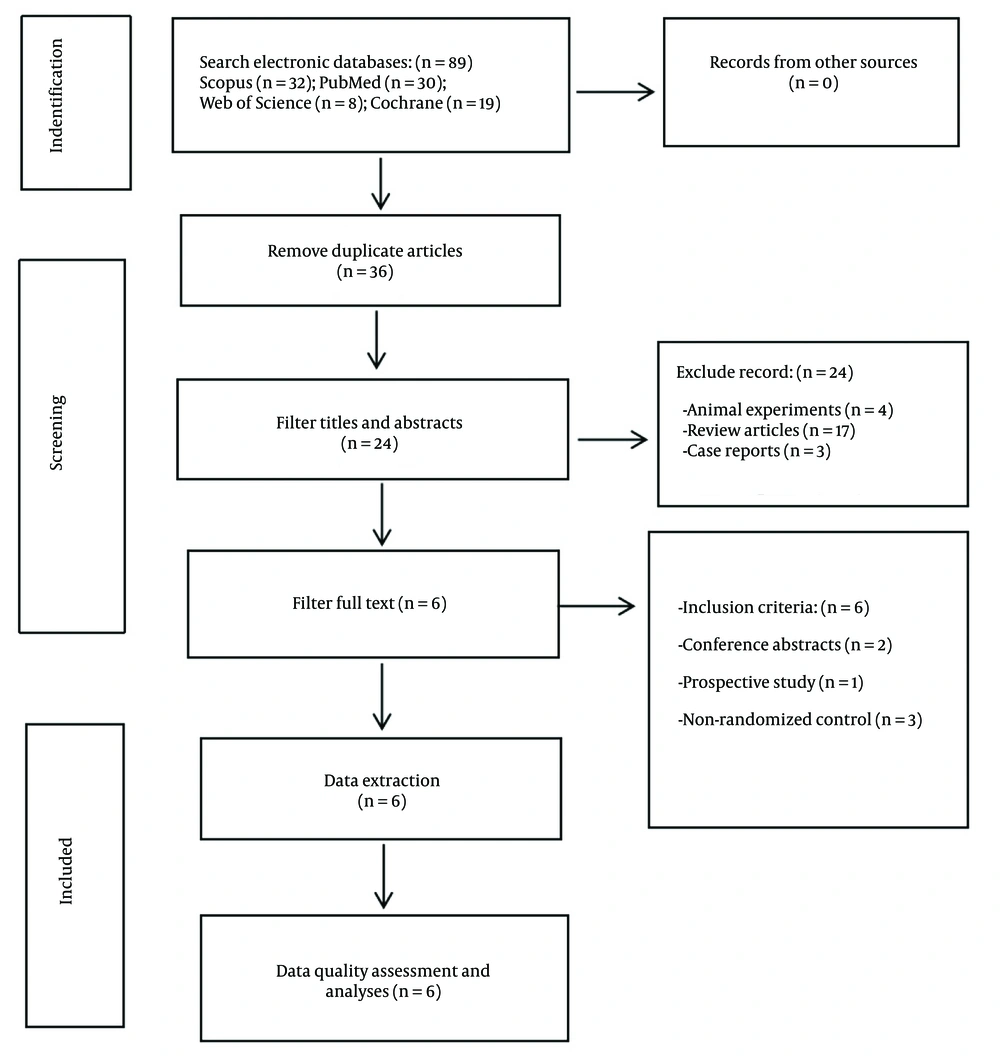
The PRISMA flow chart was used to illustrate the literature screening process. A total of 89 relevant documents were retrieved based on title and abstract searches. After removing duplicate articles, 36 articles remained. Further screening of titles and abstracts resulted in the exclusion of 4 animal experiments, 17 systematic reviews, and 3 case reports, leaving 24 articles. After reviewing the full texts, 2 conference abstracts, 3 non-randomized controlled trials, and 1 prospective study were excluded. A total of 6 articles were included in the final analysis, as shown in Figure 1.
The search strategy uses the Scopus database as an example, employing the keywords "facial massage" or "eye massage" and "visual fatigue" or "eye fatigue," combined with terms like "randomized controlled trial," "RCT," "crossover trial," "systematic review," or "meta-analysis." The search was restricted to English-language articles published between January 2000 and July 2024. The search process followed these steps: First, a preliminary search was conducted using the specified keywords in the title, abstract, and keywords. The search results were then exported to EndNote software, where duplicates were removed. Afterward, titles and abstracts relevant to the research question were screened. Finally, the full text of selected articles was reviewed to determine which studies would be included. The study selection process was independently reviewed by two researchers, and any disagreements were resolved through discussion to ensure the selection process was fair and accurate.
3.6. Quality Assessment of Included Randomized Controlled Trials and Crossover Experiments
This study used the Cochrane Risk of Bias Assessment Tool to evaluate the quality and risk of bias of each study. The tool consists of six domains: Random sequence generation, allocation concealment, blinding, incomplete outcome data, selective reporting, and other biases. The overall risk of bias is classified into three levels: Low risk (low risk in all areas or uncertain risk in only one or two areas), high risk (high risk in one or more areas, or serious concerns of bias), and uncertain risk (multiple areas of uncertainty or insufficient information). After evaluating the risk in each domain, the overall risk of bias for the study was determined. The quality of the included articles was generally high, and the findings hold significant clinical value. Detailed quality assessment results are provided in Table 1.
| Author(s), Year, Reference | Random Sequence Generation | Allocation Hidden | Blind Method | Incomplete Result Data | Selective Reporting | Other Offsets | Overall Offset Risk |
|---|---|---|---|---|---|---|---|
| Ohkawa et al., 2023 (30) | Low risk | Low risk | Uncertain risk | Low risk | Low risk | Uncertain risk | low risk |
| Hayashi and Du, 2021 (12) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | low risk |
| de Bruin et al., 2016 (31) | Low risk | Low risk | Low risk | Low risk | Low risk | Low risk | low risk |
| Gupta and Aparna, 2020 (29) | Uncertain risk | Uncertain risk | Low risk | Low risk | Low risk | Low risk | low risk |
| Lertwisuttipaiboon et al., 2017 (32) | Low risk | Low risk | Uncertain risk | Low risk | Low risk | Uncertain risk | low risk |
| Chan et al., 2015 (33) | Low risk | Low risk | Uncertain risk | Low risk | Low risk | Low risk | low risk |
4. Results
This study systematically reviewed six trials to evaluate the effects of facial massage and exercise on visual fatigue. The results confirmed that facial massage and exercise may provide relief from visual fatigue. As summarized in Table 2, all included studies were in English, with sample sizes ranging from 22 to 126 participants, aged 18 to 65 years. The interventions included both acute and chronic experiments. Acute experiments involved pre- and post-intervention measurements, while chronic experiments spanned 14 to 60 days. In total, 312 subjects were included in the analysis. The review and analysis suggest that facial massage and exercise may have specific preliminary effects in alleviating visual fatigue (Table 2).
| Author(s), Year, Reference | Subjects | Intervention Method(s) | Measurement Tool(s) | Result(s) |
|---|---|---|---|---|
| Ohkawa et al., 2023 (30) | Healthy women N = 22; facial massage group: N = 11; control group: N = 11; mean age: 20 - 22 years | Facial massage group: 3 minutes of facial massage first stage and 3 minutes of bed rest in the second stage; control group: 3 minutes of bed rest in the first stage and 3 minutes of FM in the second stage 6 minutes per intervention, 6 weeks total | POMS, VAS, blood pressure, SAA, pulse rate | Three minutes of FM significantly increased feelings of relaxation psychometrically, with participants reporting feeling "refreshed" and controls reporting feeling "sleepy." However, changes in blood pressure could not explain the reduction in stress. |
| Hayashi and Du, 2021 (12) | Healthy people (N = 40), Chinese eye exercise group: N = 10, massage roller group: N = 10, automated eye massager group: N = 10, control group: N= 10, mean age: 23.6 ± 2.3 years | Chinese eye exercise, massage roller, automated eye massager: Massage for 5 minutes, control group: No massage, Acute experiment, pre-and post-test, Slow experiment for 60 days, 5 minutes a day | OBF, static visual acuity, contrast sensitivity | Short-term periocular massage improves OBF and vision. |
| de Bruin et al., 2016 (31) | Young people with elevated stress levels (N = 126), mindfulness meditation (MM) group: N = 41, HRV-biofeedback (HRV-BF) group: N = 42, physical exercise (PE) group: N = 43, mean age: 18 -40 years | MM group: Daily mindfulness meditation, HRV-BF group: Daily mouse variation biofeedback, PE group: Daily physical activity, Duration: 5 weeks | ACS, Behavior Rating Inventory of Executive Function, Five Facet Mindfulness Questionnaire–Short Form, Self-Compassion Scale, Penn State Worry Questionnaire | Overall self-regulated daily meditations, daily HRV-biofeedback, and daily physical exercises lead to improved attention control, executive functioning, increased mindful awareness and self-compassion, and to less worrying. Mindful meditation did not outperform HRV-biofeedback or daily physical exercise with respect to these cognitive processes. |
| Gupta andAparna , 2020 (29) | Undergraduate students with visual fatigue (N = 32), exercise group: N = 16, average age: 20.94 ± 1.72, control group: N = 16, average age: 21.13 ± 1.70 years | Exercise group: Six weeks of yoga practice for 30 minutes a day, control group: No intervention | Visual Fatigue Questionnaire | Yoga ocular exercises can be considered as a nonpharmacologic and therapeutic intervention for reducing asthenopia symptoms as well as relieving the severity of eye fatigue. |
| Lertwisuttipaiboon et al., 2017 (32) | Computer users N = 32, intervention group: N = 16, control group: 16, mean age: 25 - 50 years | Intervention group: PEC plan, control group: No intervention, 30 minutes, 5 days a week, 1 month | Visual Fatigue Score | Both researchers and computer users could apply to reduce eye strain. |
| Chan et al., 2015 (33) | Myofascial pain patients (N = 60), intervention group: N = 32, control group: N = 31, mean age: 20 - 65 years | Intervention group: 6 sessions of physical therapy plus a combination of self-massage and home exercises, control group: 6 courses of physical therapy, 2 weeks. | Pain Scale, PPT, NDI, PSFS, HRV | Physical therapy combined with self-massage and home exercises is more effective than physical therapy alone. The combination of increased parasympathetic nervous system activity and decreased sympathetic nervous system activity results in less pain experienced by patients during daily activities. |
Abbreviations: OBF, ocular blood flow; ACS, Attention Control Scale.
5. Discussion
This systematic review included six high-quality studies investigating the effects of facial massage, whole-body exercise, and eye yoga exercises on visual fatigue. The key findings suggest that facial massage relieves eye fatigue by improving the function of the ANS and enhancing circulatory function. Whole-body exercise enhances overall blood circulation, relieves stress, and improves sleep quality, which indirectly benefits eye health. Eye yoga exercises directly strengthen eye muscles, improve their ability to adjust focus, and effectively reduce visual fatigue.
5.1. Mechanism of Facial Massage in Improving Visual Fatigue
Facial massage appears to alleviate visual fatigue through several mechanisms, including relaxing eye muscles, improving blood circulation to the eyes, and promoting lymphatic drainage. By stimulating local nerves and blood vessels, facial massage may enhance microcirculation in the eyes, thereby reducing visual fatigue.
5.1.1. Facial Massage and the Autonomic Nervous System
The ANS is composed primarily of the sympathetic and parasympathetic nervous systems. The sympathetic nervous system, commonly referred to as the "fight or flight" system, is activated during stressful situations, increasing heart rate, breathing, and blood pressure. In contrast, the parasympathetic nervous system, known as the "rest and digest" system, promotes relaxation and metabolic processes, such as digestion and urination, after stress (34). Massage is a well-known method for stimulating parasympathetic activity, improving mood, and reducing anxiety and depression (35). When the parasympathetic nervous system is activated, pupil constriction and a relaxation response occur, which can help alleviate visual fatigue (36). It is believed that the physiological changes induced by massage, such as enhanced muscle compliance, improved blood flow, increased muscle temperature, and reduced neuromuscular excitability, contribute to decreased anxiety and stress hormone levels, thereby generating a relaxation response (26, 37).
5.1.2. Facial Massage and the Circulatory System
Facial massage has also been shown to improve blood circulation in and around the eyes. Studies have demonstrated that eye massage can reduce intraocular pressure and increase blood flow to the retina and choroid, thereby improving overall ocular blood circulation (38). Acute periorbital massage can enhance short-term eye blood flow, while long-term massage helps maintain eye health and improve vision. Research has shown that periorbital massage positively impacts both short-term OBF and long-term vision health (12). Hamp et al. also found that facial massage can enhance general blood circulation (39).
5.1.3. Lymph Circulation
Massage has been shown to improve the function of the lymphatic system by promoting the flow of lymph fluid. By stimulating the contraction of lymphatic vessels, massage can enhance lymph flow, clear blockages, improve blood circulation, and provide more oxygen and nutrients to tissues, including the lymphatic system (40, 41). Research indicates that lymphatic vessels are present in the human choroid during both development and adulthood and that these vessels are involved in lymphangiogenesis. These findings emphasize the role of choroidal lymphatic vessels in maintaining ocular health and function, likely contributing to the regulation of ocular fluid balance and metabolic processes (42). The ocular lymphatic system helps preserve retinal health by regulating fluid balance and removing waste products from the eye. Dysfunction in the lymphatic system can result in increased intraocular pressure, inflammation, and retinal degeneration (41). Furthermore, studies suggest that the lymphatic system plays a crucial role in controlling intraocular pressure (43). Elevated intraocular pressure can cause tension and fatigue in the eyes. Therefore, facial massage may help alleviate visual fatigue by stimulating the lymphatic system, which in turn regulates intraocular pressure and improves ocular fluid balance.
5.2. The Mechanism by Which Exercise Improves Visual Fatigue
Exercise helps alleviate visual fatigue in two primary ways: Systemic exercise enhances overall blood circulation, providing the eyes with adequate oxygen and nutrients, relieving stress, improving sleep quality, and thus indirectly promoting eye health. Eye exercises, on the other hand, directly target the muscles of the eyes, improving their flexibility and focusing ability through specific movements and exercises.
5.2.1. Whole-Body Exercise
Whole-body exercise can improve visual fatigue by enhancing systemic blood circulation, delivering more oxygen and nutrients to the eyes, and promoting overall eye health. For example, whole-body vibration exercise, which uses mechanical vibrations transmitted throughout the body, is commonly used in rehabilitation and sports training. This form of exercise can significantly increase peripheral blood flow, improve blood flow velocity, and enhance vascular compliance by increasing muscle pumping action, ultimately boosting blood circulation (27).
Exercise also plays a significant role in reducing stress and triggering the release of endorphins, which help alleviate stress and improve mood. Daily physical activity has been shown to reduce stress and improve psychological well-being (31). It not only enhances mental health but also contributes to physical health, serving as an effective intervention for managing stress (28). Exercise has been found to improve mood, reduce anxiety and depression, and lower overall stress levels (28). Additionally, exercise interventions increase parasympathetic nervous system activity, helping the body manage stress more effectively by modulating the hypothalamic-pituitary-adrenal (HPA) axis response (44).
Moreover, regular exercise significantly improves sleep quality, including increasing deep sleep duration, reducing the time required to fall asleep, and enhancing overall sleep efficiency (45). Through these combined effects, exercise offers considerable benefits in reducing visual fatigue.
5.2.2. Eye Movements
Eye yoga exercises are considered an effective non-pharmacological treatment to reduce eye fatigue. In Gupta and Aparna's study, participants performed specific eye yoga exercises, such as moving the eyeballs up and down, left and right, and rotating them clockwise and counterclockwise. The results indicated that participants who engaged in these exercises experienced significant reductions in eye fatigue symptoms. Eye yoga exercises have been shown to positively impact eye blood circulation and increase the flexibility of eye muscles, making them a valuable addition to daily routines for preventing and reducing eye fatigue (29).
In Lertwisuttipaiboon et al.'s study, participatory eye care programs, which included simple eye movements like switching focus between near and distant objects, effectively reduced eye fatigue in office workers (32). Similarly, Kumar et al.’s research demonstrated that practicing Trataka Kriya—a traditional yoga practice that involves gazing at a fixed point or light source—significantly alleviated symptoms of digital eye strain, including eye fatigue, dry eyes, and headaches (46). During the COVID-19 pandemic in 2019, research showed that eye yoga exercises, including movements such as up, down, left, right, and rotations, effectively reduced eye fatigue in children and provided practical guidance (47). The Trataka exercise has also been found to reduce visual fatigue, lower anxiety levels, and improve mental health (48).
These studies suggest that facial massage and eye exercises could serve as effective methods for relieving visual fatigue. This finding has important clinical implications, as implementing simple facial massage and exercise strategies can help individuals relieve visual fatigue and improve their quality of life. Additionally, the prevention and treatment of eye fatigue through these methods could offer useful insights for ophthalmic clinical practice.
5.3. Limitations and Future Research Directions
5.3.1. Limitations
This review has several limitations. First, in terms of research design, many studies had small sample sizes, which may limit the generalizability and statistical significance of the results. Most studies also focused on short-term effects, lacking evaluation of long-term outcomes. Additionally, the sample populations were not diverse enough, often focusing on specific groups, without considering individuals of different ages, genders, or varying visual conditions. The complexity of the interventions, such as combining self-massage with home exercises, made it difficult to isolate the independent effects of each treatment. Variability in the speed, area, and intensity of massage also affected the consistency of the results. Furthermore, participants' psychological states may have biased self-reported outcomes.
5.3.2 Limitations of Meta-Analysis
This study was unable to conduct a meta-analysis primarily due to the significant heterogeneity among the included studies. Differences in study design, sample characteristics, interventions, and outcome measures resulted in insufficient comparability of the results. Many studies had small sample sizes, which could introduce self-reporting bias. Additionally, the complexity of the interventions and the lack of standardized methods further affected the consistency of the study results. Therefore, despite a comprehensive review of the existing literature, the inability to perform a meta-analysis is justified. To enhance the reliability of future studies, it is recommended to adopt uniform intervention methods and standardized measurement tools, which would provide a more robust foundation for subsequent meta-analyses.
5.3.3 Publication Bias
Although the quality of the included studies was assessed, the potential impact of publication bias must still be considered. Studies with positive results are more likely to be published, which may lead to an overestimation of the effectiveness of facial massage and exercise in reducing visual fatigue. Given the limited number of studies included in this review, it is possible that unpublished studies with differing results exist, potentially affecting our overall assessment of the interventions. To mitigate publication bias, future studies should emphasize transparent reporting and the publication of all findings, including studies with inconclusive or unexpected results. Additionally, statistical methods such as Egger's test or Begg's test should be employed in future systematic reviews to detect publication bias and evaluate the reliability of the included studies and the validity of their results.
5.3.4 Future Research Directions
To increase the generalizability of findings, future research should focus on expanding sample size and diversity, including participants of all ages, genders, races, and health conditions. Additionally, extending the observation period is necessary to evaluate the long-term effects of interventions, particularly with regard to different massage frequencies and durations. Standardizing intervention techniques—such as massage speed, area, and intensity—will improve the reliability of study findings. To minimize self-reporting bias, RCT designs and the use of independent evaluation instruments are recommended. Comparative research on different intervention methods (such as eye yoga exercises versus traditional eye exercises) would help clarify the relative advantages and broader applicability of each. Ultimately, personalized treatment plans should be developed to optimize treatment effectiveness and improve patient satisfaction.
5.4. Conclusions
Facial massage and exercise are two effective methods for alleviating visual fatigue. Research indicates that facial massage may reduce eye strain by enhancing blood circulation, relaxing muscles, and activating parasympathetic nerves. Exercise promotes overall blood circulation, helping to reduce stress and improve sleep quality, while eye yoga exercises strengthen the eye muscles to relieve visual fatigue. The combination of these approaches may produce a synergistic effect, offering a more comprehensive solution to combat visual fatigue effectively.