1. Background
According to the world health organization (WHO), cardiovascular diseases are the number one cause of death in the world (1). It is responsible for nearly 17.5 million deaths in 2012, representing 31% of all global deaths. Physical inactivity a major cause of cardiovascular diseases (1). Primary prevention is the first line of battle against cardiovascular disease prevalence in healthy populations. In the last decades, empirical scientific evidence has proved the role of exercise in the prevention of cardiovascular events in healthy people. For example, Myers et al. revealed a strong inverse relationship among exercise capacity assessed by treadmill and 6-year mortality in both 2534 normal healthy individuals and 3679 CVD patients (2). Interestingly Nocon et al. relying on a systematic review and meta-analysis of 883 372 partakers of 33 cohort studies, revealed a 35% risk reduction for CVD mortality and 33% risk decrement for all-cause mortality by physical activity (3).
Cardiovascular wellness depends on a variety of molecular and behavioral variables, amongst which exercise has a remarkable impact. The cardiovascular system responds to different modalities of exercise, especially resistance exercise (RE) in a coordinative and integrated manner to ensure that sufficient blood is delivered to working muscles (4). However cardiovascular and especially hemodynamic responses to RE are much less studied than its responses to aerobic exercise (5) as traditionally it had not been accepted that this designed regime of exercise can improve cardiovascular health (4).
RE increases the development and maintenance of strength, muscular endurance, and muscle hypertrophy (6, 7). However, some individuals cannot be subjected to high-intensity RE due to several health problems and therefore cannot train with heavy loads (> 70% of 1RM), which are otherwise recommended for increasing strength and hypertrophy in weak but healthy people (6). Accordingly, low-intensity (LI) RE combined with blood flow restriction (BFR) can be utilized for these individuals because this method uses low loads (20% - 30% 1RM) combined with a tourniquet, which reduces the negative effect of heavy loads on the joints (8-10). In addition, this method seems to be safe in terms of cardiovascular and hemodynamic responses (11-15).
Currently there is some information that suggests LI RE with BFR may modulate cardiovascular and hemodynamic responses such as heart rate (HR) (14-18), systolic and diastolic blood pressure (14-18), mean arterial pressure (MAP) (14), rate pressure product (RPP) (14), oxygen saturation (SpO2) (14), and rate of perceived exertion (RPE) (14). However, the acute effects of eccentric RE on cardiovascular and hemodynamics responses are not yet fully understood.
2. Objectives
The aim of the present study was to investigate the acute effects of LI eccentric RE with and without BFR on HR, RPP, blood pressure (BP) parameters (systolic, diastolic, and MAP), SpO2 and RPE.
3. Methods
In a semi-experimental study, a sample of sixteen recreationally active volunteer male students from Baqiyatallah University of Medical Sciences (Tehran, Iran) were selected after completing a general health questionnaire and anthropometric tests in this research (Table 1). Sample size of 16 subject was calculated using the G*Power 3.1 the current power of 0.80, α = 0.05, and an effect size (ES) of 0.30, based on processes suggested by Beck (2013) (19). Subjects were included in study if they had body mass index < 30 kg/m2, resting heart rate < 95 beat per minute, rest levels of blood pressure < 140/90 mmHg, young men aged < 32 years, and no history of participating in regular resistance or aerobic exercise in at least six months prior to the study. Individuals who had some type of musculoskeletal injury of the upper limbs, and were self-declared to be a smoker were excluded.
| Groups | Age (year) | Height (m) | Weight (kg) | BMI (kg/m2) | Body Fat (%) |
|---|---|---|---|---|---|
| +BFRRE (n = 10) | 25.50 ± 3.74 | 1.77 ± 0.61 | 74.39 ± 8.16 | 23.77 ± 1.92 | 14.24 ± 4.93 |
| -BFRRE (n = 6) | 27.33 ± 3.01 | 1.77 ± 0.58 | 66.73 ± 11.92 | 21.17 ± 2.5 | 13.87 ± 5.72 |
| P value | 0.31 | 0.99 | 0.11 | 0.18 | 0.69 |
BMI, body mass index; +BFRRE, eccentric resistance exercise with blood flow restriction; -BFRRE, eccentric resistance exercise.
aData represented as mean ± SD.
Participants were fully informed about the purpose, risks and discomforts associated with each experimental protocol. Subjects read and signed the detailed form of consent. All protocols in this study conformed to the Declaration of Helsinki and to current local guidelines approved by Baqiyatallah University of Medical Science Local Ethics Advisory Committee (protocol No. 340/3/6770). Participants were blinded about design groups. All exercises were accomplished in national sport medicine federation rehabilitation lab (Tehran, Iran) between 9 to 11 a.m. each day.
During the first visit to the laboratory, at least 5-7 days before the main exercise session anthropometric assessments such as height (Seca 217. Stable stadiometer, Germany), weight to the nearest 0.1 kg, body mass index (BMI), and total body fat percent (used body composition analyzer, Tanita BC-418 Korea), and maximal voluntary contraction (MVC) were calculated as described below.
At the first laboratory visit, Knee extensor MVC was measured using an isokinetic dynamometer (Humac norm, Cybex, TN, UK) (20). All of participants had ~5 minute warm up by stationary bike (Technogym Italy) into 50 - 60 rpm before each test session (20, 21). Then, participants were placed on the seat of the isokinetic while physiologic axis of knee joint which passes through the lateral femoral condyle coincided with the mechanical axis of the dynamometer at knee extension position. The hip and thigh were carefully fastened to the seat, while the lower leg was attached to the dynamometer lever arm 2 cm above the medial malleolus. Each test session started with 5 submaximal isometric contractions as the trial. After 20 seconds rest, continued with three isometric terminations in maximal effort at 30 degrees of knee flexion angle. Participants were instructed to push their legs into extension direction strongly as high as possible and hold it 5 seconds with 30 seconds rest between each termination. Verbal encouragement and online visual feedback of the exerted force was provided. All terminations with visible countermovement contractions were disregarded and repeated (20). The termination with highest MVC was selected for further analysis. Thirty percent of highest MVC calculated and considered as personal exercise load in exercise session.
Unilateral knee eccentric resistance exercise of quadriceps muscle was used to assess the acute cardiovascular and hemodynamic response to low intensity ECCRE with and without BFR. At the main exercise session, participants were invited to the research center of national sport medicine federation and performed 4 sets of resistance exercise that were executed with 30 % of the individuals’ highest MVC. Participants were divided randomly in two experimental groups with online randomization software (https://www.sealedenvelope.com/simple-randomiser/v1/lists), blocking methods and unequal block size: low intensity (30% maximal voluntary contraction (MVC)) eccentric RE alone (ECC RE n = 6) and low intensity (30% MVC) ECC RE combined with BFR (ECC RE BFR, n = 10). BFR was applied with pneumatic cuff (13 cm width) (Komprimeter Riester®, Jungingen, Germany) (14, 22). Restriction pressure of 90 - 100 mmHg, was selected for the restriction stimulus based on previous studies (23, 24). Occlusion was maintained throughout the entire exercise session, for a total time of ~ 6 min (339.9 ± 45 sec) and at the end, belt pressure was released immediately upon completion of the session. Since all exercise contractions were designed to be low intensity eccentric resistance (LI ECC-RE), the proper acronym only included the perfusion differences (+BFRRE: ECC - RE BFR, -BFRRE: LI ECC - RE).
Protocol was set on isokinetic mode of dynamometer with concentric-eccentric muscle actions (the concentric ‘lifting’ phase followed by the eccentric ‘lowering’ phase). Load was considered ~ 0 in concentric phase of movements (to reach this purpose assistant turned back the lever arm in full knee extension passively), and 30% of highest MVC in eccentric phase of movements. Participants started in full knee extension position and pushed up their leg to resist against lowering motion of isokinetic lever arm at frequency of 15 contractions per minute (rate of 2 seconds concentric and 2 seconds eccentric muscle actions), as the movements were performed smoothly.
Heart rate (HR), systolic/diastolic blood pressure, and blood oxygen saturation were measured before and after each set of exercise, RPP, and rate of perceived exertion (RPEs) assessed aftewards as described below.
Heart rate and oxygen saturation was measured at rest and after each set with Polar (Polar, T31 Kempele, Finland) and wrist pulse oximeter (Beijing, MD300W11, China) respectively. Blood pressure was measured in the seated position using an automatic pneumatic blood pressure machine with an appropriate sized cuff (Roosmax, Model ME701, Switzerland) (25). Mean arterial blood pressure (MAP) as index of driving pressure that determines the amount of blood flow through the body (26) was calculated by using the following formula:
MAP = 1 / 3 (SBP - DBP) + DBP
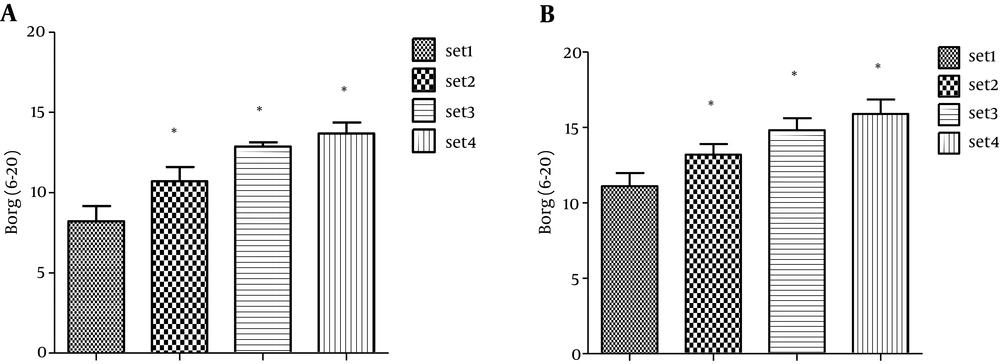
Rate of perceived exertion (RPE) assessed with the Borg, 6 - 20 scale (27, 28). RPE was assessed after each set of the exercise sessions.
Rate of pressure product was calculated as index of myocardial oxygen consumption according to this formula: RPP = [HR × SBP] / 100
Data were analyzed by SPSS 16 software, using two-way analysis of variance (ANOVA) with repeated-measures [trials (+BFR-RE vs. -BFR-RE) × time (rest vs. set 1-4)]. Post-hoc testing was performed using Tukey’s test when a significant F value was detected. Wilcoxon test was used for assessment of RPE variation. All data are represented as mean ± SD and statistical significance was set at P ≤ 0.05.
4. Results
The physiological characteristics of participant verified no significant differences between the two groups in baseline measured variables values (Table 1). The results of within groups set comparison analysis for HR, SpO2, SBP, DBP, MAP, RPP and RPE is presented in Table 2 and Figure 1, respectively. The HR increased significantly after both LI ECC-RE with and without BFR (P < 0.05). Analysis of the first and fourth data sets indicated that the HR was significantly elevated in pre-versus post-exercise periods in both groups (P < 0.05). Whereas, in sets exercised ECC-RE with BFR, HR was significantly upraised after first and third sets (P < 0.05, Table 2).
| Variable | HR (bpm) | SpO2 | SBP (mmHg) | DBP (mmHg) | MAP (mmHg) | RPP% |
|---|---|---|---|---|---|---|
| ECCRE 30% MVC | ||||||
| Rest | 76.11 ± 10 | 94.39 ± 1.02 | 121 ± 11.77 | 76.51 ± 7.74 | 98.77 ± 8.46 | 91.92 ± 12.48 |
| 1st set | 83 ± 18.9 | 93.17 ± 3.71 | 124.8 ± 12.92 | 85.83 ± 7. 25 | 105.33 ± 9.91 | 102.39 ± 19.89 |
| 2nd set | 82.21 ± 15.25 | 94.17 ± 2.14 | 117 ± 7.24 | 80 ± 11.36 | 98.50 ± 7.66 | 96.77 ± 21.3 |
| 3rd set | 80 ± 14.31 | 93.83 ± 1.16 | 118 ± 15.3 | 83.17 ± 8.4 | 100.58 ± 11.03 | 96.07 ± 20.46 |
| 4th set | 85.33 ± 9.4b | 93.33 ± 1.50 | 127.2 ± 9.68 | 90.85 ± 15.84 | 109.02 ± 11.77b | 108.75 ± 16.22b |
| ECCRE with BFR 30% MVC | ||||||
| Rest | 85 ± 10.48 | 94.30 ± 1.98 | 119.78 ± 8.77 | 80.6 ± 9.01 | 102.01 ± 8.36 | 102.20 ± 17.60 |
| 1st set | 97 ± 16.98b | 95.3 ± 3.3 | 131 ± 8.37b | 87.6 ± 6.92b | 109.31 ± 7.31b | 127.55 ± 26.32b |
| 2nd set | 93.5 ± 18.83 | 94.5 ± 3.78 | 126.4 ± 8.02b | 88.2 ± 10.77b | 107.3 ± 9.09b | 119.12 ± 29.72b |
| 3rd Set | 93.4 ± 14.81b | 95.80 ± 2.54 | 127.56 ± 9.95b | 84.6 ± 11.4 | 106.08 ± 9.96 | 121.26 ± 22.11b |
| 4th set | 94.6 ± 14.07b | 95.5 ± 2.43 | 120.8 ± 13.56 | 84.8 ± 15.2 | 102.81 ± 13.19 | 114.52 ± 21.98 |
HR, heart rate; bpm, beat per minute; SpO2, blood oxygen saturation; SBP, systolic blood pressure; DBP, diastolic blood pressure; MAP, mean arterial pressure; RPP, rate pressure product; ECC, eccentric resistance exercise; ECCRE with BFR, eccentric resistance exercise with blood flow restriction.
aData represented as mean ± SD.
bSet were significantly different compare to rest, (P < 0.05).
The within groups analysis indicate that SBP just increased significantly in volunteer post sets 1, 2 and 3 of ECC RE with BFR (P < 0.05). Similarly, DBP raised in + BFR group but only in sets 1 and 2 (P < 0.05). The comparative analysis of data indicates that MAP increased significantly after exercising without BFR (P < 0.05).
Our findings of comparative tests showed no remarkable change in SpO2, neither within nor in between groups (P > 0.05). The results of between group analyses of RPP indicate no significant differences of RPP at any time (P = 0.08). However, within group analysis showed that RPP increased significantly in pre-versus post-exercise in freely perfused eccentric RE group, and in first three sets with BFR (P < 0.05).
Present results depict that the RPE changed significantly within both groups (P < 0.05, Figure 1). However between groups comparative analyses showed no significances differences for all of evaluated parameters (P > 0.05).
5. Discussion
The present study investigated cardiovascular and hemodynamic responses and RPE of LI ECCRE with and without BFR. To our knowledge this is the first study that evaluated the acute effect of eccentric RE combined with BFR on hemodynamic and cardiovascular parameters and perceived exertion. The main findings of this study were: a) HR and RPE increased significantly in both groups; b) SBP and DBP increased significantly only with BFR; c) MAP and RPP increased significantly following exercising without BFR; d) no change in SpO2 in both groups, however, there were no differences between groups for any of evaluated parameters.
In the present study HR increase modestly whereas blood pressure remains unchanged. Increase in HR was observed in previous studies (14, 16, 17), while Yasuda et al. (29) reported no increase in the HR after BFR RE.
The alteration of HR following the onset of an exercise could be related to mode of exercise, as Featherstone et al. (30) reported less increase in HR after various load of weight lifting exercise (40, 60, 80 and 100% of MVC) (HR ranged from a low value of 74 to a peak of 92 bpm) in compare with the tre admill exercise (hiting157 bpm).
In the present study HR rose from a baseline value of 75 to high value of 94, very similar to what Neto et al. (31) reported. Most studies reported modest increase of heart rate during resistance exercise to volitional fatigue (4, 32). Still higher value of HR increase has been reported; however, they are frequently reported. In a single study the came across the heart rate went up to maximum 170 beat/min but during bilateral and unilateral lift of upper and lower body with 80%, 90%, 95%, and 100% of maximum weight equivalent (4, 33).
It therefore appears that muscle groups engaged during exercise may play an important role in determining the extent of HR response variation to BFR, along with other HR accompanying factors, as Yasuda et al. (29) reported HR increases to a higher magnitude during leg press BFR RE in comparison with knee extensor BFR RE. Loenneke et al. (8) found no significant differences in HR between the LI+BFR vs LI sessions of bilateral knee extension to 30% of 1RM with 1 second (CON/ECC) speed up to exhaustion. In the LI+BFR protocol, individuals trained with narrow elastic bands of 7.6 cm width, where the pressure cannot be verified. Therefore, a modest rise in HR in present study where knee extensors were recruited unilaterally well fits the spectrum of results reported in current literature.
Although no study has verified the acute effect of eccentric RE with BFR in terms of cardiovascular and hemodynamic responses, few studies have evaluated the effects after combined concentric and eccentric exercises (8, 32, 34). Our findings corroborate those studies in which the authors found no significant differences between the protocols that performed the LI training with or without the BFR.
Although results of set analysis showed that MAP and RPP were elevated after both regimes of exercise, interestingly, pre to post-test comparison analysis revealed that MAP and RPP increased significantly per se following LI ECC RE. Increases in RPP as index of myocardial oxygen consumption subsequent to this modality of exercise means that the heart did more work during LI ECC RE in comparison with BFR RE. However, between groups comparison indicated that MAP and RPP changes did not significantly differ amongst groups.
In accordance to our results Figueroa and Vicil (34) observed no significant differences between the RE protocols with and without the BFR on HR, SBP, DBP, and MAP. The authors submitted the volunteers at sessions of exercises knee flexion and extension (bilateral) at 40% of 1RM, being performed three series to exhaustion with one minute interval between sets. The protocol LI + BFR, subjects trained with a sphygmomanometer (Unknown width) set at 100 mm Hg pressure. Neto et al. (31) subjected 24 men to three exercise protocols (HI, LI, LI + BFR), who performed bilateral arm flexion and extension, and knee flexion and extension (agonist/antagonist) RE. The authors used a restriction pressure of 93 mm Hg to arms and 108 mm Hg to the legs. They found an increase in HR and RPP within all three groups, but no differences between them. Comparing the findings of the three studies with one another and also with the present study, we observed that whatever the form of execution (concentric and eccentric vs eccentric) if the exercises are performed to exhaustion all at the same volume, it seems that there will be an increase in hemodynamics immediately after exercise, but without significant differences, which emphasizes the safety of these modalities of exercise, since the hemodynamic is elevated in proportion to the LI without the BFR.
Additionally, the responses of hemodynamic and cardiovascular variables may have been influenced by muscle tension associated with the strangulation of blood vessels induced by BFR. Thus, the BFR may have stimulated the muscle mechanoreceptors and tendon (35), which might justify an increase in blood pressure (36).
In relation to SpO2, our findings differ from the study performed by Neto et al. (31) that found significant reductions in the LI protocols with (Δ = - 1.13%) or without (Δ = - 0.92%) BFR. This may be related to the amount of exercise and muscle groups involved (one vs four), the form of contraction (eccentric vs concentric and eccentric) and time under tension were higher in the study performed by Neto et al. (31). However, the reduction in oxygen saturation observed in the study by Neto et al. (31) may have altered the supply of intramuscular oxygen, providing a more acidic ambient and an anabolic environment (28), a fact that could justify a higher RPE (extension and flexion of knees) in the protocol LI + BFR when compared to HI. In the present study there was no reduction in SpO2 probably because eccentric contraction was performed in only one exercise movement and one muscle group (ECC knee extension of quadriceps muscle). However, the RPE increased in both protocols, and it is speculated that as the eccentric contraction generates larger muscle damage after exercise, the stress imposed on the muscles is very high which provided a significant increase in RPE. In addition, it is observed that some studies have reported the effect of RE with BFR on the RPE (32, 37-39), but none of them evaluated the effect of eccentric RE on RPE.
In conclusion, although both LI ECC RE with and without BFR induces substantial increment HR and RPE, but it seems that the cardiovascular system has to work more in response to LI ECC RE. Hearts have to eject blood against modest increase in MAP seen with LI ECC RE; consequently it could enhance RPP following this mode of exercise, whereas MAP and RPP fluctuate at normal range in response to BFR RE. Therefore, it seems that BFR RE is safe and optimum option regarding the hemodynamic and cardiovascular system in healthy populations. However, application of these protocols in clinical treatment needs more studies.