1. Background
Lateral ankle sprain is the result of a supination torque that excessively loads the lateral structures of the ankle (1). Up to 70% of people who experience an initial ankle sprain will develop chronic ankle instability (CAI), defined as repetitive giving way or feeling of instability that may involve both functional and mechanical deficits (2). Several researchers have found weakness and changes in muscle activation in the hip in subjects with ankle instability and anterior knee pain (3-5). This finding points to the importance of assessing beyond the site of injury through sensorimotor chains. The muscles of the hip, particularly the gluteus medius (G-Med) and gluteus maximus (G-Max) are involved with positioning of the femur which, through the kinetic chain, affects the positioning of the tibia, and subsequently the ankle joint. The increase in G-Max activity prior to landing may suggest the need to position the foot under the base of support, moving it into slight hip extension. G-Med dysfunction is a common cause of insufficient hip abduction and external rotation strength that is often associated with decreases in postural control that is very important to prevent from lower extremity injuries (5). Another factor that is very important in sport injuries is fatigue. Fatigue has been proposed to desensitize muscle spindles and the afferent pathways to the central nervous system, slowing the response and number of muscle fibers needed to handle the perturbations. This impact on the central nervous system increases the predisposition to injury (6).
Unfortunately, although the effects of fatigue have been evaluated frequently in the literature, no existing models assess the effect of gluteal muscles fatigue on functional performance testing in subjects with and without CAI. Therefore, the purposes of this study were 1) to assess group differences in functional performance testing 2) to assess the differences of functional performance testing between the two times (pre and post gluteal muscles fatigue) and 3) to assess the effect of gluteal muscles fatigue on static and dynamic balance.
2. Methods
2.1. Participants
We recruited 24 physically active participants from basketball, volleyball and football teams. Participants were separated into 2 groups: 12 with CAI (12 females; mean ± SD, age; 22 ± 3.8 years; height, 168.7 ± 3.8 cm; body mass, 62 ± 4.7 kg) and 12 control subjects (12 females; mean ± SD age, 21.3 ± 3.7 years; height, 165.2 ± 5.2 cm; body mass, 62.7 ± 10.3 kg). In the CAI group, 12 subjects were recruited with previous history of ankle injury which caused limping or pain for at least 24 hours. Since the time of the initial injury, subjects in the CAI group reported having at least two episodes of the ankle “giving way”, in six the months preceding testing. At the time of testing, patients were able to perform normal activity with no pain and scored 89% or lower on the foot and ankle disability index (FADI) and/or 84% or lower on the FADI-Sport (7). They were excluded from both groups if they had history of lower extremity fracture, lower limb surgery, injury to knee or hip or low back injury. An informed consent was taken from all athletes prior to testing. The study was approved by Razi university ethical committee.
2.2. Procedures
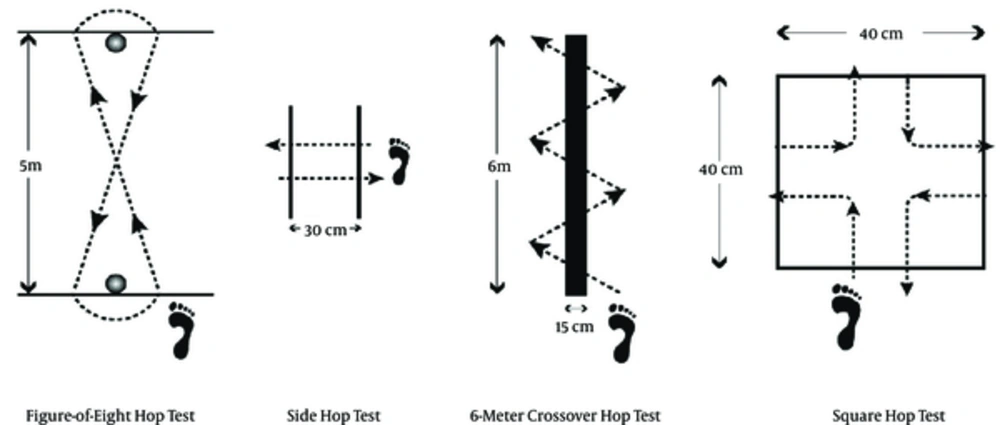
In this semi experimental study, each participant performed a 10-minute warm-up with jogging, running and jumping activities; then 24 participants completed 4 functional performance tests, the figure-of-8 hop, side hop, 6-meter crossover hop, and square hop. Before testing, each test was demonstrated along with verbal instructions. To familiarize themselves with the experimental protocol, the participants then performed three trials each of the 4 functional performance tests. Time was recorded using a hand-held stop-watch to the nearest 0.01 seconds. The limb was matched between the CAI and control groups. For the figure-of-8 hop test, a 5-m course outlined by cones was used (Figure 1). Each participant was instructed to hop on 1 limb, twice around the course, as fast as possible. We marked any trials in which a participant put the contralateral foot down, fell, missed the stopwatch pad, or did not complete the course as outlined as unacceptable and asked to perform the trial again. Reliability for this test was reported excellent by Caffrey et al., (2009), with an intraclass correlation coefficient (ICC) of 0.95. For the side hop test, all participants were instructed to hop on 1 limb laterally over a 30-cm distance (Figure 1). One repetition constituted hopping laterally 30 cm and back to the starting location. Each participant completed 10 repetitions and was instructed to do so as quickly as possible. If a participant fell, put the contralateral foot down, missed the stopwatch pad, or did not completely clear the 30-cm distance while hopping the trial, we recorded the trial as unacceptable and the participant repeated the trial again. Again, trial reliability was reported well by Caffrey et al., with ICC2 of 0.84. In the 6-meter crossover hop test, a line 6 m long was used. The participants were instructed to hop on 1 limb diagonally over the 15-cm-wide line, alternating sides for the entire 6 m, as fast as possible (Figure 1) (8). We recorded a trial as unacceptable if the participant put the contralateral foot down, fell, missed the stopwatch pad, or did not completely clear the width of the line. The trial was repeated if not acceptable. Trial reliability for this test was reported excellent, with an ICC2 of 0.96. The square hop consists of a 40 × 40-cm square marked on the floor with tape (Figure 1). Starting outside of the square, participants were instructed to hop in and out of the square as fast as possible for 5 repetitions. One repetition constituted hopping in and out of the tape outline completely around the square back to the starting point. With the right limb, participants hopped in a clockwise direction and, with the left limb, they hopped in a counterclockwise direction. When a participant fell, put the contralateral foot down, hopped in the wrong direction, missed the stopwatch pad, did not completely clear the outline of the tape on the right and left sides of the square, or did not clear the outline of the tape on the top and bottom of the square with the balls of the feet, we marked the trial as unacceptable and the participant repeated the trial. Trial reliability for this test was reported well, with an ICC of 0.90 (8, 9).
Static and dynamic balance was analyzed by Romberg and Y test that are valid tests and have high reliabilities 0.85 - 0.91 (10).
2.3. Fatigue Protocol
First 1 - 5 minute submaximal running, second 8-repetition hip abduction with hip 60 at degrees and knee at 90 degrees. 8-repetition side-lying hip abduction subjects were positioned side-lying on the floor, in a starting position of full knee extension and neutral hip position. Subjects slowly abducted the hip from the top. 8-repetition single-limb squat subjects started the squat by balancing on their purposed limb, with their knee and hip flexed approximately 30° and their hands on their hips. Subjects slowly lowered themselves toward the ground, using their ankle, knee, and hip joints, until they could touch their contralateral middle finger to the outside of their dominant foot without reaching with their shoulder. Subjects then returned to the starting position. 8-repetition lateral band walks with elastic band (resistance, 2.04 kg/30.5 cm of expansion) was tied around the subjects’ ankles while they stood upright with their feet together. During the exercise, the subjects maintained their knees and hips in 30° of flexion. Subjects kept their hands on their hips and began with their feet together. Next, subjects sidestepped leading with their purposed limb. 8-repetition multiplanar lunges were performed in the sagittal, frontal, and transverse planes. All 3 lunges started with the subjects standing with their feet near each other and hands on their hips. All lunges were performed with the purposed limb, keeping the trunk in an upright position, so that the knee and hip of the purposed limb flexed to 90°. Subjects were instructed to keep their knees over the toes for all lunges. 8-repetition multiplanar hops, similar to the lunges, were performed in the sagittal, frontal, and transverse planes. Subjects started in the same position of the lunges and hopped in the desired direction off the purposed limb and landed on the other limb. Subjects were instructed to land “as softly as possible,” with their knees flexed, and to keep their knees over their toes. In addition, they were asked to repeatedly abduct and extend the hip to 30 while in a side-lying position, with the knee fully extended. Then each participant was instructed to raise and lower the leg to this reference angle and afterwards extend to this reference angle at a pace of 60 beats per minute as provided by a digital metronome (model 96204X; Mel Bay Publications, Pacific, MO) until she reported a Borg perceived exertion scale rating of 19 or greater (on a 6 - 20 scale) and she failed to touch the bars. All functional tests and balance tests were done immediately after fatigue criteria were met (Borg perceived exertion scale and failed to touch the bar in 30 on 2 consecutive repetitions) again (11-13).
2.4. Statistical Analyses
Means and SDs were calculated for age, weight, height and all dependent measures. To identify performance differences, we used mixed-design 2-way (time × group) ANOVAs, 1 for each test, with time (pretest versus posttest) and groups (CAI versus control) as the independent factor. And we used independent sample t-test to identify performance differences in pretests and posttests. The alpha level for all analyses was P ≤ 0.05.
3. Results
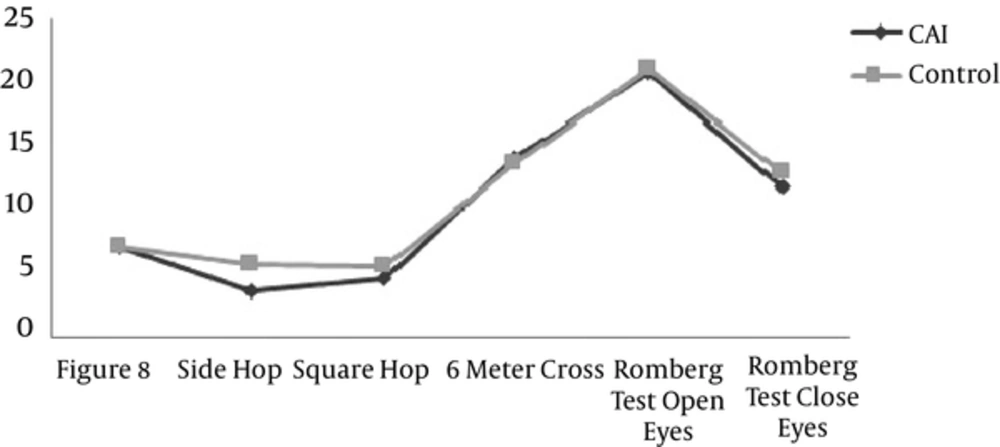
The results of this study didn’t show any significant differences between groups in pretest for all functional performance tests. The main effect of figure 8 test in pretest to post test was significant (F (1, 22) = 59.5, P = 0.0001), and partial eta square (effect size) was 0.73, but there was no significant differences between two groups (experimental and control) (F (1, 22) = 0.00: P = 0.98). The main effect of side hop test in pretest to posttest was significant (F (1, 22) = 32.9: P = 0.0005), and partial eta square was 0.60 as well. Significant differences were shown between two groups (F (1, 22) = 4.7, P = 0.04) and effect size was 0.17. The main effect of time for square hop scores was significant, (F (1, 22) = 102.5, P = 0.0001). With partial eta square 0.82. Also the intraction effect (time × group) was significant (F (1, 22) = 5.6, P = 0.02). In addition, the square hop scores for participants in the CAI increased from pre to the posttest, (F (1, 22) = 2.2, P = 0.02), But the square hop scores for participants in the control group didn’t significantly increase from the pre to posttest, (F (1, 22) =1.13, P = 0.06).
The main effect of time for 6 meter cross test in pretest to posttest showed significant differences (F (1, 22) = 38.3, P = 0.0005), and partial eta square was 0.63, but no significant differences between two groups (F (1, 22) = 0.23: P = 0.6).
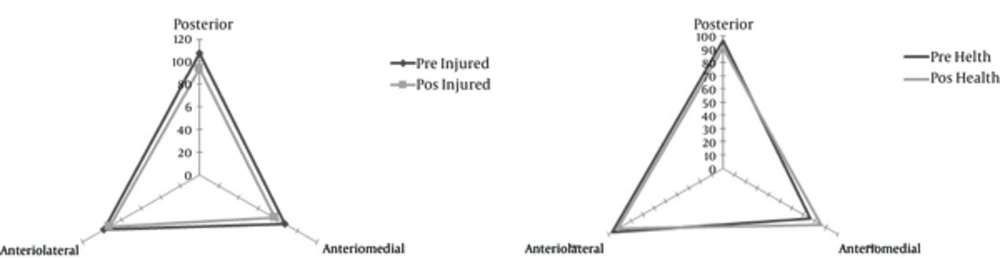
The results of independent sample t-test showed that in the posttest of all functional performance tests there wasn’t a significant difference between CAI and control groups except side hop (P = 0.016), (Table 1). Other results of this study showed that balance and control of posture is affected by the hip abductor muscles’ fatigue. Romberg scores for static balance testing in open eye situation in pretest to post test showed significant differences (F (1, 22) = 38.3: P = 0.0005), and partial eta square was 0.51, but there was no significant differences between two groups (F (1, 22) = 0.23: P = 0.5). But in closed eyes situation, the reduction on time to hold the test was the same as healthy subjects, as in pretest to post test there were significant differences (F (1, 22) = 51.5: P = 0.0005), and partial eta square was 0.70 but no significant differences between two groups (F (1, 22) = 0.1: P = 0.7). Y test scores in pretest to post test had significant difference (F (1, 22) = 20.4: P = 0.0005), partial eta square was 0.48, but there were no significant differences between two groups (F (1, 22) = 0.6: P = 0.4) (Figure 2). Also the results showed that CAI group was weaker in posterior direction, but the healthy group was weaker in anteriomedial direction.
| Variables | CAI Group | Control Group | ||
|---|---|---|---|---|
| Pre Test | Post Test | Pre Test | Post Test | |
| figure-8 | 5.7 ± 1.2 | 7.2 ± 1.3 | 5.8 ± 1.1 | 7.1 ± 1.1 |
| Side hop | 5.0 ± 2.1 | 6.8 ± 2.3b | 3.7 ± 1.1 | 5.7 ± 1.5 |
| Square hop | 5.2 ± 0.9 | 6.3 ± 1.4b | 2.2 ± 1.1 | 5.5 ± 1.3 |
| 6 meter cross | 11.2 ± 3.0 | 14.1 ± 3.7 | 10.2 ± 2.5 | 13.7 ± 4.6 |
| Romberg test open eyes | 20.9 ± 8.4 | 18.5 ± 8 | 21.1 ± 6.8 | 15.1 ± 7.7 |
| Romberg test close eyes | 11.9 ± 7.3 | 8.2 ± 4.6 | 13 ± 4.7 | 8.6 ± 4.1 |
| Y test | 108.24 ± 18.2 | 100 ± 13.8 | 118.27 ± 33.11 | 106.46 ± 30 |
aValues are expressed as mean (SD).
bValue increased compared with control group (P < 0.05).
4. Discussion
Hip-muscles weakness has been indicated as a risk factor for lower extremity injuries such as patelofemoral pain syndrome, medial tibial stress syndrome, ACL tearing etc (5). The purpose of this study was to investigate the effect of hip abductor and extensor fatigue on ankle functional performance and balance in subjects with and without CAI. We observed, after a gluteal muscles fatigue protocol, ankle functional performance of participants in two groups (ankle instability group and healthy group) was defected, as we saw increased time of all functional performance tests and decreased balance scores. But we observed that just in two tests (side hop and square hop tests) of all functional performance tests there was significant differences between CAI and control groups that were in agreement with the results of Webster, Bullock and Buchanan that found changes in hip muscle latency for subjects with unilateral CAI, utilizing inversion perturbations as an intervention (3-5). The results of prior studies reported that most of ankle sprains occur during landing and cutting tasks (14, 15). Results of this study also indicate that two of the functional tests which had side hopping (side hop and square hop tests) similar to cutting maneuvers showed significant differences between CAI and control groups; however, all participants in both groups had increased functional performance test times that indicated fatigue had negetive effect on ankle performance which could lead to exposure to recurrent sprain and instability. These results match other researchers’ results that have found weakness and changes in muscle activation in the hip in subjects with ankle instability (3-5). This finding points out the importance of assessing beyond the site of injury through sensorimotor chains. Gribble and hertel reported that, in fact, a destabilizing effect of a abductor muscular fatigue induced on the frontal movers of the dominant leg’s hip in mediolateral center of pressure (Cop) displacements in the unilateral dominant leg (16). On the other hand, Webster reported that when landing from a jump, if the center of pressure (COP) at the foot is located medial to the subtalar-joint axis when the foot makes contact with the ground, the vertical ground reaction forces, acting in the opposite direction, cause a greater supination movement which may lead to an inversion ankle sprain (5, 17). In addition, the results of Lee et al (2014) showed that individuals with diminished hip abductor muscle strength demonstrated decreased medial-lateral postural stability (18) also our results showed that two tests that had side hopping were significant between groups. Therefore hip abductor fatigue could affect medial-lateral postural stability, and predispose CAI group to recurrent ankle sprain and instability.
Another result of this study showed that Y balance tests scores for all participants in two groups were decreased in pretests to post tests, but there were differences in Y balance scores of CAI and control groups in pretest that refer to deficit in proprioception of CAI group (19-22). these results match theHoch and et al. results that reported postural control deficits had been observed in those with CAI when evaluated using dynamic assessment techniques examine by SEBT (20), Decreased scores of two tests of functional performance tests and static and dynamic balance tests indicated that gluteal muscles have a very important role in lower extremity injuries such as ankle injuries especially acute or chronic sprains, so we recommend to all specialists, physiotherapists and coaches to pay attention to the entire kinetic chain (resistance to hip muscles fatigue exercise) for recurrent sprain prevention and rehabilitation after occurrence ankle sprain.
Based on our results and other studies, we can say that gluteal muscles paly an important role in increased frontal-plane motion of the knee when landing, increased knee valgus and tibia external rotation that have been identified as potential mechanisms of lower extremity dysfunction. Gluteal muscles fatigue or weakness can result in valgus of knees and change the mechanics of lower extremity. On the other hand, hip muscles fatigue protocols result in altered force production, proprioception, coordination, and landing kinematics that can effect thelower extremity such as ankle, and put it to expose of sprains (23). Some studies reported that most injuries occur in the second half of the games, (1) this might be due to fatigue, so we recommend all specialists, coaches and athletes to incorporate resistance training into their programs to prevent of changes in kinetic chain and sprains following hip muscles fatigue.