1. Introduction
Several studies showed that ankle injuries occur in sports up to 30%. Residual symptoms may occur in up to 50% of people. In this regard, ankle impingement is a major cause of chronic pain. Anterior and posterior impingements are well documented and generally considered as separate entities with different causal injury patterns (1).
Complications are well described. The ankle arthroscopy complication rates from 7.6% to 13.6%, according to different authors (2, 3). Neurological injury is the most frequently described within the spectrum of complications including vascular injuries and false aneurysms, infections and synovial fistula, invasive distraction related problems and stress fractures. Furthermore, instrument breakage, complex regional pain syndrome (CRPS), compartment syndrome, thromboembolic complications (4), and painful scars are reported (5).
Deep vein thrombosis (DVT) is considered as a serious complication, especially in lower extremities and has the potential to result in significant morbidity and possible mortality (6, 7). The risk of DVT for patients with isolated foot and ankle conditions, even with plaster cast immobilization, and the possible benefits of mechanical and chemical prophylaxis were poorly studied (8). Nevertheless, some studies mentioned risk factors as injury severity (9), immobilization (10), obesity (11), nonweight-bearing (12), hindfoot surgery (13), and tourniquet time (13).
The current report aimed at showing an infrequent complication (DVT) in combined ankle arthroscopy for anterior and posterior ankle impingement syndrome.
2. Case Presentation
Informed consent was obtained from the study participant. A 27-year-old male patient, smoker, and recreational athlete referred to the outpatient orthopedics department complaining of left recurrent painful ankle. The patient had no specific risk factors for DVT preoperatively (family history, obesity, previous DVT, medical co-morbidities, or drugs, etc.). Hypercoagulable states were factor V leiden + and lupus anticoagulant -, as well as protein C or S deficiency, based on the evaluation of blood parameters. He previously had an ankle sprain while playing soccer. In the physical examination presented anterior (predominantly located anteromedially) and posterior ankle pain (positive ankle hyperflexion plantar test). The preoperatively AOFAS (the American orthopedic foot and ankle society score) (14) was 70. Radiological analysis showed an anterior ankle impingement type B (15) and a posterior impingement syndrome (posterior talar spur) (Figure 1).
Magnetic resonance imaging (MRI) showed an ankle synovitis and a flexor hallucis longus tenosynovitis (Figure 2).
He had conservative treatment (non-steroidal anti-inflammatory drugs, rehabilitation, and cryotherapy) for 3 months. Due to the lack of response, surgery was performed.
2.1. Surgical Technique
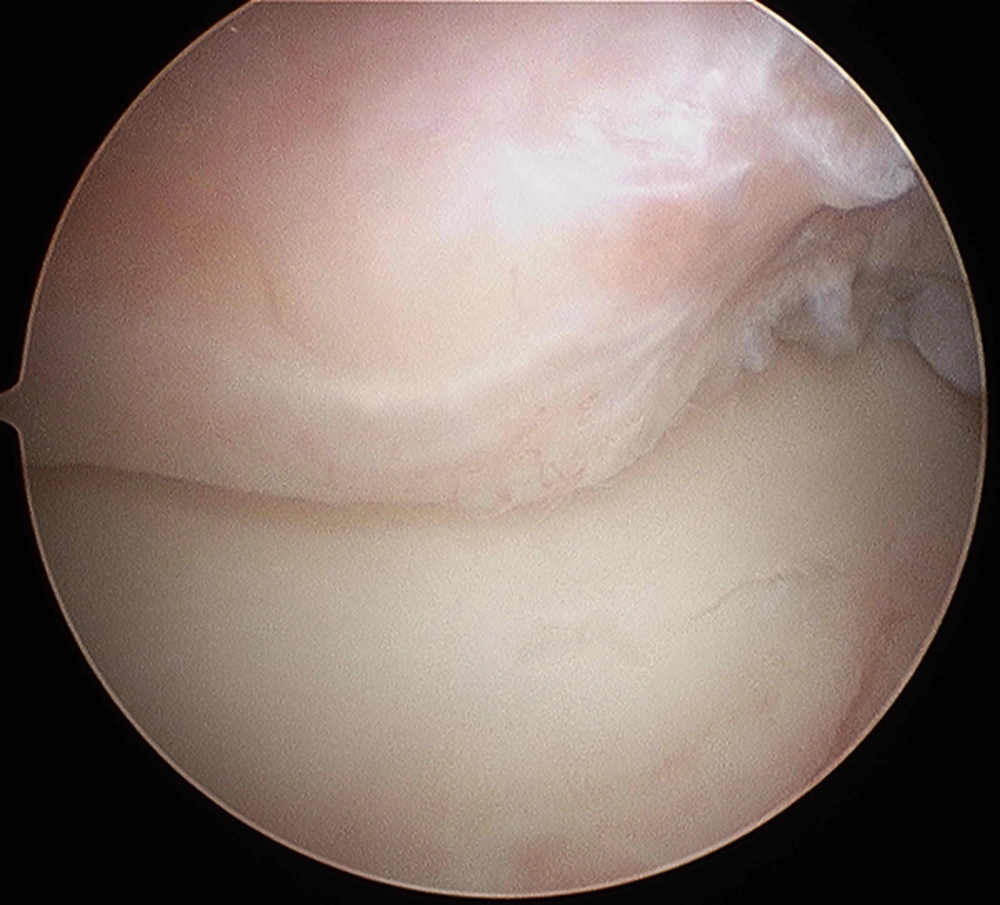
The patient received lumbar spinal anesthesia and placed in the supine position with a thigh tourniquet without any distraction technique. First, an anterior ankle arthroscopy was performed through the 2 standard anteromedial and anterolateral portals (5) to perform the debridement of osteophytes (Figure 3) and hypertrophic synovial in the anterior ankle (4.0 mm; 30 degrees; Storz). The duration of surgery was 25 minutes. Then, the patient was placed in prone position and a hindfoot endoscopy (16, 17) was performed to resect the talar spur (Figures 4 and 5) and tenosynovectomy; the duration was 22 minutes. The whole procedure lasted 65 minutes (including the patient’s change of decubitus). The tourniquet was deflated between the 2 procedures.
After the surgical procedure, the patient was not immobilized and authorized to full weightbear according to pain control with elastic bandage. According to the Caprini DVT risk factor assessment score (score 1: minor surgery planned) (8, 18), it was decided not to use pharmacological DVT prophylaxis.
2.2. Outcome
At 72 hours postoperatively, the patient had pain in posterior region of left leg, without other clinical sign of DVT; then, Eco Doppler was performed and reported DVT in deep posterior tibial vein. The patient was admitted for 24 hours to be matched for anticoagulation protocols (low molecular weight heparin 60 mg/24 hours), and then, discharged with rivaroxaban (19) 15 mg/12 hours for 30 days, reducing the dose to 20 mg/24 hours until 60 days of treatment. Four weeks after surgery, he began the rehabilitation without symptoms. At the 12 months postoperative visit, the patient was satisfied with the results and was performing sports activity (AOFAS score: 91).
3. Discussion
VTE (venous thromboembolism) is highlighted as a particular risk following the orthopedic surgery or injury to the lower limb. However, most studies investigating VTE were conducted on patients undergoing major orthopedic surgeries at or above the knee (4, 20).
The risk of VTE in patients with isolated foot and ankle conditions, even with plaster cast immobilization, and the possible benefits of mechanical and chemical prophylaxis were poorly studied (8).
The Caprini risk assessment model (RAM) was derived over a decade ago based on a combination of clinical experience and published data for risk-stratified plastic and reconstructive surgery patients for VTE risk (21). The Caprini RAM was 1st reported in 1980, and then, it was regularly updated to a relatively mature model in 2010 (18) (eg, supplementary file Appendix 1 shows the Caprini assessment and supplementary file Appendix 2 the suggested prophylaxis). Calder et al., published on VTE following the isolated foot and ankle surgery and proposed guidelines for VTE prevention (14). The most recent review by the American college of chest physicians (ACCP) also recommended against chemical prophylaxis in lower leg injuries requiring immobilization (22).
In the current report, the patient was authorized to walk with full weight bearing with elastic bandage, and had a low-risk of thrombosis according to the Caprini protocol; therefore, no anticoagulants were indicated.
Although the presented surgical technique had the disadvantage of repositioning the patient (from supine to prone), some studies mentioned that ankle arthroscopy and hindfoot endoscopy can be performed without adding endovascular complications (23). In the current study, the median total operative time, including the time needed for switching the position from supine to prone, was 94 minutes (ranged 72 to 168 minutes) and the result included 3 bilateral cases. However, the authors did not experience complications caused by changing the patient’s position. Nevertheless, the results of the current study suggested that simultaneous arthroscopic and endoscopic surgery can enable professional athletes with an intractable combination of AAIS (anterior ankle impingement syndrome) and PAIS (posterior ankle impingement syndrome) to return to athletic activity as soon as possible (23). Authors agree with the disadvantage proposed by Miyamoto et al., in relation to repositioning the patient, but it is thought that combined anterior and posterior ankle arthroscopy has other disadvantages such as longer surgical time with the aggravation of the use of tourniquet associated (13).
Vascular changes due to tourniquet may also include direct vascular injury, hyperemia on tourniquet deflation, and increased incidence of deep venous thrombosis, pulmonary embolism, and cardiac arrest (24, 25). Solis and Saxby found a direct relationship between the DVT and the duration of the tourniquet use. However, there are still no data regarding the removal and replacement of the tourniquet during the same procedure (13).
Anterior and posterior impingement can be treated arthroscopically or by open debridement with good results (1), but the arthroscopic technique is related to minor complications. Recently, Song et al. (26) presented a new technique to treat anterior and posterior impingements in dorsal decubitus by means of 3 portals. This, by avoiding turning the patient, might prevent complications avoiding long surgeries.
In conclusion, it seems that the use of prolonged tourniquet in addition to repositioning the patient may increase the risk of complications such as VTE and this combination is not included in any published protocol. Finally, authors also recommend the combination of the Calder antithrombotic recommendations (8) associated with the Caprini RAM (21), aimed at encompassing a higher risk population.