1. Background
Musculoskeletal disorders (MSDs) constitute common problems in dental practice. These disorders are characterized by discomfort, persistent pain or disability in different components of the musculoskeletal system including joints, ligaments, muscles, nerves, tendons, and structures that support limbs, neck and back not directly by an acute event but due to a chronic situation (1). MSDs may cause pain in the neck, shoulder, arm, wrist, hands, upper and lower back, hips, knees and feet (2). Reported prevalence of MSDs is about 63 to 93 percent among dental professionals (3). Among Iranian dentists, it has been reported as high as 49-75% in three different studies (4-6).
Some of these MSDs may be attributed to postural abnormalities or poor posture, especially in some demanding jobs such as dentistry. Different definitions have been suggested for poor posture. The American Academy of Orthopedic Surgeons (AAOS) defines poor posture as a faulty relationship of the different body parts, which creates increased strain on the supporting structures. Moreover, persisting postural faults can result in discomfort, pain or disability (7, 8).
Previous studies have identified correlation between sagittal posture alteration and low back pain (LBP) as well as neck pain (9). On the other hand, the effect of pain on normal posture has been shown in the past studies (10).
There are some associated factors, which may play important roles in pathogenesis and persistence of musculoskeletal complaints in dentistry. Some of these proposed factors include static and dynamic awkward postures, repetitive movements (11, 12), fine-tuned function (13), vibrating instruments (14, 15), inappropriate lighting (11, 16), genetic factors, physical conditioning, emotional stress and psychological factors (17, 18). These features of clinical work are the predisposing factors for continued static positions (19, 20), prolonged spinal flexion (21) and poor posture (22, 23). Otherwise, there may be some potential parameters, which may have a role, including age, gender, occupational experience, academic grade, dominant hand, working hours and specialty.
In addition to effects on personal life, previous studies have identified that MSDs in dentistry may considerably influence the social life and result in diminished working efficacy and early retirement. (22, 24-26).
2. Objectives
To our knowledge, although the musculoskeletal health of dentists has been the subject of numerous published works, however, their focus has been on the pain and working posture rather than habitual posture (25, 27). As the faulty habitual posture may have a significant role in development and persistence of musculoskeletal pain and consequently unfavorable effects on the carrier of dentists and due to the paucity of available evidence regarding postural abnormalities of dental professionals, the objective of the present study was to investigate the prevalence of the head, shoulder and spinal postural disorders and to determine the probably correlated personal and occupational factors in the Iranian academic dentists.
3. Patients and Methods
This descriptive study was conducted in January 2012 to June 2013 on 96 dental staff including academic professors, residents and senior students in Tehran University of Medical Sciences. They were invited to participate via written notification, email, short message system and face to face. Exclusion criteria were any history of known rheumatoid disorders, cancer, neurologic disorders, trauma as well as surgery in shoulders and spine.
First, the procedures were explained for each participant and all of them signed the informed consent form; then, personal and occupational characteristics of participants, including gender, age, dominant hand, academic grade, specialty, occupational experiences, daily and weekly working hours and current musculoskeletal pain as well as its location were recorded using a researcher-made questionnaire. The anthropometric measurements were assessed by stadiometer for height (meter) and medical scale for weight (kilogram). body mass index (BMI) was calculated by dividing weight to square height (kg/m2).
An expert physician assessed the posture of all participants with palpation and marking the determined landmarks using small and non-allergenic stickers. These landmarks included the tragus of the left ear, the left acromial process and the left lateral malleolar process and the spinous process of 7th cervical vertebra.
Forward head posture, rounded shoulder posture and scoliosis were assessed using a plumb-line and checkerboard. Assessment first was done in sagittal plane. The participants were asked to stand laterally behind the plumb-line on the predetermined feet locations, and then forward bending was done three times. Afterwards, they were instructed to stand in their normal, comfortable posture, arms resting by the sides, with feet shoulder-width apart and equally balanced on both feet.
According to the Kendall and McCreary definition, lateral posture is considered normal, if the plumb-line passes through the tragus of the ear, C7 spinous process, the acromial process, the greater trochanter, just anterior to the midline of the knee, and slightly anterior to lateral malleolus. Therefore, forward displacement of the tragus and acromion compared to plumb-line in lateral view will be considered as FHP and RSP, respectively (7).
Then, procedure was progressed on the coronal plane for posterior postural assessment. The participants were requested to stand back to the standard checkerboard. The scoliosis was investigated in form of any deviation of the spine. If there was any doubt about existence of the scoliosis, the participants were asked to perform Adam’s forward bending for further assessment of the condition. In assessment session, all of the procedure was repeated three times one after another by the same examiner and results were recorded.
To assess hyper kyphosis and hyperlordosis, a flexible 32 inch ruler (flexi curve) was used. This instrument consists of a flexible metal ruler covered in plastic and can be molded to the spine in order to reproduce the back shape. Flexible ruler is a low-cost, non-invasive and valid instrument comparable with the radiological Cobb’s method. Reliability and validity of this instrument for lumbar and thoracic regions have been shown in some studies, which demonstrated significant correlation between this method and Cobb’s angle method (10, 28-32).
To measure the thoracic curve, participants were asked to swing their hands three times and stand in the straight-line position with habitual body posture. The flexible ruler was molded along the contour of the spine and the C7, T1, T12 spinous processes were recorded using the metric scale incorporated in the device. Then the ruler was removed carefully and the internal curve (the side of the ruler in contact with the skin) was drawn onto graph paper. Thereafter, it was straightened again and the procedure was repeated three times by one rater and same device.
In the next stage, the flexible ruler was molded along the contour of the lumbar spine and the L1 and S1 spinous processes recorded. Drawing the lumbar curve onto paper and repeating the procedure were done similar to the previous process. Later, kyphosis and lordosis angles were calculated and converted to Cobb’s angle equivalents, using the following method:
After tracing the curvatures, thoracic length (L1) was drawn by connecting the T1 mark (most superior point) to the T12 (most inferior point). Thoracic width (H1) was considered as the greatest width from the thoracic curve to the vertical line. For each trial, Kyphosis Angle (KA) was calculated according to the following formula:
Kyphosis Angle = 2Arctang (2H1/L1) (33). Then Cobb’s angle for thoracic curve was determined, using the subsequent:
CAT = 0.8587 FAT + 6.9064
(CAT, Cobb’s angle for thoracic curve; FAT, flexible ruler angle for kyphosis) (10).
The average of three-kyphosis angles was used for further analysis. Available evidence has shown that the calculated angle is systematically smaller than the Cobb’s angle; therefore, by scaling 1.53 to the flexicurve angle, the Cobb’s angle was calculated (31). Lordosis angle (LA) was calculated according to the following formula:
Lordosis Angle = 4Arctang (2H2/L2) (28).
In the equation, lumbar length (L2) is the distance from the L1 to the S1 mark and lumbar width (H2) is the greatest width from the lumbar curve to the vertical line. For conversion of this angle to the Cobb’s equivalent, the correction with the linear transformation formula was done:
CAL = 0.7702 FAL + 9.6924
(CAL, cobb’s angle for lordosis; FAL, flexible ruler angle for lordosis) (10).
Again, the average of three-lordosis angles was used. Regarding the acceptable range of spinal kyphosis or lordosis angles, there are conflicting reports in the literature. The accepted ranges for normal thoracic kyphosis and lumbar lordosis have been reported between 20 to 50 degrees and 31 to 79 degrees (from L1 to S1), respectively (34). In the present study, we labeled the faulty postures as hyper kyphosis and hyperlordosis when the measured Cobb’s angles exceeded two standard deviations more than reported adult norms for thoracic and lumbar curve angles. Accordingly, figures of 50 and 60 degrees were considered as cut-off points, respectively (35, 36). Additionally, although there is a positive correlation between thoracic kyphosis and lumbar lordosis, (37) we considered their prevalence separately in the present study. The study was approved by the Research Ethics Committee of Tehran University of Medical Sciences.
3.1. Statistical Analysis
Data were analyzed using SPSS version 17. Baseline data was computed as prevalence. The between- groups differences were assessed using Chi-square and Fisher exact test. Independent sample t-test and One Way ANOVA were used to detect association between quantitative and descriptive parameters. Moreover, Simple Luminal Logistic Regression Analysis was performed to evaluate the individual characteristics and some associated factors at work on the occurrence of abnormal postures. The important confounders of gender and age were always included in each model, regardless of their significance. These analyses were carried out separately for postural disorders. Relevance odds ratio with 95% confidence intervals (95% CI) were calculated as a determinant of association. P < 0.05 was considered statistically significant.
4. Results
Ninety six dental staff of Tehran University of Medical Sciences including 53 females (55.2%) and 43 males (44.8%) were recruited in this study. Participants consisted of general dentists and senior students (40.7%) and specialists in different fields of prosthetics (14.6%), pediatric dentistry (12.5%), endodontic (7.3%), periodontics (7.3%), orthodontics (7.3%), restorative dentistry (6.3%) and radiology (2.1%). Among the participants, 85 (88.5%) and 11 (11.5%) persons were right and left-handed, respectively. Basic characteristics of the participants are shown in Table 1.
| Parameter | Mean ± SD | Range |
|---|---|---|
| Age, y | 31.1 ± 10.1 | 21 - 66 |
| Height, cm | 169.5 ± 9.2 | 150 - 192 |
| Weight, kg | 65.9 ± 13.2 | 41 - 106 |
| Body mass index, kg/m2 | 22.8 ± 3.4 | 14.7 - 32.8 |
| Weekly working, h | 27.8 ± 12.9 | 5 - 60 |
| Daily working, h | 5.2 ± 2.1 | 2 - 10.5 |
| Total experience | 95.8 ± 114.1 | 5.5 - 392 |
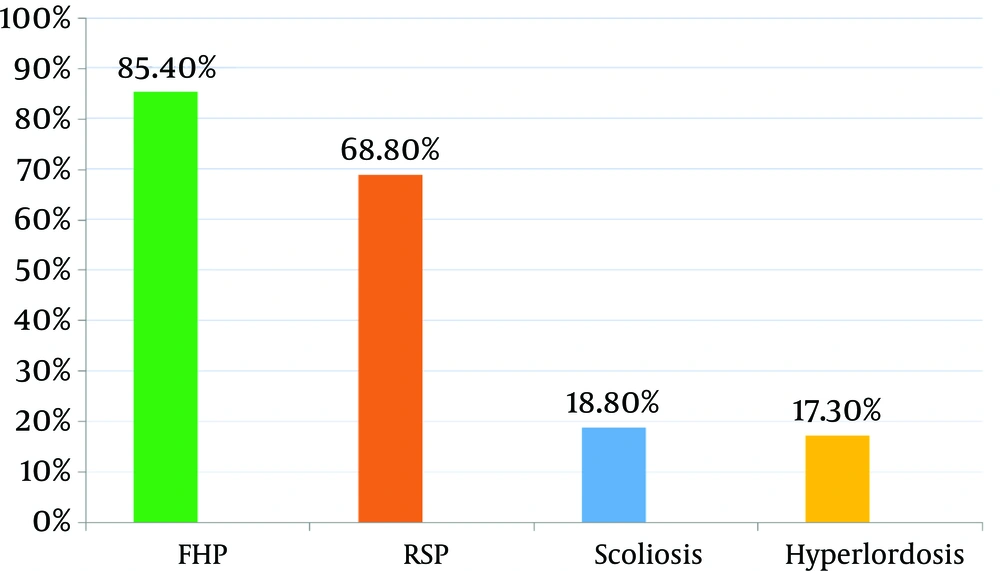
Regarding work-related MS pain, almost 59.4% of subjects suffered from this type of pain. The most common sites of pain were neck 41 (42.7%), low back 39 (40.6%), shoulder 24 (25%) and hand 23 (24%). Concerning the prevalence of common postural disorders, FHP was the most prevalent abnormal posture (85.4%), followed by rounded shoulder (68.8%), scoliosis (18.8%) and hyperlordosis (17.3%). No case of hyper kyphosis was identified (Figure 1). Kyphosis and lordosis angles measured by Flexicurve and Cobb’s equivalent are shown in Table 2.
a Values are expressed as mean ± SD.
The correlations were observed between scoliosis and gender (weight-adjusted OR = 0.13) (P = 0.009; 95%CI = 0.07 - 0.74) and hyperlordosis and weight (P = 0.007; 95%CI = 1.9 - 15). In addition, alternative analysis with Fisher’s exact test showed significant correlation between gender and FHP (P = 0.04; 95%CI = 0.07 - 1.1). However, no significant correlations were found between identified postural abnormalities and probable associated factors such as dominant hand, academic grade, specialty, dental work experience, and weekly working hours (P > 0.05).
5. Discussion
The results of this cross-sectional study indicated the high prevalence of some awkward postures and revealed that the majority of the participants had at least one postural abnormality (Figure 1). The prevalence of postural disorders in a study on healthy subjects between the ages of 20 to 50-years-old was 66% and 73% for FHP and right RSP, respectively (38). However, the prevalence of FHP in the present study was higher compared to the healthy population. Prevalence of adult scoliosis in a previous study was 8.3% (39). In another study on persons with 40-years-old or over, prevalence of scoliosis was 8.9% and it was associated with race and age, but not with gender (40). The prevalence of 18.8% among our participants indicates higher prevalence of scoliosis in dentists compared to general population. Regarding hyperlordosis and hyper kyphosis, a research project reported the prevalence of these postural disorders as 16% and 10% respectively among the young adults (32). In our study, prevalence of hyperlordosis (17.3%) is similar to this study. Furthermore, no case of hyper kyphosis was found in the participants, which is contrary to the data on the general population. However, the comparison of our findings with other similar studies on the habitual postural disorders may have limited value due to significant differences in assessment instruments as well as diverse methods of measurement. Otherwise, the data on prevalence of habitual postural disorders among dentists are sparse.
According to the survey’s results, 59.4% of the participants had suffered from self-reported work related pain. The prevalence of MS pain in this study is less than reports from Australia (87.2%) and Turkey (94%) (41, 42), as well as previous studies on Iranian dentists (73% - 75%) (4-6). It may be related to the younger age of our participants (including senior students), as well as more emphasis on ergonomic rules because of the academic milieu. The common sites of pain in the study were in the neck, low back, shoulder and hands. In the other studies, these sites were reported as the most common sites of problems in the dentists (4-6). This data are in accordance with our study.
Regarding the correlation between postural disorders and the gender, our study showed that FHP was less prevalent in female sex. Existing data regarding this correlation are contradictory. Results of some studies reported much more males who experienced anterior neck posture than females; similar to our study (31, 43). In another investigation, no significant difference was found between genders for anterior head and shoulder alignment (33). The lower prevalence of FHP in females in our study may be attributed to the 20% less weekly working hours of female dentists compared to males [25.8 (11) in females vs. 30.3 (14.6) in males]. In this study, significant correlation was reported between gender and scoliosis, and after adjustment for weight, female gender was a protective factor against scoliosis posture. About RSP posture, kyphosis and lordosis, our study did not demonstrate any significant correlation with gender. However, restricted existing evidence implied that RSP was more prevalent in females (43). Regarding postural disorders and demographic and anthropometric characteristics, there was significant correlation between weight and hyperlordosis; as with each 10 kg increase in weight, 60% increase for hyperlordosis was reported. Previous studies had identified positive correlation between hyperlordosis and weight. We did not find any statistical correlation between age, height, working hours as well as experience of dental practice and posture. Concerning the postural disorders and academic grade, FHP, RSP and scoliosis in the students were more frequent than academic staff and residents. However, the statistical correlation was not found. In the existing literature, there was no similar investigation.
About correlation of postural disorders with different specialties, although there was not any significant correlation, some postural abnormalities were more prevalent among particular specialties, as the following: FHP in endodontic, RSP and scoliosis in endodontic and periodontics and hyper kyphosis in restorative and periodontics. However, in this survey, the sample size for specialists was not large enough for any significant conclusions to be drawn, or to establish a relationship between the type of specialty and the location of pain in different parts of body. Although the cross-sectional study does not permit causal inference, the observed relations give valuable evidence for further research and policy making.
With regard to high prevalence of postural disorders and MS pain among dental practitioners, we suggest postural assessment as an ordinary and periodic exam for dentists. Besides the measures to diminish the pain, effective education and intervention for correction of the habitual posture can play a prominent role in prevention and management of MSDs in dentists.