1. Background
The shoulder is the most commonly dislocated joint due to its large range of motion and weak bony support. It is estimated that this joint accounts for 50% of all major joint dislocations (1). The most common complication after a shoulder dislocation is recurrent dislocations (2). Bankart lesion, defined as labrum detachment from the glenoid rim, is the most significant pathological basis for the recurrent dislocations (3, 4). Bony defects in humeral head (Hill-Sachs lesion) and glenoid labrum, are the other two known causes of recurrent dislocation (1, 2). Up to 76% of recurrent shoulder dislocations show presence of Hill-Sachs lesions (5-7).
In 1950, Latarjet et al. proposed a successful technique to repair a glenoid rim defect using the coracoid process as a structural bone graft (8). The Latarjet technique used to be employed in patients suffering from recurrent shoulder dislocation particularly in glenoid bone defects (8). The technique has been modified since the conception by extracapsular placing of the graft through the middle part of the subscapularis tendon rather than detaching the superior one-third of the subscapularis muscle (9). In this study, we evaluated the mid-term results of minimally invasive modified Latarjet technique in traumatic anterior recurrent dislocations associated with gross Hill-Sachs and Bankart lesions.
2. Objectives
To evaluate the clinical results of minimally invasive modified Latarjet technique in recurrent, traumatic anterior shoulder instability associated with obvious Hill-Sachs and Bankart lesions.
3. Patients and Methods
For this prospective observational study, we enrolled all 36 patients with recurrent traumatic anterior shoulder instability who underwent minimally invasive modified Latarjet procedure in Ghaem Hospital, Mashhad, Iran between 2007 and 2013. All participants were consenting adults with a history of at least two previous anterior dislocations of the same shoulder and glenoid defect of more than 30% in CT scan. The exclusion criteria included a previous surgical stabilization of the shoulder. The osseous defects and Bankart lesion were evaluated pre-operatively using plain radiographs, CT scan and MR imaging. The MRI studies revealed labrum detachment and Hill-Sachs lesion in all shoulders. Informed consent was obtained from all participating patients and the Ethical Research Committee of Mashhad Medical University approved the study.
For all patients, demographic and injury data were obtained and Constant Shoulder score, Rowe score, and UCLA scores were completed by the operating surgeon. The shoulder stability was assessed with the Jobe’s relocation test preoperation. The patients were followed up at two weeks, one month, three months, and six months from the date of the surgery and evaluated for probable complications. Above mentioned assessments were completed again at the time of the final follow-up by the same surgeon.
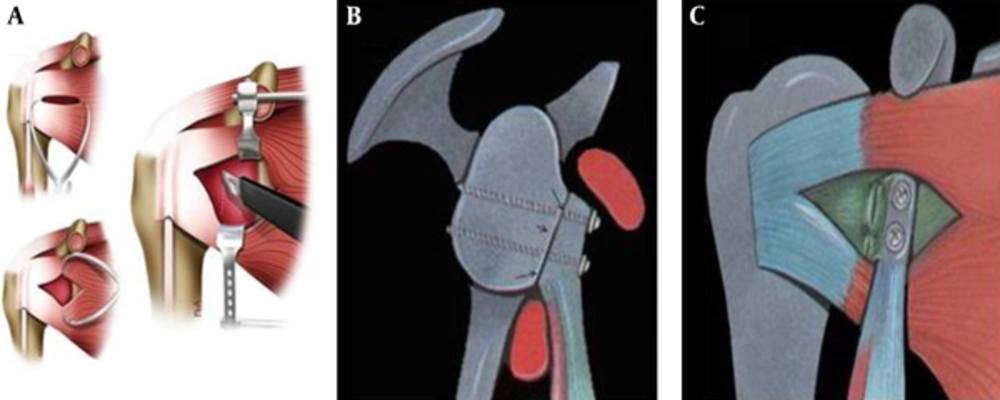
The modified Latarjet technique was used in our study. In the original Latarjet technique, all the long part of coracoid process was detached from scapula. After that, the pectoralis minor tendon and coracoacromial ligament were detached and the bone was used as a bony block in the anterior inferior glenoid region between superior one-third two-third of the subscapularis muscle (8). In the modified technique, we split the muscle along the middle portion of muscle fibers instead of detaching the superior one-third of subscapularis muscle (Figure 1) (9).
The average age of the enrolled patients was 24.6 ± 3.3 (ranging from 18 to 33 years) (Table 1) and 35 patients out of the total of 36 patients were males. Motor-vehicle accidents were the major cause of the injuries (52%, Table 2) with the average interval between the injury and operation of 3.1 ± 1.2 years (Ranging from 1 to 5 years). The average number of incidents of dislocations between the injury date and the surgery was 7.2 ± 2.1 (Ranging from 4 to 20). The average follow-up period was 37 months (ranging from 12 to 65 months).
SPSS version 16 (SPSS Inc, Chicago, IL) was utilized for statistical analysis. The data was presented using mean and standard deviation in continuous variables and frequency and percentage for string variables. Paired t-test was administered for comparing the means of different scores before and after the operation. ANOVA test was used to analyze categorical variables and P value of 0.05 was considered significant.
| Variable | Frequency | Percent | P Value |
|---|---|---|---|
| Gender | < 0.001 | ||
| Male | 35 | 97.2 | |
| Female | 1 | 2.8 | |
| Etiology | 0.091 | ||
| Motor-Vehicle Accident | 19 | 52.8 | |
| Fall from height | 10 | 27.8 | |
| Fall in sport | 4 | 11.1 | |
| Others | 3 | 8.3 | |
| Affected side | 0.23 | ||
| Right | 23 | 63.9 | |
| Left | 13 | 36.1 | |
| Dominant side | |||
| Right | 25 | 69.4 | 0.11 |
| Left | 11 | 30.6 |
| Results a | Before Operation | After Operation | ||
|---|---|---|---|---|
| Frequency | Percent | Frequency | Percent | |
| Excellent | 0 | 0 | 34 | 94.4 |
| Good | 1 | 2.8 | 2 | 5.6 |
| Fair | 14 | 38.8 | 0 | 0 |
| Poor | 21 | 58.4 | 0 | 0 |
aExcellent = 100 to 90; Good = 89 to 75; Fair = 74 to 51; Poor ≤ 51.
4. Results
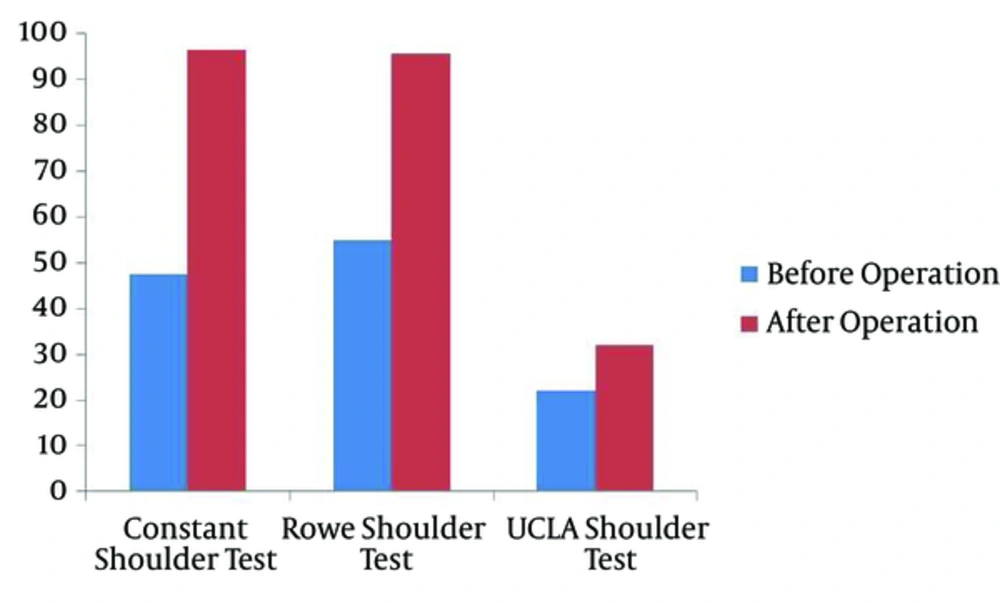
All patients had positive Jobe’s relocation test (Aprehension sign) pre-operatively and negative Jobe’s relocation test post-operation. Significant improvements in scores were demonstrated after the surgery compared to pre-operational assessment in all cases (P value < 0.001 in all tests) (Table 2-5Figure 2). Final follow up radiographs showed union of all the grafts and patients reported no incidents of re-dislocation during the follow-up period (Figure 3). One incidence of a superficial infection two weeks post operation was the only complication in this study. The infection was resolved with antibiotic treatment.
| Results a | Before Operation | After Operation | ||
|---|---|---|---|---|
| Frequency | Percent | Frequency | Percent | |
| Excellent | 0 | 0 | 34 | 94.4 |
| Good | 0 | 0 | 2 | 5.6 |
| Fair | 7 | 19.4 | 0 | 0 |
| Poor | 29 | 80.6 | 0 | 0 |
aExcellent = 100 to 90; Good = 89 to 75; Fair = 74 to 51; Poor ≤ 51.
| Results a | Before Operation | After Operation | ||
|---|---|---|---|---|
| Frequency | Percent | Frequency | Percent | |
| Excellent | 0 | 0 | 14 | 38.9 |
| Moderate | 0 | 0 | 22 | 61.1 |
| Poor | 36 | 100 | 0 | 0 |
aExcellent = 100 to 90; Good = 89 to 75; Fair = 74 to 51; Poor ≤ 51.
A) Bony Bankart lesion and a Hill Sachs lesion on humeral head; B) Post-Operative X-ray; C) Follow-up CT scan shows solid union of the coracoid graft; D) Normal external and internal rotation ranges of motion of the shoulder one year after surgery compared to unaffected side; E) Internal rotation range of motion of the shoulder one year after surgery
5. Discussion
In this study, most of the patients were males in their twenties who sustained the injuries in motor vehicle accidents. The Latarjet procedure demonstrated good or excellent short-term outcomes in management of the patients with traumatic, recurrent anterior shoulder dislocation with a low level of post-operative complication risks.
There are several key points of comparison between this study and the previous studies. While the sample size of this study is within the range of the other studies, ranging for 11 to 113 patients, (3, 9-12), our follow-up period was close to most published studies (3, 9-12). The average age, 24 years old, is also younger than the population of participants in most studies (3, 9, 10, 13-16). The mean age in other studies varied between 26 to 58 years. In our study, almost all of the patients were males in contrast to the gender distribution of the other studies that ranged between 68 and 90 percent (3, 10, 17).
Another mismatch between our population and other studies was the cause of recurrent dislocation. In more than half of our patients the major cause of the primary shoulder dislocations was motor-vehicle accidents while sports injuries were accounted for 11%. In the study by Cerciello et al. sport injuries were responsible for more than 80% of primary shoulder dislocations and motor-vehicle accidents were only accounted for 4% of patients (18). The discrepancy may be due to the high rate of motor-vehicle accidents in Iran.
In the current study, the time between initial shoulder dislocation due to trauma and surgical intervention was 3 years with on average 7 incidences of dislocations. Doursounian et al. reported the interval of 5 years (17). Lafosse et al. and Hart et al. reported the average of 6 and 5 dislocations before operation (12, 16).
Similar to our study, the Jobe’s relocation test of pre-operative patients in previous literature was usually positive in all patients with recurrent dislocation (3, 9, 10, 16). This test was found positive in 2 to 33 percent of patients after operation (3, 9, 10, 16, 19),which is in contrast to our study which showed negative Jobe’s relocation test in all shoulders after the operation.
Patients with recurrent shoulder dislocations experience high level of disability before surgical stabilization (10, 12). Hart et al. reported the score of 56 according to Constant questionnaire and Allain et al. reported the score of 51 according to Rowe score before operation indicating similar levels of disability as demonstrated in this study (10, 12). The dramatic improvement of the shoulder function after the operation mirrored the results seen in the other studies. After operation, Constant score was reported as high as 84 to 95% (9, 10, 14, 16) and Rowe score 90 to 93% (10, 14). In our study, Constant and Rowe scores after operation were 96 and 94 respectively.
Latarjet procedure has known possible complications such as persistent instability (10, 20), fibrous nonunion (9), screw fractures (9), and osteoarthritis (19, 20). In our series we had only one superficial infection. However, the lower rate of complication may be due to the mid-term follow-up.
The key limitations of this study are the short follow-up period, restriction of the patients on one center, and the lack of control groups. The follow-up period was limited to 37 months, which is not long enough to reveal long-term complications such as osteoarthritis and screw breakage. Additionally, we were unable to assess the efficacy of the modified Latarjet technique compared to the other common techniques such as standard Latarjet, Bankart, or Bristow as control groups. Moreover, given the lack of control group, we could not prove that the good results of study were related to the surgery itself or they are the natural healing process or the rehabilitation program after operation. In conclusion, our study demonstrated the minimally invasive Latarjet technique is an effective management approach to recurrent traumatic anterior shoulder dislocations with good or excellent short-term outcomes with a minor complication risk.