1. Background
Low back pain (LBP) is a common complaint in athletes participating at the high school, college and professional levels with more than 30% of athletes reporting it during their careers (1). More than 50% of young athletes experience back pain by age 15 and 10-15% report consistent back pain with activities (2, 3). The incidence of LBP in college athletes ranges between 7-65% and accounted for 30% of lost playing time for college level football players (4-6). Even at the elite level, this symptom is one of the most common causes of missed playing time with up to 75% of elite athletes having one or more episodes (7, 8). The pathology most commonly associated with lower back pain in athletes is degenerative disc disease, disc herniation, and/or spondylolysis/spondylolisthesis. However, other potential causes include Scheuermann’s kyphosis, sacral stress fractures, neoplasms, infection, scoliosis as well as idiopathic causes (5, 8-11)
2. Lumbar Degenerative Disc Disease
The etiology of degenerative disc disease in the general populace is multifactorial, including genetic predisposition, occupational/leisure physical loading, aging, smoking, and anthropomorphic factors (12, 13). Over the past 20 years, the thoughts regarding the development of disc degeneration has undergone a paradigm shift, in which physical loading activity that was once thought to lead to disc degeneration has been replaced with genetic-related factors (12, 14, 15). While current research on the general populace describes leisure and occupational loading as having only a modest effect on degenerative disc disease, elite athletes experience greater forces on the lumbar spine over prolonged and consistent training periods which typically start during childhood. These forces have been postulated to contribute to early degenerative changes and result in a higher prevalence of disc degenerative changes compared to non-athletes (13). From a mechanistic perspective, the primary concern is that degenerative disc disease can be induced in elite athletes by the daily, repetitive loads on a vulnerable, growing lumbar spine; often greater than those experienced by manual laborers (8, 13, 16-18).
2.1. Radiographic Imaging
Typically, plain anteroposterior and lateral radiographs are used in the initial assessment of discogenic pain. Flexion and extension lumbar radiographs may be used to show mobility across the lumbar segment; however, the cost of additional radiation has caused its clinical utility to be questioned (19). MRI imaging provides a more detailed view of disc pathology and is highly sensitive to degenerative changes such as loss of signal intensity on T2-weighted images, annular tears, high intensity zones, and associated bone marrow/vertebral endplate changes defined as Modic changes (20). The clinical significance of these findings is controversial, as one recent study suggested that the presence of high intensity zones, thought by many to correlate with back pain, does not reliably lead to a diagnosis of internal disk disruption (21).
2.2. Management
Rehabilitation Program Stages Stage Components Stage I: Early protected mobilization 1. Patient education: maintaining a neutral spine 2. Relative rest: < 2 days of absolute bed rest 3. Pain control a. Physical Modalities: superficial heat and cold b. Oral Medications: NSAIDS c. Manual Therapy d. Epidural steroid/anesthetic injections e. Short term bracing 4. Early exercise: Restoration of range of motion and low impact aerobics Stage II: Dynamic spinal stabilization 1. Gain dynamic control of segmental spine and kinetic chain forces a. Co-contraction exercises of the lumbar extensor and abdominals b. Progressive intensity c. Isometric strengthening Stage III: Spine safe strengthening and conditioning training 1. Isotonic exercises: Early gains related to improved neuromuscular control 2. Aerobic exercise: 20-30 minutes, 2-3 times per week Stage IV: Return to sports 1. Return to play requires a. Full, pain free range of motion b. Ability to maintain a neutral spine position during sports specific exercises c. Restoration of muscular strength, endurance and control 2. Plyometric exercises 3. Sports specific retraining Stage V : Maintenance program 1. Home exercises performed at least 3 times per week 2. Daily stretching
3. Lumbar Disc Herniation
Although it is yet unknown whether elite athletes are at higher risk for lumbar disc herniation (LDH), one of the most common mechanisms that cause a herniation in athletes is combined flexion with compression, compromising the material nature of the disc and annular fibrosis (29). Sports that replicate these movements include but are not limited to football, wrestling, hockey, gymnastics, tennis and golf. Lumbar disc herniation is a relatively routine complaint amongst athletes, with ages 20-35 at the highest risk for disc injury (29). This is supported by data from the National Football League reporting that lumbar disc herniation accounted for 8.6% of spinal injuries and resulted in an average of 52 days missed per injury (30). Furthermore, LDH accounted for 43% of all lumbar injuries for tennis players (29). For the elite athlete patient population, few studies on the treatment of lumbar disc herniation exist to guide treatment. In the flagship study from the Professional Athlete Spine Initiative (PASI) in 342 patients, players with a diagnosis of LDH from hockey, baseball, football and basketball, successfully returned to play 82% of the time, with 81% of surgically treated patients returning to play for an average additional 3.3 years (31).
3.1. Imaging
Plain radiographs may be normal in cases of lumbar disc herniation, although a lateral lumbosacral view may demonstrate a non-specific slight reduction in disk space height. Some authors contend that plain radiography is not useful in diagnosing disc herniation (32). MRI is the imaging modality of choice and typically accepted as the most sensitive test for detecting herniations and nerve root compression (5).
3.2. Management
3.2.1. Non-operative
In general, LDH in athletes carries a favorable prognosis with more than 90% of players with a disc herniation improving with non-operative treatment, showing a response to conservative therapy with improved pain and sciatica within 6 weeks of the initial onset (5). Non-operative treatment in athletes is similar to the general public, initially discouraging bed rest and encouraging early activity, such as a progressive walking program (5). While physical therapy for LDH typically consists of lumbar extension and core strengthening exercises, few, if any trials have shown these exercises to have a significant advantage over other treatments such as activity restriction (5). Epidural corticosteroid injections have questionable long-term efficacy but may provide an alternative to surgery in high level athletes (33).
3.3. Operative Treatment
While randomized control trials in the general population (SPORT) have demonstrated excellent clinical results after surgical treatment for LDH, outcomes in professional athletes have historically been less clear (34). These players have often been unfairly negatively profiled and scrutinized by the national media when they fail to meet expectations after surgery and ignored when they successfully return (31) Recent data from retrospective clinical studies suggest that clinical outcomes are better than that predicted from the lay press. In a study of 137 National Football League (a difference in outcome) players with LDH, surgical treatment led to a significantly longer career and higher return to play rate than those treated non-operatively ((37 months vs. 24 months, respectively; P = 03 ) and (36 games vs. 20 games, respectively; P = 002)) (10). Similarly, Schroeder et al. reported 85% RTP rates in 87 hockey players with no significant difference in rates or outcomes between the surgical and nonsurgical cohorts, an outcome found in major league baseball players as well (28, 35). These studies conclude that although a diagnosis of lumbar disc herniation has career-ending potential, most players are able to return to play and generate excellent performance-based outcomes, even if surgery is required (10). Recent data also suggests that physical demands specific to sport may affect outcome after surgical treatment for a lumbar disc herniation. For example, American football players have a significantly lower rate of return-to-play than baseball athletes, which could be explained by the physical nature of the respective sports (31). Furthermore, comparative studies show that a lumbar discectomy may lead to a shorter career in baseball players compared to non-operative treatment (233 versus 342 games, respectively; P = 0.08), suggesting that physical demands unique to this sport may lead to a difference in outcome (35). While the etiology of this effect has yet to be proven, some authors have postulated that the twisting nature of some sports may predispose players to chronic problems after disc surgery. In an in vivo study quantifying trunk axial rotation and angular acceleration in professional pitchers and batters, significant forces were generated with near front foot contact for pitching and after ball contact for batting (36). Other factors have also been demonstrated to affect performance-based outcome after LDH such as prior game experience and age at diagnosis. For example, game experience before injury was noted to be a positive predictor of career length after treatment, which may be explained by acquired skills that accommodate for any potential physical shortcomings seen after treatment (31). Not surprisingly, age at diagnosis has been a negative predictor of career length, which highlights the relatively short careers of these players (10, 31). It has been opined that the best performance-based outcomes from LDH occur in young, experienced athletes (10, 31).
4. Spondylolysis
Spondylolysis, a defect of the pars interarticularis of the neural arch, is a risk factor for low back pain, and has been reported in as high as 47% of young athletes presenting with LBP (37). Professional soccer and baseball players were noted to have spondylolysis incidence levels of 38.1% and 44.1%, respectively (38). Furthermore, in a group of 3132 symptomatic, competitive athletes, spondylolysis was diagnosed in 43% of divers, 30% of wrestlers and 23% of weight lifters (39).
4.1. Imaging
Plain radiographs can diagnose spondylolysis in many cases (11). The typical views are anteroposterior, lateral and oblique. While oblique films may show a fracture through the pars interarticularis with a “Scotty dog sign”, the amount of radiation from such a study coupled with the relative low sensitivity have led to many surgeons to abandon evaluation with this view (2). CT scan is considered the best method for identifying a spondylolytic defect, providing multiple views using thin cuts and allowing detailed visualization of the bony morphology, typically using a reverse gantry angle (40). Because CT is often unable to distinguish active and inactive lesions, this study can be used in conjunction with single photon emission computed tomography (SPECT), a nuclear medicine technique that uses radioisotopes to generate multiple imaging planes (11, 41). The radiation risk of neoplastic change with CT scans is present, especially in the female pediatric population, with the estimated number of cancer cases attributed to pediatric CT exposure is as high as one for every 300 abdomen/pelvis or 270 spine CTs (42). SPECT has a comparable radiation exposure of 3-4mSv, approximately half the dose of a spine CT (43). SPECT scans may be considered without CT, but only when an acute fracture is suspected. While historical use of MRI has not been recommended for detecting pars defects because of its inability to display adequate bony anatomy, more recent studies have suggested that specific sequences can allow for a high interobserver and intraobserver reliability compared to CT and SPECT scans, leading to an adopted classification system (40). Campbell et al. demonstrated that MRI was able to detect abnormality on 98% of pars defects and concluded that this could be used as a first line imaging modality for juvenile spondylolysis (40).
4.2. Management
4.2.1. Non-operative
The primary goal of spondylolysis treatment is to minimize pain while restoring function and motion. Conservative treatment is the first-line management for spondylolysis, with care given to bone healing potential, in hopes of limiting those conditions that lead to spondylolisthesis (44, 45). In acute fractures, athletes are instructed to undergo activity modification, including cessation of competitive play. Regardless of the activity modification program selected, patients must rest for at least a short duration to allow for bone healing. A study of soccer players showed decreased performance markers in those foregoing 3 months of rest, as compared to the cohort which underwent 3 months of rest prior to restarting play (45, 46). Bracing can also be used as an adjunct to activity modification. The most frequently referenced treatment and bracing protocol for spondylolysis is with use of a Boston brace with recommended wear of 23 hours a day (Figure 1). (2, 47). Clinical data in soccer players with spondylolysis suggests that compliance to the brace treatment regimen is likely more important than the particular brace type (45, 46). Regardless of protocol used, most published expert opinions agree that bracing is discontinued once the patient is asymptomatic, regardless of the fracture having healed.
A Boston Overlap Brace (48)
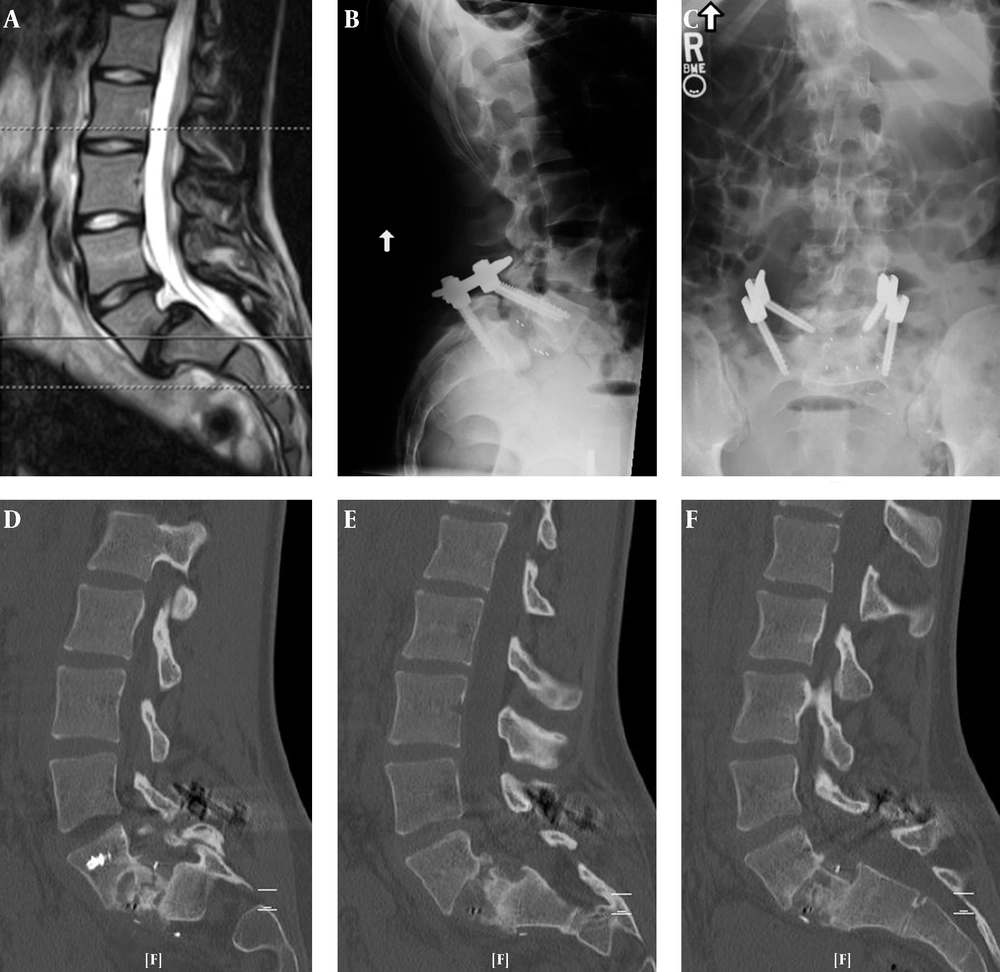
A 22-years-old Female Olympic Equestrian, Presented with Grade III Spondylolisthesis without Neurological Deficits. After a one-Level Anterior Lumbar Interbody Fusion with Percutaneous Posterior Fixation, Solid Fusion was Achieved 4 Months after the Operation. The Patient was Able to Successfully Return to Competitive Horseback Ridin
4.3. Operative
4.4. Return to Play
After a pars repair, Radcliff et al. describe a rehabilitation protocol beginning with core strengthening and non- impact activity 2 weeks postoperatively. During the first 3 months, all exercises are done with a neutral spine. At 3 months, higher impact training may start and at 4-6 months sport specific training begins. Athletes may return to play when they demonstrate normal strength, normal range of motion and no pain with sport specific activity; typically occurring at 6-12 months after surgery. This group notes that while radiographic evidence of fusion is preferred, this is the least important RTP determinant (45). Other studies demonstrate a wide variability in the recommendations of activity given by surgeons after lumbar fusion, ranging from 62-66% allowing RTP for noncontact sports at 6 months postoperatively to complete delay for at least one year (53, 54). Anecdotally, from our experience, there are very few restrictions after surgical treatment of spondylolisthesis (even with fusion) as long as the surgical construct spans one level (Figure 2). With the evidence that professional athletes can resume contact sports after such a procedure, players can be counseled as to the expectations after surgery. While the demanding nature of a twisting sport such as baseball is discussed when applicable, the evidence from our institution suggests that athletes can be encouraged to return to sport after an appropriate rehabilitation program following surgery.
5. Discussion
Degenerative spine conditions are common in athletes, especially at higher levels of competition, and present unique considerations when planning conservative and surgical treatment. Degenerative disc disease may be more common in competitive athletes, likely due to the incessant training at a growing age. The recent evidence-based literature regarding lumbar disc herniation in elite athletes suggests that it is reasonable to expect excellent clinical outcomes and successful return-to-sport after either operative or non-operative treatment, regardless of sport played. However, those athletes who require repetitive torque on their lumbar spines may have poorer long-term outcomes if surgical treatment is required. Painful spondylolysis in athletes can often be successfully treated non-operatively, however, when surgery is required, direct pars repair provides a motion sparing alternative which has been shown in athletes of all levels, including professional contact sports, to lead to successful return to play.