1. Background
Heart disease is one of the most common chronic illnesses in elderly and middle-aged people. Patients with heart failure due to decreased left ventricular systolic function demonstrate large end-diastolic volumes and have little contractile reserve (1). The prevalence of congestive heart failure appears to have increased in the USA (2, 3). Nearly 15 million people in the world and more than 4.9 million people in the United States are suffering from heart failure (4).
One of the common characteristics of patients with heart failure is exercise intolerance, which may be due to mass loss of muscle power leading to reduced performance in individuals' daily affairs and ultimately loss of ejection fraction and quality of life (5). In addition, poor physical conditions, mental stress, and readmission to hospital could also decrease the quality of life in these patients (6, 7), ending with depression and psychological disorders in their social relationships. Congestive heart failure significantly compromises quality of life by contributing to physical, role, and social functioning impairment as well as increased psychological distress (8-11). During the past two decades, quality of life in chronic patients, as one of the indicators of effective care and treatment, has been one of the important issues for clinical research. Some studies are being done to investigate the effect of quality of life on the differences among patients, the prediction of disease, and evaluation of interventions (12-16).
An exercise program, developed based on the physical conditions of patients, can promote the quality of life in heart failure patients. Also, in patients with chronic but asymptomatic (Class II) heart failure, exercise training is recommended alongside pharmacological and non-pharmacological therapies (7, 17). Training induces a delay in the increase in blood lactate, the rates of creatine phosphate consumption and glycolysis are frequently high and blood free-fatty acids increase gradually during exercise(17, 18). Aerobic training has been shown to improve the physiological components of aerobic metabolism. In particular, studies have repeatedly demonstrated an improvement in VO2 peak. This improvement is usually cited as being between 15 - 25% though has been documented as high as 36% (19). Exercise may cause further increase in left ventricular end-diastolic volume in these patients that would increase wall tension and may be detrimental to left ventricular function Also, it could improve total peripheral vascular resistance (TPR) and peripheral perfusion (7, 19).
Aerobic training reverses left ventricular remodeling in asymptomatic individuals with chronic heart failure (20). Studies have shown that patients with stable conditions that have regular and moderate exercise have better quality of life and less mortality rates compared to the patients who do not exercise (8). Because of low cost, accessibility, and easy use, exercise training is an intervention that could be recommended for most patients with heart failure (17). These studies suggested that patients, who had physical problems and were dissatisfied with their status, experienced a considerable progress in their physical ability after an exercise period. The results showed that there was a significant relationship between exercise ability and the level of satisfaction with quality of life in these patients. Compared with usual care, exercise training reduces heart failure-related hospitalizations and results in clinical betterments in quality of life among heart failure patients (20, 21).
Lifestyle changes such as doing exercise, and managing stress and excitement by the health team in patients with heart failure can help to reduce signs and symptoms of disease progression and improve quality of life (22). These changes in lifestyle of cardiac patients require follow-up, care, education, and interventions such as physical activity under the supervision of health care teams especially nurses (23).
Due to the increased incidence of heart failure and importance of exercise and other supportive interventions, such as stress and excitement management, and the fact that heart failure patients suffer from several problems, utilizing moderate exercise programs and understanding the effect of other factors on ejection fraction and quality of life by medical staff especially nurses can help to improve these patients' health considerably.
2. Objectives
This study was aimed to investigate the effect of exercise training on the quality of life and echocardiography parameters of systolic function in patients with chronic heart failure in Iran.
3. Patients and Methods
3.1. Design and Sample
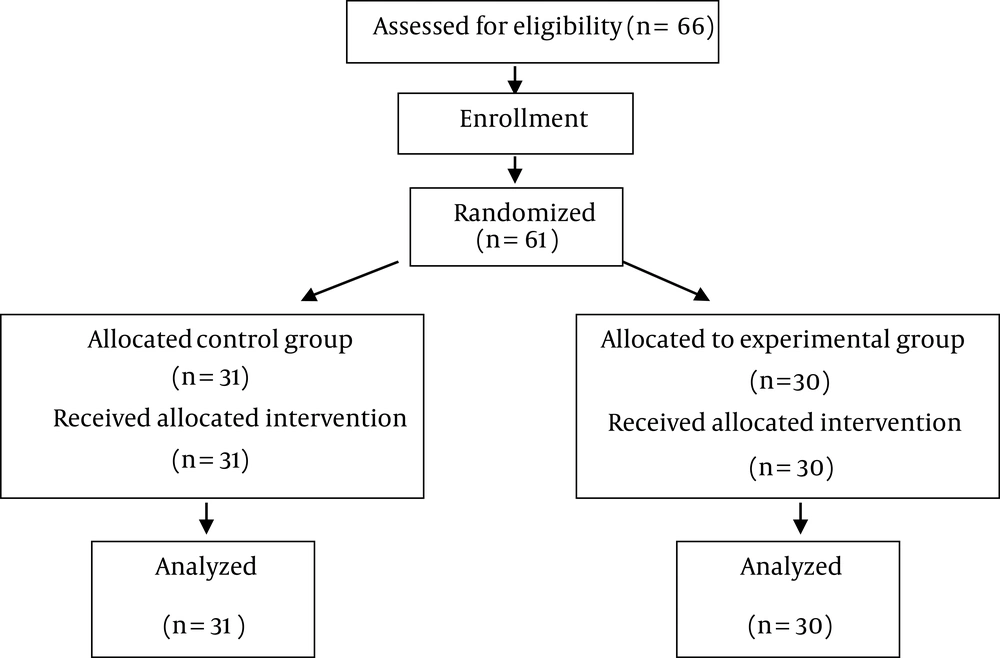
This is a quasi-experimental study in 2012. Statistician examined 66 patients for our study (33 patients each group with d = 0.13, p = 0.5 and q = 0.5). Subjects were randomly allocated (considering matching by gender and age) into two groups. The randomization code was developed with a computer random-number generator to select random permuted blocks. Then, these patients suffering from chronic heart failure were chosen. The patients were referred to the cardiology ward of Shahrekord University of Medical Sciences and were assessed for eligibility to participate in the study. Patients were randomized into control and experimental groups. Five patients were excluded from the study because of death, coronary bypass surgery, and refusal to receive treatment. Finally, 61 patients were participated in this study: control (including 31 patients) and experimental group (including 30 patients).
3.2. Inclusion Criteria
Inclusion criteria were male and female patients of 65 ± 15 years with chronic heart disease and consent to participate in the study. Other criteria for eligibility were diagnosis of heart failure, left ventricular ejection fraction of ≤ 40%, sinus rhythm, and being admitted by the Hospital. Chronic heart failure was based on clinical symptoms, echocardiographic evidence, and the physicians’ statements. In addition, the ability to perform the exercise program after the medication therapy, no difficulty with movement (such as rheumatoid arthritis, fractures, etc.), no heart transplant three months after exercise program, no advanced heart failure, and no traveling during the research were determined as other inclusion criteria.
3.3. Exclusion Criteria
Coronary bypass surgery during the research, neurological, orthopedic, peripheral vascular or severe pulmonary diseases probably intervening in successful completion of exercise tests, and being unwilling to cooperate were considered as exclusion criteria. Accordingly, in the experimental group three patients (one patient because of death and two patients for coronary bypass surgery) and in the control group, two patients (being unwilling to cooperate with the research team) were excluded from the study.
Procedure: The exercise program was performed three sessions per week for 24 weeks. The exercise program included 40 minutes, including 5-10 minutes for warm-up, 25 - 30 minutes of exercise (walking), and 5 minutes for cooling down) MET (Metabolic Equivalent) value of various common activities was light intensity activity: < 3MET). The patients, immediately after enrollment, underwent simple walking in a sport facility or gym in the hospital while they were supervised by a nurse or cardiologist. Exercise started until heart rate reached equal to 60% of heart rate reserve. After 6 sessions, the duration of the exercise (walking) was increased to 30 to 35 minutes, and heart rate to 70% of heart rate reserve. Each patient exercised based on his/her ability and resistance. Exercise was stopped when patients were physically tired or faced severe dyspnea, fatigue, dizziness or other problems that could jeopardize patient health based on Rhoten Fatigue Scale (RFS). To assess the reproducibility of gas exchange parameters, the cardiopulmonary test was repeated 3 to 5 days before starting the protocol for all patients and considered as baseline. The examination was repeated at the end of the study.
Patients in the control group received educational support but no exercise protocol; they were asked to continue their individually prescribed cardiovascular medications and their usual lifestyle but not to do any physical activity that caused breathlessness or fatigue and were supervised by their nurse and physicians.
Blood pressure and heart rate were measured before and after exercise. Drug treatment was not changed during the study in control and experimental groups. To further minimize the bias, we did not let the cardiologist who was informed of echocardiography results whether the participant was control or case (The physician who did perform echocardiography and the nurse who did data gathering were different from the physician and nurse that were monitoring the exercise).
3.4. Instruments
The required data were collected by MacNew Heart Disease Health-Related Quality of Life questionnaire (physical performance, limited activity following mental problems, limited activity following physical problems, energy and fatigue, physical problems, mental health, social performance and body pain). The self-administered MacNew questionnaire is designed to evaluate how daily activities and physical, emotional, and social functioning are influenced by heart disease, demographic characteristics, and echocardiography (2). Each of these 8 dimensions may be scored from 0 to 100. Scoring is performed according to criteria of SF-36 standards, with higher scores indicating better function (24, 25). The quality of life questionnaire was filled out and echocardiography was carried out on both groups by the researchers twice, before the exercise program at the hospital and 24 weeks after the exercise program (Figure 1).
3.5. Data Analysis
The obtained data were analyzed using SPSS software (version 11.5) through independent t-test. P < 0.05 was considered as the level of significance. For quantitative variables, mean and standard deviation and for qualitative variables, frequency and percent were used to report the data.
The ethical approval (with ethics code of 85-9-1) was obtained from Ethics Committee of the Shahrekord University of Medical Sciences and registration code of I.R.CT201306251376831 was issued by Iranian Registry of Clinical Trials for this study.
4. Results
The mean age of patients was 60 ± 4.25 years in the experimental group and 58 ± 4.22 in the control group. 60% in the experimental group and 74% in the control group were male. 83% of the patients in the experimental group and 81% in the control group had heart failure class III (Table 1).
| Variables | Experimental Group b | Control Group b |
|---|---|---|
| Gender | ||
| Male | 18 (60) | 23 (74) |
| Female | 12 (40) | 8 (24) |
| Age, y | 60 ± 4.25 | 58 ± 4.22 |
| Disease diagnosis | ||
| Ischemic cardiomyopathy | 21 (70) | 20 (64.5) |
| Dilated cardiomyopathy | 2 (6.66) | 1 (3.22) |
| Hypertension | 7 (23.4) | 9 (32.27) |
| Peak oxygen uptake, mL.kg/1.min-1 | 17 ± 12 | 18 ± 15 |
| NYHA class | ||
| I | 0 | 0 |
| II | 6 (20) | 6 (19.33) |
| III | 25 (83) | 25 (81) |
| Ejection fraction | 32 ± 4 | 33 ± 5 |
| Medications t | ||
| Digitalis | 21 (70) | 22 (68) |
| ACE inhibitors | 24 (80) | 27 (87) |
| Diuretics | 28 (94) | 28 (90.3) |
| Warfarin | 12 (40) | 13 (42) |
Baseline Characteristics in Patients with Congestive Heart Failure in Experimental and Control Groups a
The results show that there was no significant difference in ejection fraction and demographic characteristics between the two groups before the study. The results also showed that after exercise training, ejection fraction in exercise group increased from 32 ± 4 to 37 ± 4, but in control group, it decreased from 33 ± 5 to 33 ± 4. (Table 2). Independent t-test indicated that the quality of life score in eight dimensions was not significantly different between the two groups at the beginning of the study (Table 3).
| Variables | Exercise training group | Control group | ||||
|---|---|---|---|---|---|---|
| Baseline | 6-MonthFollow-up | P value | Baseline | 6-MonthFollow-up | Р value | |
| LV-EDD, mL/m2 | 65 ± 5 | 60 ± 5.2 | < 0.05 | 65 ± 4.7 | 66 ± 5.5 | > 0.05 |
| LV-ESD, mL/m2 | 58 ± 5 | 54 ± 4.5 | < 0.05 | 57 ± 6 | 57 ± 5.7 | > 0.05 |
| LV-EDV, mL/m2 | 224 ± 9 | 202 ± 8.5 | < 0.05 | 230 ± 7 | 228 ± 7.7 | > 0.05 |
| LV-ESV, mL/m2 | 155 ± 6 | 127 ± 6.3 | < 0.05 | 157 ± 5 | 155 ± 7 | > 0.05 |
| LVEF, % | 32 ± 4 | 37 ± 5 | < 0.05 | 33 ± 5 | 31 ± 5 | < 0.05 |
Ejection Fraction between the Two Groups (Before and After the Study)
| Group | Control Group b | Experimental Group b | Р Value |
|---|---|---|---|
| Life quality (8 dimensions) | |||
| Physical performance | 55.08 ± 8.62 | 54.22 ± 10.87 | > 0.15 |
| Limited activity following mental problems | 56.84 ± 10.33 | 57.18 ± 12.39 | > 0.47 |
| Limited activity following physical problems | 55.14 ± 9.91 | 54.32 ± 12.41 | > 0.71 |
| Energy and fatigue | 55.43 ± 11.67 | 56.69 ± 13.62 | > 0.84 |
| Mental health | 62.9 ± 13.76 | 63.12 ± 16.83 | > 0.56 |
| Social performance | 67.82 ± 15.68 | 66.62 ± 19.71 | > 0.37 |
| Body pain | 72.8 ± 16.55 | 71.1 ± 17.47 | > 0.35 |
| Overall health | 64.85 ± 17 | 65.12 ± 15.93 | > 0.66 |
Different Dimensions of Life Quality in Patients with Congestive Heart Failure in Case and Control Groups at the Beginning of the Study a
Independent t-test also showed that there was a significant difference in the physical performance, activity limitation following physical problem, energy and fatigue, social performance, physical pain, and public health at the end of the exercise program in the experimental group and 24 weeks after in the control group (Table 4). These results indicated that exercise program had a significant effect on promoting the patients’ quality of life score. The quality of life score was significantly different between before exercise program and at the end of the exercise program in the experimental group and 24 weeks after in the control group (Table 5).
| Group | Control Group b | Experimental Group b | Р Value |
|---|---|---|---|
| Life quality (8 dimensions) | |||
| Physical performance | 46.12 ± 7.24 | 56.16 ± 12.19 | < 0.05 |
| Limited activity following mental problems | 66.43 ± 8.69 | 48.34 ± 12.27 | < 0.05 |
| Limited activity following physical problems | 59.32 ± 7.51 | 50.74 ± 11.65 | < 0.05 |
| Energy and fatigue | 52.12 ± 9.76 | 58.42 ± 13.06 | < 0.05 |
| Mental health | 59.76 ± 12.28 | 68.78 ± 16.29 | < 0.05 |
| Social performance | 59.9 ± 11.51 | 69.56 ± 18.74 | < 0.05 |
| Body pain | 74.43 ± 16.38 | 68.18 ± 17.96 | < 0.05 |
| Overall health | 57.92 ± 18.5 | 70.28 ± 19.33 | < 0.05 |
Different Dimensions of Life Quality in Patients with Congestive Heart Failure in Case and Control Groups After the Completion of Intervention a
Mean ± standard Deviation of Different Dimensions of Life Quality in Patients With Congestive Heart Failure in Case and Control Groups Prior to the Intervention and After the Completion of the Intervention a
5. Discussion
The present study’s results showed that there was a significant change in left ventricular diameter and ejection fraction after exercise training in the experimental group. In a single-center study mortality decreased after exercise training (26) and some studies reported improved cardiac output response to exercise with no heightened pulmonary artery pressure (27, 28).
In a research, oxygen uptake increased by 26% at maximal exercise and 39% at the lactate threshold in the exercise group, whereas control values did not change (2). Also maximal oxygen uptake increased progressively after training. The increase in maximal oxygen uptake in the trained group paralleled an increase in maximal cardiac output but maximal cardiac output did not change in the control group (29).
In another study, the results showed that both resting and peak exercise pulmonary vascular resistance reduced after training therapy, indicating that the improvement in left ventricular systolic function may have led to a decreased preload and/or that an improvement of endothelial function may also have affected pulmonary resistance vessels (30).
Kitzman et al. found that an exercise program improved cardiac output but the response to the quality of life in individuals varied (31). Therefore, we require long term plans to determine the best response to increased ejection fraction. Why mild to moderate aerobic exercises lead to improved left ventricular ejection fraction and the general condition of patients with chronic heart failure, is not clearly known, but it could be argued that exercise leads to changes in lifestyle; increased mobility in patients and thus leads to higher peak VO2. On the other hand, exercise results in decrease in peripheral vascular resistance and thus increases blood flow in coronary vessels and reduces afterload.
In a study by van Tol et al. training sessions increased quality of life and ejection fraction (26). Exercise affects the endothelial membrane of peripheral vessels and therefore causes decreased resistance of peripheral vessels in relaxing and exercising. Therefore, it leads to decreased LV wall stress and afterload and increased cardiac output.
Also, in the present study the results showed a significant increase in quality of life especially in terms of physical performance, energy, social performance, and public health and a decrease in physical pain, activity limitation, physical problem, and fatigue at the end of the exercise program in the experimental group but not in the control group. Gary et al. obtained similar results, as well. They found that quality of life improved in the experimental group compared to the control group three months after the intervention but there was no significant difference in depression level at the end of the exercise program between the two groups (32).
In a study to determine the effect of a 12-week rehabilitation program on quality of life, aerobic ability, and the level of daily activity in the patients with heart failure, Collins et al. found a significant increase in physical performance, reduced sense of failure, and increased exercise tolerance in the experimental group. In addition, exercise had good outcome for the level of performance, ejection fraction, and the quality of life in these patients (33). Since exercise causes increased lung capacity, increased stroke volume, heart rate at rest and exercise, increased cardiac output, increased blood pressure and decreased diffusing capacity at rest and exercise, it leads to reduced anxiety, isolation, fatigue, and pain, enhances psychosocial function and improves overall health. Georgiou et al. found that exercise had a remarkable effect on reducing the cost of care and hospitalization, the referral to the physicians, and the length of survival (34). The study of Inglis et al. showed that exercise in patients with heart fibrillation decreased mortality rate, readmission, and days of hospitalization in the experimental group in comparison to the control group, but the level of anxiety and depression did not change significantly (35). Thus we can conclude that we need exercise programs, more care and intervention as well as specialized professionals in this field to enhance emotional, mental, physical, and social performance and public health and to decrease physical pain, activity limitation, and fatigue in heart patients. Exercise and lifestyle changes are the best tools for improving the ejection fraction and quality of life. We also must make use of the assistance of nurses for these patients’ better care.
Our findings show that quality of life is impaired in congestive heart failure patients. The results of this study indicate that exercise training in treating heart failure is important for increase in ejection fraction and improvement of the quality of life. Therefore, it is essential to address exercise, stress, excitement, and quality of life in these patients more seriously. In addition, dutiful and capable nurses can be helpful in this regard.
5.1. Limitations
Small sample size enrolled in this study limits the generalization of the study findings.