1. Introduction
Lipoma arborescens (LA) is a rare synovial disorder characterized by the replacement of subsynovial tissue with mature fat cells, often termed villous lipomatous proliferation of the synovium (1, 2). The suprapatellar pouch is almost always the affected site, with or without the lateral recesses of the knee joint (2, 3). Very rare cases in the wrist, elbow, shoulder, hip, and ankle have been reported, as well as an even smaller number of bilateral and polyarticular cases (4). LA equally affects males and females most often the 5th to 7th decades of life, though age range reaches as low as 9 years (2, 4). The most common associated pathology is joint effusion, followed by degenerative changes, meniscal tear, synovial cyst, bone erosion, and synovial chondromatosis (2, 4). Hypothesized etiologies of LA include traumatic, inflammatory, rheumatologic, developmental, and reactive processes (1, 4). The disorder can be classified into primary type that exists without associated joint changes and is more common in younger patients, and secondary type that occurs in the setting of degenerative joint disease and is more common in older patients (4).
2. Case Presentation
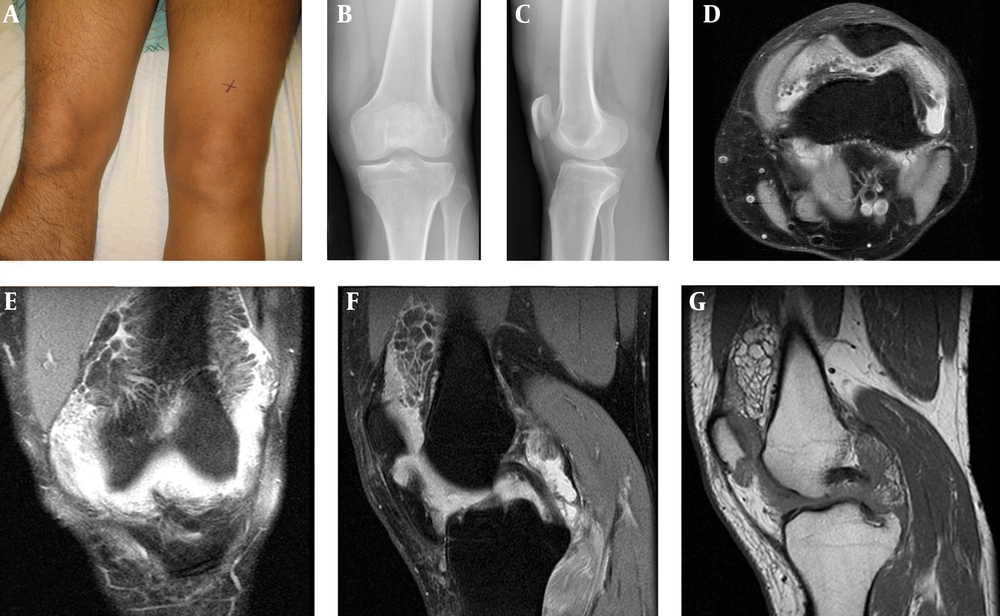
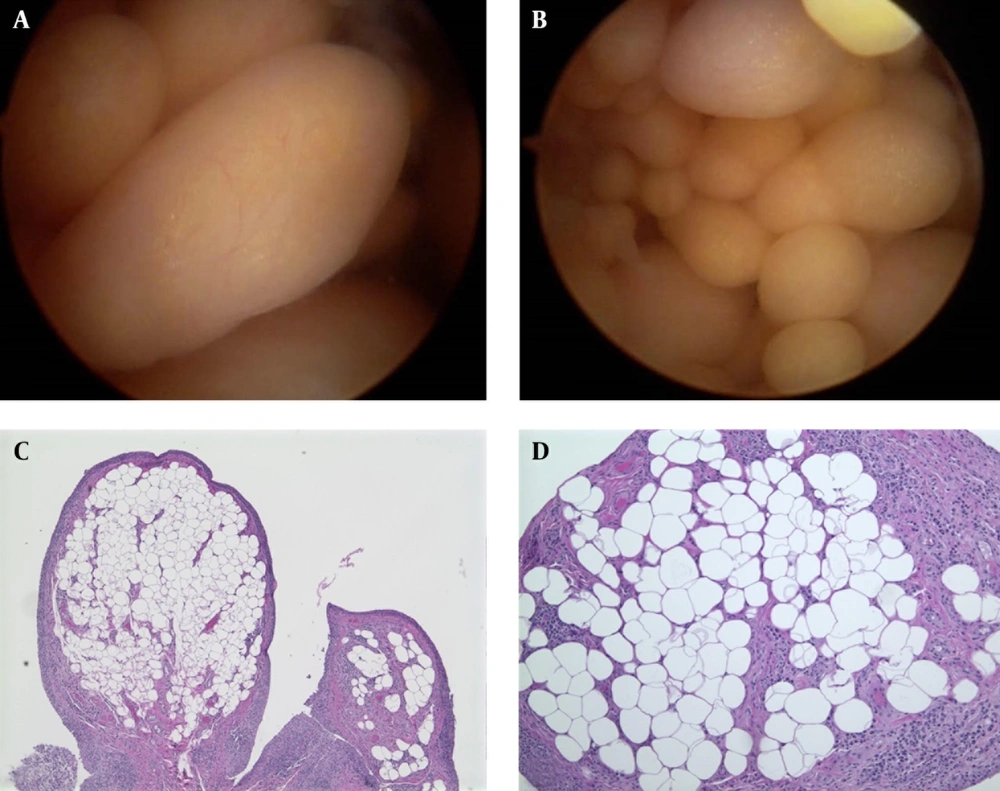
An otherwise healthy 37-year-old male presented with a complaint of left knee pain. Several months prior to presentation, the patient began noticing painless fullness in his knee after playing soccer. One month prior he developed anterior knee pain after a six kilometer run. Inspection showed obvious suprapatellar fullness on his left side (Figure 1 A). Palpation revealed additional fullness in the patient’s left posterolateral knee. Active knee flexion was limited to 90° with normal range of extension. Radiographs and MRI were obtained (Figure 1 B-G). The patient underwent an arthroscopic surgical resection (Figure 2 A and B).
2.1. Histological Findings
The surgical specimen measured 2.8 × 1.7 × 0.2 cm, macroscopically; the tissue was soft, yellow, smooth, and fatty. Microscopic examination revealed a villous architecture with a synovial cell lining (Figure 2 C and D). Some areas of synovial hyperplasia were present. Villous infiltrate consisted of mature adipose tissue with mild lymphoplasmacytic inflammatory infiltrate, all benign in appearance. Occasional hemosiderin-laden macrophages consistent with hemarthrosis were present.
A) Prominent swelling in the left suprapatellar pouch. B and C) Unremarkable x-rays. D) Transverse T2-weighted MRI reveals uniform adipose tissues in gutters. E) Coronal T2-weighted MRI reveals lobulated, uniform adipose tissues in the suprapatellar pouch. F) Sagittal T2-weighted MRI shows joint effusion and uniform adipose tissues in the suprapatellar pouch. G) Sagittal T1-weighted MRI shows uniform adipose tissues in the suprapatellar pouch.
A and B) Arthroscopy revealed the frond-like villi. C) Histology reveals a villous architecture with a surface synovial cell lining, hyperplastic in areas (hematoxylin and eosin, original magnification × 5). D) The villi are infiltrated by mature, benign adipose tissue along with a mild lymphoplasmacytic inflammatory infiltrate (hematoxylin and eosin, original magnification × 20).
3. Discussion
Patients with LA typically report gradual knee swelling, limited range of motion with or without locking, and variable pain (2, 3). In some patients, symptoms have progressed over years. Physical examination shows soft, painful, boggy swelling in the suprapatellar pouch with normal ligament stability (2, 5). Differential diagnosis includes pigmented villonodular synovitis, synovial hemangioma, rheumatoid arthritis, synovial lipoma, and synovial chondromatosis (3, 6). Hematology and synovial fluid labs are usually normal (1). Plain radiography shows occasional bone erosions and tissue density in the suprapatellar notch (6). Computed tomography (CT) shows synovial masses with attenuation values of fat and no enhancement with injected contrast. High resolution ultrasound may make a provisional diagnosis of LA by showing frond-like synovial thickening with real-time movement (6).
Variation in treatment and prognosis of similar pathologies necessitates accurate diagnosis, which is the best achieved by MRI (6). The uniform fat signal on any MRI modality is the key for narrowing the differential diagnosis (Figure 1 D-G). With LA, T1 weighted images demonstrate uniform high intensity signal for the synovial mass and low intensity signal from the adjacent effusion (6). T2 weighted images show high intensity effusion fluid infiltrated by multiple, low intensity projections from the fatty mass, most commonly in the suprapatellar pouch (6). None on the differential demonstrates the fat uniformity of LA (2, 4). Other fat suppression MRI modalities, such as STIR (Short Time Inversion Recovery), can be used to confirm the uniform fatty composition of the synovial mass (1, 2, 4). The frond-like appearance found by Patil et al. on ultrasound may implicate ultrasound as a specific but insensitive diagnostic test for LA (6).
A histologic diagnosis of LA is made when there is a diffuse presence of infiltrative, subsynovial fat. Grossly, the mass is bright yellow, shaped with a combination of villi and nodules, or more rarely with an overall frond-like appearance (1, 2, 5). Microscopically the lesion has papillary protrusions with a membrane of synovial cells covering mature adipose tissue with or without hyperaemic capillaries (3, 5). Synovial cells may appear reactive with eosinophilic cytoplasm or have an infiltrate of mononuclear inflammatory cells (3, 5). Treatment modality for LA has historically been open synovectomy, but reports of arthroscopic anterior synovectomy dominate the more recent literature (1, 5, 7).
LA is a rare synovial mass with unknown etiology. MRI is the best diagnostic modality which can be specific in the identification and characterization of LA (4, 6). Typical pattern on MRI shows an intra-articular synovial mass with characteristic frond-like morphology (4, 6). MRI should be performed prior to surgery in order to evaluate size, location, extension, and characterization of the mass. Ultrasound may reveal frond-like projections of the mass which move in real time, but it has low sensitivity in case of smaller lesions (6).