1. Introduction
As a cause of stroke, arterial dissections may happen at any age, but they are more common in the young population. Dissections are causes of approximately 20% of ischemic strokes in young adults. The annual incidence of spontaneous cervical artery dissections has been reported as 2.6 per 100000 in the USA. The mean age of patients was 44 to 46 years in North America and Europe. There is no clear gender or ethnic predominance in patients, but in some studies men were slightly more affected (1, 2). Most dissections occur spontaneously or after minor or trivial injury to the head or neck. Spontaneous cervical artery dissection has been classified as vertebral artery dissection or internal carotid artery dissection (3). Dissection has been reported in association with sports such as tennis (4), volleyball (5), basketball (6), skating (7), diving (8), dancing (9), trampoline use (10), and yoga (11). There are reports of arterial dissection immediately after swimming in a 60-year-old female (12), and also following sea wave trauma to the neck in a 56-year-old man (13). This report may be the first one of the spontaneous cervical arterial dissection in a young swimmer.
2. Case Presentation
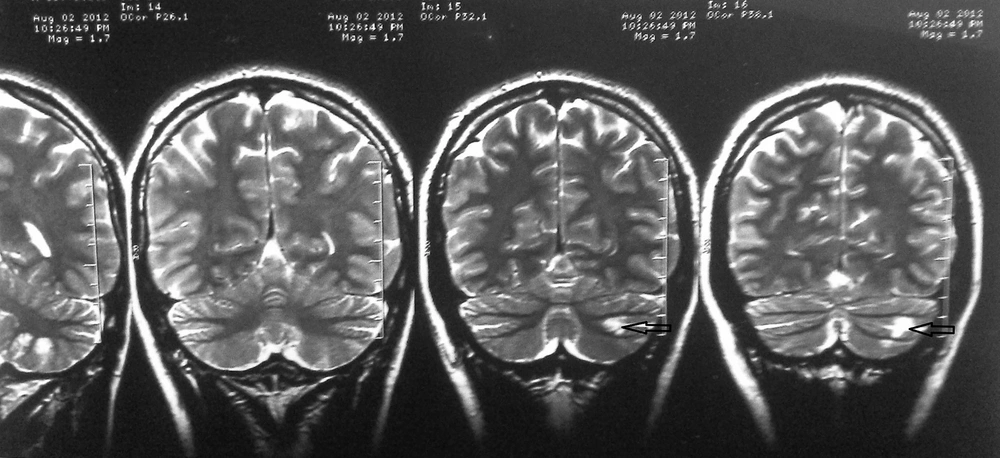
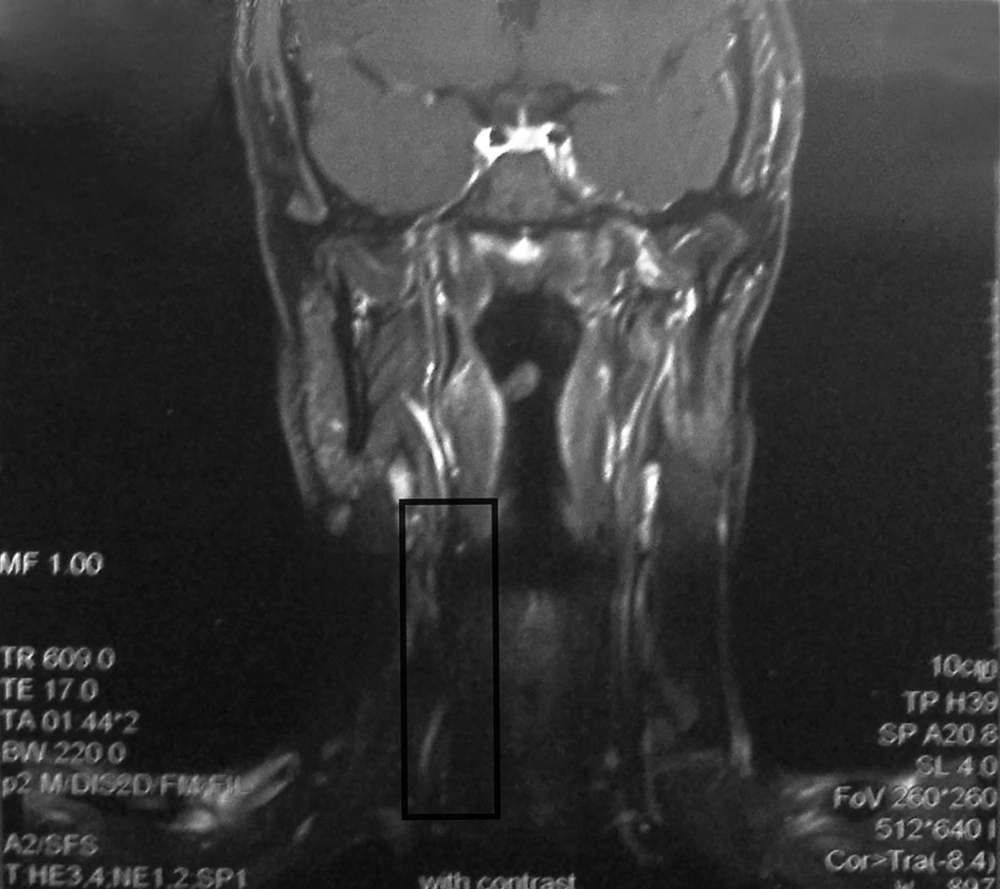
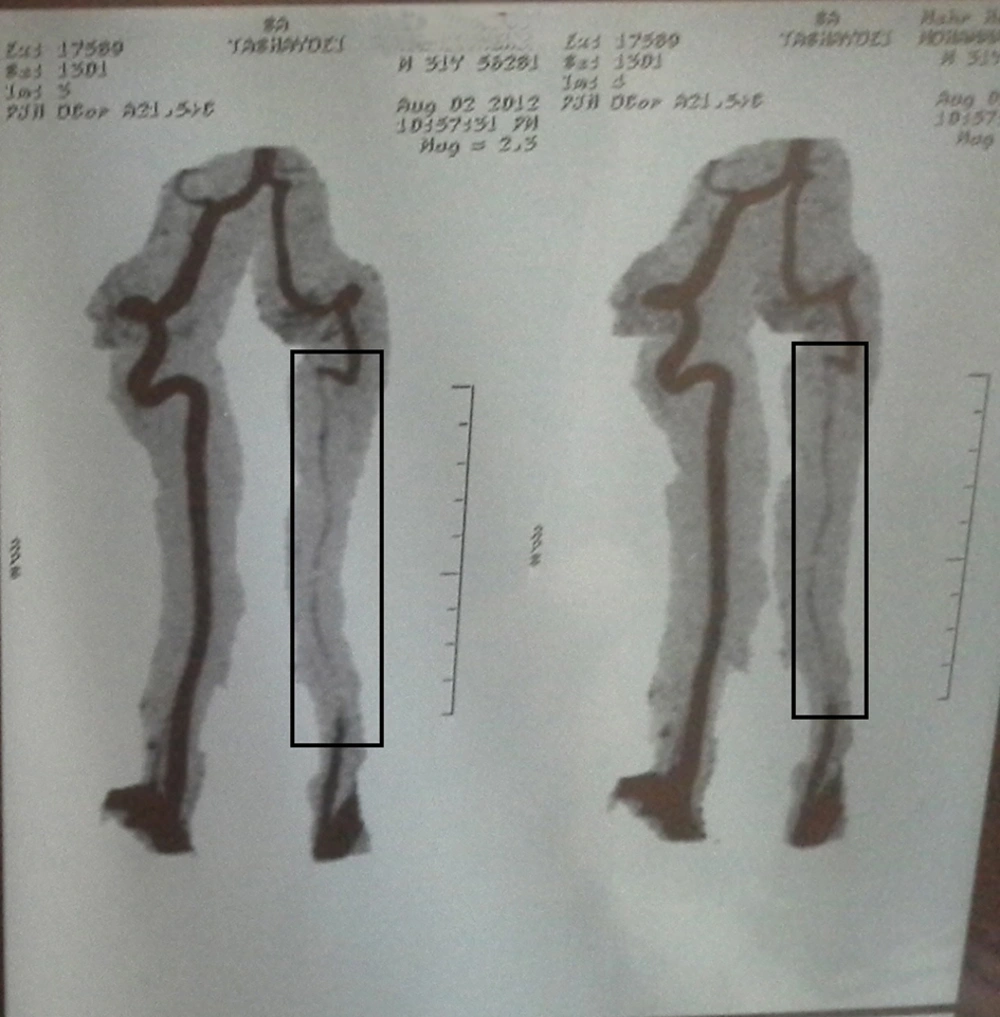
A 30-years-old male professional swimmer suddenly complained of moderate headache, neck pain, unilateral left facial weakness, and feelings of tingling and paresthesia on the left side of his body and face, a few minutes following head and body stretching exercises in land. There was no history of major head or neck trauma or manipulation. Also, he had not practiced any diving skills in the past. He had severe ataxia and could not walk without help, but he did not have any loss of consciousness. Acute infarction of the left cerebellum was diagnosed after brain computed tomography (CT) and magnetic resonance imaging (MRI) (with contrast) studies. Magnetic resonance angiography (MRA) of the brain was also done, which was normal. There was no history of major disease in his past medical history. Cardiac and rheumatological workups were normal. His brain and neck MRI (with contrast) and cervical MRA can be seen in Figures 1 - 3.
3. Discussion
Dissection usually causes an ischemic stroke or transient ischemic attack. The development of specific neurological symptoms and signs are related to the ischemia of tissues in the territory of the involved arteries or may result from the compression of the adjacent tissues by the aneurysmal dilatation of the dissected artery. They include local symptoms and signs such as head and/or neck pain (the two most frequent initial symptoms), Horner’s syndrome (approximately in 25% of cases), retinal artery occlusion, tinnitus, audible bruit, cranial neuropathies, scalp tenderness, orbital or monocular pain (rare in carotid artery dissections), cervical nerve root involvement (rare in vertebral artery dissection), or more generalized presentations such as cerebral ischemia and infarctions and in the case of vertebral artery dissection, lateral medullary infarction (Wallenberg’s syndrome) and other posterior circulation territory infarctions and spinal cord ischemia. Subarachnoid hemorrhage rarely occurs (1% of patients). The diagnosis of dissection is usually made with MRI or MRA of the brain or neck. Computed tomography angiography can be used for the diagnosis of cervicocephalic arterial dissection with the same sensitivity and specificity as MRA. Conventional angiography is reserved for younger patients in whom despite high clinical suspicion, there are no conclusive findings in noninvasive imaging studies. Important differential diagnoses of cervicocephalic arterial dissection include other vascular or neurological causes of the head and neck pain and/or local neurological syndromes (such as subarachnoid hemorrhage, migraine, and cluster headache) and other causes of brain ischemia such as cardiac emboli, atherosclerosis, and vasculopathy of brain vessels (14).
In the cervical MRI of this patient (with contrast), there were luminal abnormalities of the left vertebral artery such as arterial wall disruption and intramural hematoma (Figure 2). In the neck MRA of this patient, string sign could be observed with a low flow at the left vertebral artery with a normal flow at the proximal and distal parts of the artery, which are diagnostic of dissection (15) (Figure 3).
Also, the diagnosis of cardiac emboli and vasculopathy of the brain vessels was not considered for our patient as he did not have any history of cardiac or rheumatologic diseases and echocardiographic and brain MRI studies were negative for the findings of these diseases. It is important that sports medicine practitioners pay attention to this less-diagnosed cause of stroke in young athletes.