1. Background
Athletes’ health is an important issue and for promoting it, pre-participation examination (PPE) is widely performed by responsible bodies around the world. While the sudden cardiac death (SCD) incidence in sports is rare (1:50,000 to 1:200,000 annually) (1, 2), it must be considered as an important cause of death among athletes, so early diagnosis of any fatal disorder could prevent sudden death. Sudden cardiac death has been defined by world health organization (WHO) as a fatal condition that happens within 24h after onset of symptoms (3). At the 26th Bethesda conference “athletes’ SCD” was defined as: “non-traumatic, nonviolent, unexpected death due to cardiac causes within one hour of the onset of symptoms. Sports-related SCD are defined as those with symptoms occurring within one hour of sports participation” (4).
Most of the deaths reported in sports are related to cardiovascular conditions (5-11) and hypertrophic cardiomyopathy is the most common cause among them. The other fatal cardiovascular conditions which result in SCD include major Vascular anomalies, valvular disorders, coronary ischemic heart disease, Wolf Parkinson white syndrome, arrhythmogenic cardiomyopathy, long Q-T interval, aortic aneurysm, cardiac conduction disorders, myocarditis, and the other congenital heart diseases (12). That is obviously clear that most of SCD causes could be diagnosed by electrocardiogram (ECG), and it should be considered that under the age of 35, genetic and congenital disorders are more common and for people above 35 years old, coronary artery disease is the most common causes of SCD (13). The risk of SCD increases by rising of age and exercise intensity (11, 12). The other non-cardiac causes of sudden death among athletes are head, chest and abdominal traumas (9-11, 14). It has estimated that sudden death cases are 2 times more common among athletes comparing to non-athlete people (3). Therefore it could be concluded that early diagnosis of cardiac disorders has an important preventive role in sudden death. On the other hand many of the above mentioned causes are hereditary, so in case of any SCD the other family members should be examined for screening (15). It is a critical issue to find a reliable and specific approach to diagnose people exposed to SCD (4). Many countries have their own attitude to PPE for detecting possible causes of sudden death such as Spain (16), USA (17-24), Sweden (25), Denmark (26, 27), Norway (28), Italy (26, 29, 30), Switzerland (31), Germany (32), France (33), Netherland (34), China (35), Japan (36, 37), and UAE (38). These examinations are also routinely performed for all athletes participating at major sports events like Asian games and Olympic games by Iran’s Sports medicine federation. The examination consists of a comprehensive questionnaire, full physical examination (by cardiologist as well as orthopedic surgeon, sports medicine specialist, optometrist and internist), a 12 lead 2-dimensional electrocardiogram (ECG), routine blood and urine laboratory examinations (such as blood cell count, hemoglobin, serum iron, fasting blood sugar, lipid profile, liver function tests, blood urea nitrogen, creatinine, and urine analysis). In recent years an echocardiography has been added to these examinations. Supplementary exams and para-clinicals such as radiography and magnetic resonance imaging (MRI) are also done upon request of physicians.
2. Objectives
Our aim was to investigate the prevalence of cardiovascular abnormalities in history, examination and electrocardiography of Iranian elite athletes participating in Asian games.
3. Materials and Methods
In this retrospective study, all profiles of athletes participating at Asian games who referred to Iran sports medicine federation during 2012 to 2013 were reviewed. Most of the athletes were at the peak of exercise and physical fitness. All athletes were examined one by one by expert general practitioners and specialists, the setting of examinations was based on station-type which means multiple examiners conducted discrete portions of PPE in sequence. We had two stations for heart examination. In the first station, medical history was taken and also cardiovascular system was examined entirely by a cardiologist. In the second station ECG and blood pressure were recorded by an expert. The 6-channel ECG device (brand name: CONTEC®, Model Number: ECG600G) as well as Richter® mercury sphygmomanometer were used. Then all data were reviewed and evaluated by a sports medicine specialist. All profiles with missing data were omitted. All data related to cardiovascular system including past history, familial history, and physical examination as well as ECG interpretation were extracted and analyzed again. Sokolov-Lyon criteria was used for the detection of cardiac hypertrophy. Electrocardiographic criteria for right atrial hypertrophy was a peaked P wave (P pulmonale) with amplitude bigger than 2.5 mm in the inferior leads (II, III and aVF) or bigger than 1.5 mm in V1 and V2. Diagnostic criteria for right atrial hypertrophy was bifid P wave with more than 40 milliseconds between the two peaks or total P wave duration more than 110 milliseconds in lead II or biphasic P wave with terminal negative portion bigger than 40 milliseconds duration or biphasic P wave with terminal negative portion more than 1mm deep In V1. For long QT syndrome we used from QTc) Corrected QT). QTc is prolonged if it was more than 440 milliseconds in men or more than 460 milliseconds in women. Inverted T was important for us in inferior leads (II, III, aVF), lateral leads (I, aVL, V5-6) and anterior leads (V2-6). Standard for left axis deviation was QRS axis less than -30 degrees and for right axis deviation, QRS axis greater than +90 degrees.
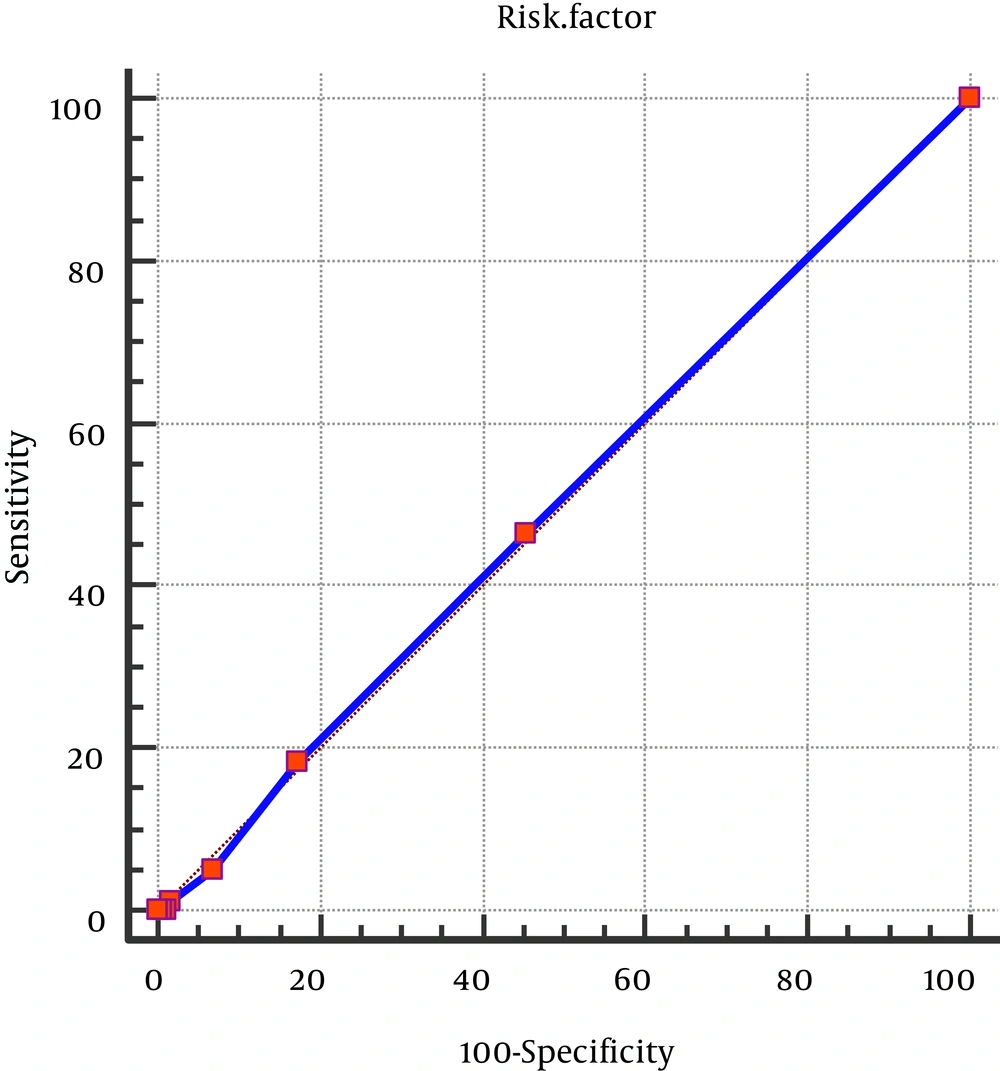
To study single variable impact, IBM SPSS Statistics® software version 21 and multiple logistics regression of R® statistical software were used at the same time. In order to determine any relation between clinical signs and symptoms and ECG changes, Chi-squared (X2) test as well as Fisher exact test were performed. First bias reductions also performed because despite the likelihood function converges, some of the parameters are not convergent. In order to predict ECG changes by taking history and physical examination, receiver operating characteristic (ROC) curve was performed. Level of significance was set as 0.05.
This study was approved by ethical subcommittee of Iran Sports medicine federation education and research committee.
4. Results
in total, 388 elite athletes including 80 females (20.6%) and 308 males (79.4%) participated in this study. The youngest one was 16 and oldest one 36. Comparing 21 various sports disciplines, dragon boat athletes were 48 persons and team of diving and tennis consisted of of 4 athletes. Baseline characteristics are shown in Tables 1 and 2.
| Characteristics | No. (%) |
|---|---|
| Demographic data | |
| Male | 308 (79.4) |
| Female | 80 (20.6) |
| Sport category | |
| Powera | 200 (51.5) |
| Enduranceb | 7 (1.8) |
| Team Sportsc | 151 (46.6) |
| Sport Discipline | |
| Dragon Boat | 48 (12.4) |
| Basketball | 46 (11.9) |
| Kabaddi | 34 (8.8) |
| Wushu | 34 (8.8) |
| Volleyball | 22 (5.7) |
| Jujitsu | 21 (4.4) |
| Wrestling | 19 (4.9) |
| Taekwondo | 18 (4.6) |
| Archery | 16 (4.1) |
| Karate | 15 (3.9) |
| water polo | 13 (3.4) |
| shooting | 12 (3.1) |
| Others | 90 (23.19) |
| Total | 388 (100) |
| History findings | |
| Smoking | 9 (2.3) |
| Dizziness | 43 (11.2) |
| Faint | 8 (2.09) |
| Chest wall pain | 21 (5.6) |
| Anemiad | 28 (7.4) |
| Death of Female Family Member under 65 | 11 (2.8) |
| Death of Male Family Member under 55 | 23 (6) |
| Palpation | 49 (13.1) |
| Extra sound (described by athlete) | 8 (2.1) |
aWeightlifting, Wrestling, Wushu, Karate, Taekwondo, Boxing, Judo, Jujitsu.
bDragon Boat, Cycling, Distance Running, others.
cVolleyball, Basketball, Kabaddi, Water polo.
dAnemia is a medical condition in which the red blood cell count or hemoglobin is less than normal. For men, anemia is typically defined as hemoglobin level of less than 13.5 g/100 mL and in women as hemoglobin of less than 12.0 g/100 mL.
| Characteristics | No. (%) |
|---|---|
| Physical Exam Finding | |
| Murmur | 11 (3.1) |
| ECG Findings Axis | |
| NL | 380 (97.9) |
| Right Deviation | 4 (1) |
| Left Deviation | 4 (1) |
| Left Ventricular hypertrophy | 12 (3.1) |
| Atrial hypertrophy | 3 (8) |
| Heart block | |
| block level 1 | 35 (11.6) |
| Branch block | |
| RBBB | 38 (9.7) |
| Sinus Rhythm | |
| Bradycardia | 124 (32) |
| Tachycardia | 5 (1.3) |
| Arrhythmia | |
| PVC | 2 (0.5) |
| WPW | 1 (0.3) |
| T change | |
| T invert | 6 (1.5) |
| Jpoint elevation | 17 (4.4) |
Two athletes (0.5%) suffered from asthma, and in 8 persons (2%) who didn’t have any other cardiovascular symptom, cardiac murmur was reported. Based on physical examination 11 athletes (2.8%) had heart murmur. Investigation of their ECG showed that there was not any evidence of right ventricular hypertrophy in athletes while 12 sportsmen (3%) had signs of left ventricular hypertrophy. First degree heart block was detected among 45 (11.6%), and there was nobody with second degree heart block. Right bundle branch block (RBBB) was shown in 38 (9.8%) but nobody had left bundle branch block (LBBB). Only 2 (0.5%) of them had arrhythmia which was benign premature ventricular contraction (PVC) according to their ECG. Six sportsmen (1.5%) had inverted T wave in v1 and v2 leads and nobody had long corrected Q-T interval.
Regarding to the distribution of symptoms among various sports disciplines, water polo players had the highest rate of chest wall pain compliant (30.8% of athletes). The highest rate of palpitation was reported among weightlifters with (40%) and after that were shooting (25%) and water polo (23.1%). Regarding the physical examination, highest resting heart rate belonged to soccer players (64.2% of them had heart rate above 75/min) and lowest heart rate was for water polo players (23.3% had heart rate below 50/min) (Table 3).
| Quantitative Parameters | Mean (SD) | Range |
|---|---|---|
| Heart rate | 66 (8.4) | 48 - 91 |
| Respiratory rate | 12 (1.07) | 10 - 15 |
| Blood pressure max | 11.1 (1.1) | 9 - 15.6 |
| Blood pressure min | 7.1 (0.8) | 5 - 10 |
There was not any significant relation between ECG changes and variables including sports discipline, history of hypertension, history of lightheadedness, vertigo, unconsciousness, chest pain, history of death below age of 65 in female and 55 in male family members due to cardiovascular causes, metabolic disorders, palpitation, and exhaustion. There was a significant relation between gender and ECG changes (P < 0.0001) that means 58% of male athletes had ECG variations (which most of them were considered normal changes) but these changes are lesser in female sportspersons (13.8%) which have been shown in Tables 4 and 5. The mean age of athletes with and without ECG changes didn’t have any significant correlation (P = 0.201) which were 23 and 23.5 years old respectively.
| ECG Change | Total | P Value | ||
|---|---|---|---|---|
| No | Yes | |||
| Gender | < 0.0001b | |||
| Male | 128 (41.7) | 179 (58.3) | 307 | |
| Female | 69 (86.3) | 11 (13.8) | 80 | |
| Sport | 0.707c | |||
| power speed | 82 (45.8) | 97 (54.2) | 179 | |
| Endurance | 4 (57.1) | 3 (42.9) | 7 | |
| Team | 70 (49.6) | 71 (50.4) | 141 | |
| HTN history | > 0.99c | |||
| Yes | 1 (100.0) | 0 | 1 | |
| No | 194 (50.7) | 189 (49.3) | 383 | |
| Dizziness history | 0.339b | |||
| Yes | 19 (44.2) | 24 (55.8) | 43 | |
| No | 176 (51.9) | 163 (48.1) | 339 | |
| Light headedness | 0.608b | |||
| Yes | 7 (58.3) | 5 (41.7) | 12 | |
| No | 187 (50.8) | 181 (49.2) | 368 | |
| Faint history | > 0.99c | |||
| Yes | 4 (50.0) | 4 (50.0) | 8 | |
| No | 191 (51.2) | 182 (48.8) | 373 | |
| Chest pain | 0.453b | |||
| Yes | 9 (42.9) | 12 (57.1) | 21 | |
| No | 181 (51.3) | 172 (48.7) | 353 | |
| Dead 55 maled | 0.446b | |||
| Yes | 10 (43.5) | 13 (56.5) | 23 | |
| No | 185 (51.7) | 173 (48.3) | 358 | |
| Dead 65 femaled | 0.323b | |||
| Yes | 4 (36.4) | 7 (63.6) | 11 | |
| No | 190 (51.5) | 179 (48.5) | 369 | |
| Metabolic historye | 0.98b | |||
| Yes | 27 (51.9) | 25 (48.1) | 52 | |
| No | 164 (51.7) | 153 (48.3) | 317 | |
| Tired history | 0.892b | |||
| Yes | 18 (50.0%) | 18 (50.0) | 36 | |
| No | 172 (51.2%) | 164 (48.8) | 336 | |
| Palpitation | 0.753b | |||
| Yes | 24 (49.0%) | 25 (51.0) | 49 | |
| No | 166 (51.4%) | 157 (48.6) | 323 | |
| Extra sound history | 0.007c | |||
| Yes | 8 (100.0) | 0 | 8 | |
| No | 182 (50.0) | 182 (50.0) | 364 | |
| Age | 0.201f | |||
| Mean (SD) | 22.96 (4.44) | 23.54 (4.32) | ||
| Median (Range) | 23 (16 - 36) | 23 (16 - 36) | ||
aValues are expressed as No. (%).
bMann-Whitney U test.
cKruskal-Wallis Test.
dFamily history of early coronary heart disease (heart attack, stroke percutaneous coronary catheter interventional procedure, CABG, treated angina or SCD) in a first-degree family in a female parent or sibling before age 65 years or a male parent or sibling before age 55 years.
eThe metabolic syndrome refers to the accompaniment of several cardiovascular risk factors, including: atherogenic dyslipidemia, obesity, insulin resistance and hypertension.
fSpearman’s rho.
| Regression Coefficient | S. E. | Chi Square | P Value | OR | |
|---|---|---|---|---|---|
| Age | 0.006 | 0.029 | 0.039 | 0.844 | 1.006 |
| Gender | |||||
| Male | 1.975 | 0.369 | 37.301 | < 0.0001 | 7.213 |
| Female | |||||
| Sport | |||||
| Power-Speed | 0.330 | 0.249 | 1.805 | 0.179 | 1.391 |
| Endurance | -0.323 | 0.792 | 0.191 | 0.662 | 0.724 |
| Team | |||||
| HTN history | |||||
| Yes | -1.712 | 2.542 | 0.885 | 0.347 | 0.181 |
| No | |||||
| Dizziness history | |||||
| Yes | -0.182 | 0.392 | 0.23 | 0.632 | 0.833 |
| No | |||||
| Light headedness | |||||
| Yes | -0.041 | 0.837 | 0.003 | 0.957 | 0.959 |
| No | |||||
| Faint history | |||||
| Yes | -0.519 | 1.091 | 0.277 | 0.599 | 0.595 |
| No | |||||
| Chest pain | |||||
| Yes | 0.069 | 0.541 | 0.018 | 0.894 | 1.072 |
| No | |||||
| Dead 55 male | |||||
| Yes | 0.207 | 0.511 | 0.179 | 0.672 | 1.23 |
| No | |||||
| Dead 65 female | |||||
| Yes | 0.559 | 0.702 | 0.735 | 0.319 | 1.75 |
| No | |||||
| Metabolic history | |||||
| Yes | 0.397 | 0.354 | 0.013 | 0.909 | 1.04 |
| No | |||||
| Tired | |||||
| Yes | 0.316 | 0.435 | 0.556 | 0.456 | 1.372 |
| No | |||||
| Palpitation | |||||
| Yes | 0.118 | 0.364 | 0.11 | 0.740 | 1.126 |
| No | |||||
| Extra sound history | |||||
| Yes | -2.307 | 1.661 | 3.874 | 0.049 | 0.099 |
| No |
In accordance to Table 6 and Figure 1, it is shown that clinical signs and symptoms could not be used as predictors for ECG changes (P = 0.863).
| Parameters | Results |
|---|---|
| Area under the ROC curve (AUC) | 0.505 |
| Standard Error | 0.0289 |
| 95% Confidence interval | 0.450 to 0.560 |
| Z statistic | 0.173 |
| Significance level P (Area = 0.5) | 0.8627 |
5. Discussion
As above mentioned, two purposes were followed in this study; to determine prevalence of cardiovascular disorders among athletes participating at Asian games and answering the question whether an electrocardiogram (ECG) is a necessary part of pre-participation examination (PPE) for prevention of sudden cardiac death. In other words, the current study was to find any correlation between ECG changes and cardiovascular signs and symptoms. In Iran there are diverse standards for pre-participation examination. For example for school level athletes PPE includes of history taking and physical examination but for professional and championship level athletes the PPE consists of ECG and some blood and urine tests in addition to history taking and physical examination. Sometimes in accordance to level and number of athletes, echocardiography is also performed for them. Among various reasons for performing examinations, predicting and prevention of sudden cardiac death is very important due to its incidence. While the incidence of SCD is low and reported only about 90 annually in United States (39) but regarding the importance of athletes’ health, PPE is performed in accordance to 26th Bethesda conference (40, 41) which is emphasized on family history and examination and there is not any clear recommendation for performing ECG (42). Based on American heart association (AHA) guidelines the most effective and cautious method of screening for detecting cardiovascular abnormalities, is history taking and physical examination (43). In Italy taking ECG is required for all athletes prior to participation at sports events (42). In Veneto region of Italy, performing this guideline resulted in 89% decrease of sudden death among athletes (29). European society of cardiology also recommended ECG in European countries for cardiovascular disorder screening (44).
International Olympic committee (IOC) also recommended ECG for athletes participating in Olympic games. For screening of SCD, 42 Diversity of methods and strategies around the world is due to different common causes of sudden cardiac death in various countries. In USA the most common cause of SCD is hypertrophic cardiomyopathy, but in Italy arrhythmogenic right ventricular cardiomyopathy is the most common cause of it (9, 29, 39, 45). Wheeler et al showed that performing ECG is both cost effective and diagnostic for SCD (42). In our current study and regarding to the results we concluded that there is not any correlation between positive signs and symptoms and ECG changes. On the other hand the cost of taking ECG is lesser than 5 US$, therefore ECG could be considered as a mandatory part of PPE. Although there is not any consensus about the PPE (24) and more studies are recommended in accordance to application of different methods, their costs and efficacies (46). Performing echocardiography is still expensive (47), controversial and needs more investigations.
While 2.3% of athletes were smokers and their average age was 4 years more than mean age of all athletes, regarding the increase of cardiovascular disorders’ risk, the educational programs could be conducted for confronting this problem.