1. Background
Globally, the number of elderly individuals is growing faster than all of the younger age groups. The elderly population -those aged 60 years or older- is expected to more than double by 2050 and more than triple by 2100, from 962 million worldwide in 2017 to 2.1 billion in 2050 and 3.1 billion in 2100 (1). In this scenario, the growth of the elderly population has become a public health concern because aging brings with it a series of physiological and anatomical changes that predispose people to chronic diseases and functional limitations (1-4). Therefore, possible repercussions, such as falls, can occur frequently in the elderly population. Falls are defined as episodes of imbalance that can cause the elderly to come into accidental contact with the ground or nearby surfaces (5, 6). Falls increase rates of morbidity, mortality and hospitalization and can cause injuries that are costly to treat (7, 8). Approximately 30% of falls result in severe injuries in the elderly, and there is a relationship between age and the frequency of episodes of postural imbalance (9). Since one in three elderly individuals suffer falls, it is necessary to develop interventions to promote the maintenance of postural balance in this population (10).
Balancing is an extremely complex process that involves the proper functioning of the vestibular, visual and central and peripheral nervous systems, as well as the responses of the musculoskeletal system to sensory stimuli. These responses are related to the integrity of range of motion, muscle strength and proprioception (11). As a biomechanical strategy for maintaining balance, the individual tries to maintain his or her center of gravity on his or her support base using all possible means of doing so (12-14).
Conventional balance exercises are one of the most preferred exercise options for improving balance in geriatric populations. As an alternative to conventional balance training, virtual reality rehabilitation (VRR) has increasingly been used. VRR is an emerging technology used for the physical restoration of different populations. It is defined as a two- or three -dimensional computerized simulation that gives users the illusion of interactively entering a virtual world in real time (15). During real-time use, it is believed that the central nervous system incorporates sensory augmentation as an additive input, supplementing other sensory information (16).
VRR can promote adaptation of the individual in the proposed training, which is followed by a progression of exercises through varied levels of difficulty offered by the platforms. This model is consistent with the recommendations made regarding exercises for the geriatric population (i.e., starting an activity according to the individuals’ capacities and gradually looking for an evolution of functionality) (17). Both randomized and nonrandomized controlled trials have reported positive effects of VRR activities on gait speed, functional balance, and cognition (18, 19). In addition, VRR-based balance exercises seem to improve strength, mobility, and functional abilities, while decreasing fears of falling, in community-dwelling older adults (16-19).
Currently, electronic platforms, such as the Nintendo™ Wii Fit, are being used as tools for VRR in the field of physical therapy (20). VRR leveraging these platforms has shown satisfactory results in various clinical conditions, mainly due to the excellent adherence of individuals to treatment plans (21, 22). In addition, in recent years, sensors have been developed that capture movements of the user’s entire body and reproduce them faithfully on a screen. One example of this is the Kinect sensor (KS), which was developed by the Microsoft Corporation (20). These sensors allow the user to have the freedom to move without the need for controllers and offer different types of games, with each emphasizing a certain type of motion.
The use of sensors that capture body motion may be an effective option to address the need for new resources to treat postural imbalance, especially since the proposed activities, in addition to being playful, stimulate movements similar to exercise therapies used in balance rehabilitation. Despite being more accurate and reliable compared to other platforms, the KS is still rarely used in VRR of postural balance in elderly subjects (23).
2. Objectives
To evaluate the effect of training using body sensors on body balance in the elderly.
3. Methods
3.1. Participants
Between October 2017 and May 2018, a non-randomized controlled clinical trial was conducted with 16 individuals aged ≥ 60 years. Individuals who reported previous heart disease, uncontrolled hypertension, visual and/or auditory disorders, neurological disorders and musculoskeletal problems were excluded (24, 25). Additionally, a Berg Balance Scale (BBS) score of less than 45 points was also used as exclusion criterion because these individuals have a high risk of falls during walking (26, 27). The project was approved by the Research Ethics Committee of the Faculty of Medical and Health Sciences of Juiz de Fora (SUPREMA), Juiz de Fora, Brazil, under number 0015/12 and is in compliance with the provisions of the Declaration of Helsinki. All of the individuals who participated signed consent forms.
We also evaluated a control group that consisted of 10 young adults with a median age of 23 (20.1 - 27.8) years, of whom five were men. The median body weight of this group was 65.6 (59.8 - 70.1) kg. This group was subjected to the same exclusion criteria as the group of elderly subjects.
3.2. Intervention
The treatment protocol consisted of 10 sessions lasting 20 minutes each. During this time, 14 minutes were allocated to the application of stretching exercises, and the remainder was used for rehabilitation with the KS (Microsoft Corporation, Redmond, WA, USA). The period between the evaluations was five weeks, and the sessions were performed three times per week. Before the first session and one day after the last session, participants underwent static and dynamic balance assessments; a resting state was used for these assessments. In this and the other sessions, the participants performed muscle stretching exercises, which were followed by the activity with the KS.
3.3. Berg Balance Scale
The BBS is widely used in clinical practice, especially among the elderly and people with neurological disorders in rehabilitation programs. It consists of 14 common static and dynamic balance tasks based on activities of daily living such as standing up, transferring, standing unsupported, reaching and turning. Each task yields a score between zero and four points. If the participant required supervision or an external aid to perform the task, a lower score was assigned for the corresponding task. The evaluation was based on the sum of the tasks’ points, with a potential maximum score of 56 (26, 27). After the BBS was finished, the participants completed a sequence of specific tests of static and dynamic balance, which also served as a parameter for comparing gains in postural balance (28).
3.4. Timed Up and Go test
The Timed Up and Go (TUG) test is performed by having the individual rise from a chair with a backrest, walk three meters and return to the chair. The speed of the execution of the task is established by the participant, as there is no stimulus through verbal commands. For this study, the time taken by the participant to complete this task was measured at the initial evaluation and after the 10 sessions were completed (29, 30).
3.5. Tandem Romberg Test
The participants held themselves in a standing position with their eyes closed and the calcaneus of their non-dominant foot in front of the toes of their dominant foot until they lost their balance or reached the maximum time of one minute (31, 32).
3.6. Muscle Stretching
After blood pressure measurements were obtained, participants performed muscle stretching exercises to increase their performance during the KS sessions because the flexibility triggered by these exercises is an important tool for adequate postural balance (13, 33). The muscle stretches were performed bilaterally and in an active-assisted manner. The stretches included lateral cervical flexion, forward and backward cervical inclination, standing trunk flexion, lateral trunk inclination and rotations in the transverse plane. For the upper limbs, shoulder and elbow flexion, horizontal adduction of the shoulder joint and flexion and extension of the fingers and wrists were performed.
3.7. Kinect Sensor
The Stack ’Em Up mode (difficult level) in the Your Shape™ Fitness Evolved game, which is available on the Xbox 360 platform, was used. The participants were instructed in how to complete the activity and were aided by verbal commands. They positioned themselves in front of the KS and remained in a static position, with their upper limbs raised, simulating holding a board. In the game, colored blocks are dropped onto this board, which must be dropped into an opening on the floor by inclining the trunk laterally, based on the visual stimulus received, to the same side as the opening on the floor, which is simulated on the bottom half of the screen. The floor opens alternately on the right and left sides. Occasionally, burning blocks are dropped, and to put them out, it is necessary to raise the lower limb on the same side as the block that is descending toward the board through hip and knee flexion of 90°.
3.8. Statistical Analysis
The distribution of the data was analyzed using the Shapiro-Wilk test along with graphical analysis of the histograms. Because the variables presented as non-Gaussian distributions in at least one of the study moments (before and after intervention with the KS) and/or groups (elderly and younger adults), non-parametric tests were used. Inferential analysis consisted of the Wilcoxon signed-rank test to compare the assessments before and after intervention with the KS within each group (intragroup analysis) and the Mann-Whitney test to compare the results of the elderly with the results of the young adults (intergroup analysis). The values of relative delta between the two moments of the study (before and after intervention with the KS) were calculated as follows: Equation 1. Variables were described in terms of median and interquartile interval values. Differences were considered statistically significant at P < 0.05, with 95% confidence intervals. Analyses were conducted using SAS 6.11 software (SAS Institute, Inc., Cary, NC, USA).
4. Results
Of the 16 elderly individuals who were evaluated for inclusion in the study, six were excluded for the following reasons: Visual and/or auditory disorders (n = 2), musculoskeletal problems (n = 2) and BBS scores of less than 45 points (n = 2). The median age of the elderly subjects was 64.5 (60.8 - 68.7) years, and five of them were men. The median body weight of this group was 61.7 (56.4 - 66.5) kg, which was not significantly different from that of the control group (P = 0.13).
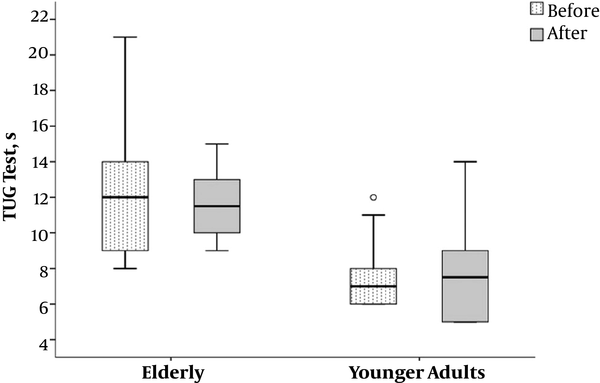
The results of the body balance tests for the elderly and young adults are shown in Table 1. Relative to the young adults, the elderly required a longer median time to perform the TUG test both before and after KS training (P = 0.003 and P = 0.015, respectively). However, there were no significant differences in the TUG test (relative deltas) within either group between the pre- and post-intervention analyses (Figure 1).
| Variables | Elderly | Younger Adults | P Valuec |
|---|---|---|---|
| TUG test, s | |||
| Before using KS, s | 12 (8.8 - 14.5) | 7 (6 - 8.8) | 0.003c,d |
| After using KS, s | 11.5 (9.8 - 13) | 7.5 (5 - 10) | 0.015c,d |
| Relative delta, % | -7.7 (-13.8 - 29.9) | 7.2 (-35.1 - 40.6) | 0.88 |
| P valueb | 0.96 | 0.81 | |
| Tandem Romberg, s | |||
| Before using KS, s | 9.5 (4.8 - 60) | 60 (60 - 60) | 0.012c,d |
| After using KS, s | 56 (17.8 - 60) | 60 (60 - 60) | 0.045c,d |
| Relative delta, % | 275 (0 - 950) | 0 (0 - 0) | 0.11 |
| P valueb | 0.075 | 0.31 | |
| BBS, points | |||
| Before using KS, points | 52 (49.8 - 53.3) | 56 (56 - 56) | 0.0001c,d |
| After using KS, points | 54.5 (54 - 55.3) | 56 (56 - 56) | 0.0006c,d |
| Relative delta, % | 4.8 (3.3 - 8.1) | 0 (0 - 0) | 0.0001c,d |
| P valueb | 0.005b, c | 0.31 |
Results of Body Balance Testsa
In the tandem Romberg test, the two groups showed different values both before and after the KS intervention (P = 0.012 and P = 0.045, respectively). However, there were no significant differences within either group when the differences between the pre- and post-treatment values (relative deltas) were assessed (Figure 2).
When evaluated using the BBS scale, there were significant differences between the elderly and young adults both in the initial evaluation (P = 0.0001) and in the final evaluation (P = 0.0006). When the relative deltas between the pre- and post-treatment BBS scale values were evaluated, a significant difference was only observed in the elderly group (P = 0.005) (Figure 3).
5. Discussion
The main findings of the present study were the significant improvements in static and dynamic balance in the elderly subjects after a rehabilitation program with the KS based on evaluations using the BBS. In addition, the elderly showed an improvement in static balance as measured by the tandem Romberg test, although this improvement only showed a trend toward statistical significance. To our knowledge, this is the first study to show an improvement in postural balance in the elderly after a rehabilitation program using the KS.
In conventional rehabilitation programs, it is very difficult for health professionals to teach patients to optimize their postural balance. In addition, the exercises usually become repetitive and adherence to the interventions gradually decreases, especially in the elderly population. VRR, in this context, can promote the completion of challenging exercises using technological resources that provide auditory, visual and proprioceptive feedback, thereby integrating the systems involved in postural control in a playful way, which consequently results in greater motivation to continue treatment (34). One of the benefits of VRR is the ability of the trainer to vary environmental conditions and give feedback; greater learning is demonstrated with training in virtual rather than physical environments (35). Upon undergoing VRR, the geriatric population exhibits improvements in postural balance even though these vary across types of platforms with regard to intensity, duration, repetitions, and series (36).
In the present study, after VRR using the KS, the elderly subjects did not present with a significant reduction in the time spent performing the tasks in the TUG test. These results are in contrast to those observed by Hara and Shimada (37) who used the TUG test to evaluate the dynamic postural balance of elderly subjects after an exercise program performed two to three times per week. The authors observed a reduction in the test execution times after the intervention. Interestingly, Kimura et al. (38) suggested, based on the execution time of the TUG test by the elderly subjects in their study, that age is directly proportional to the time required to complete the test.
Despite disagreements in the literature regarding the determination of a cutoff point in the TUG test to predict the minimum time suggestive of a fall risk, this is one of the tests most commonly used in clinical practice (39). Shumway-Cook et al. (39) proposed that a time greater than 13.5 seconds represents a high risk of falls, while Okumiya et al. (40) established a higher cut-off point of approximately 16 seconds. In the present study, although we did not observe significant differences between the pre- and post-intervention analyses, the reduction of the median from 12 seconds to 11.5 seconds in the test execution time in the elderly may have some clinical importance because there was an increase in the distance between the TUG test results and the cut-off points previously described.
Regarding the static balance assessment, Longridge and Mallinson (41) used the tandem Romberg test and did not find significant differences between young and elderly adults in relation to performance on the test, suggesting that this test is not effective at predicting balance conditions since it is not sufficiently precise in distinguishing individuals from different age groups. Contrary to these findings, we observed a significant difference between the two groups in the tandem Romberg test, with an obvious distinction in the time maintaining balance at the initial evaluation. Importantly, our study showed a trend towards statistical significance in the Romberg tandem test in the elderly after treatment with KS. This outcome is explained by the fact that the Stack ’Em Up mode in the Your Shape™ Fitness Evolved game intermittently demands lateral trunk flexion and one-leg stance movements, which stimulates straightening and trunk balance reactions. These reactions are also required during the tandem Romberg test, as the body’s weight is predominantly supported by ankle inversion and eversion movements when the patient positions one leg anteriorly and in the same line as the other (42). Although it only evaluates static balance and its execution is substantially influenced by the learning effect, the tandem Romberg test is a simple, low-cost test that does not take up too much time during physical examinations and balance control assessments (31).
According to Whitney et al. (43) the BBS is one of the most relevant tests for predicting the risk of falls. This instrument is considered safe and easy to apply in the elderly population because it only requires verbal guidance and its equipment costs and supervision requirements during the performance of the tasks are low (26). Park and Lee (44) established through a meta-analysis that cut-off scores between 45 and 49 points had lower heterogeneity for the interpretation of the risk of falls and that the accuracy of the BBS scale was 0.84 based on the groups studied. The VRR intervention using the KS proposed in the present study yielded a gain of 2.5 points in the median score when comparing the pre- and post-intervention analyses (52 vs. 54.5 points). The control of postural balance in the elderly as measured using the BBS in the present study was far from the cut-off points observed in the meta-analysis by Park and Lee (44), including in the studies that considered values of up to 49 points as predictors of a high risk of falls; however, it is worth noting that we used a BBS score of below 45 points as an exclusion criterion in the present study. In agreement with our findings, Yesilyaprak et al. (45) observed that BBS scores improved significantly, with a 3.4-point mean change, following VRR in older adults. These authors used VRR exercise sessions through balance training with visual displays and audio feedback.
Using a meta-analysis, Lesinski et al. (46) suggested that the duration of a single training session of 31 - 45 minutes is critical for positive outcomes in the static and dynamic balance of elderly patients. These authors also suggested a frequency of three times per week as being most adequate for achieving therapeutic success. Although our study also used a frequency of weekly sessions similar to that suggested by Lesinski et al. (46), the duration of each session with the KS was five to seven times shorter than that recommended in the rehabilitation of balance using conventional methods (46). This reinforces the importance of playful and motivational training in the geriatric population through VRR.
Hernandez et al. (47) subjected elderly individuals with Alzheimer’s dementia to a systematized regimen of physical activity that included dance, stretching and relaxation exercises; each activity session was 60 minutes long, sessions were held three times per week, and the intervention was held over a six-month period. The researchers evaluated balance using the BBS and the TUG test, and they did not observe significant differences between the pre- and post-intervention evaluations in the experimental group. The intervention in our study, on the other hand, showed a significant increase in the BBS score even with a total intervention time 10 times lower than that of Hernandez et al. (47). In addition, there was a significant difference in relation to the lengths of these interventions. It should be noted, however, that Alzheimer’s disease presents with neurological deficits that lead to apraxia, hypertonia and postural changes in the medium and long term, and this disease was not reported in the evaluation of any of the volunteers in the present study.
Another aspect worth mentioning is the inversely proportional relationship between age and the BBS score. In a comparative study by Pereira et al. (48), the authors suggest that the BBS is able to discriminate the risk of falls depending on the age of the individuals. This fact was also observed in our study and, additionally, an increase in the sum of the points after the intervention was observed, thus showing a reduction in the risk of falls in the elderly population after the KS intervention.
An additional advantage of VRR in the elderly is improvement in social and family interactions, which may be important in the context of the natural consequences of aging (49). It is worth mentioning that the motor learning achieved through this therapeutic method can be transferred to the activities of daily living, thereby promoting the reintegration of the elderly into the environment (45). These factors extend to institutionalized patients who, although often subjected to conventional methods of the rehabilitation of balance, experience limited stimulation because there is not much variation in the tasks proposed. This condition can be modified with the use of virtual platforms such as the KS (50).
Using the KS, Clark et al. (51) proposed that a three-dimensional system for the detection of body positions may be valid as a tool for the rehabilitation of postural balance in the clinical setting. This is confirmed in our study, as we found that the postural control of the elderly subjects improved. Llorenz et al. (52) used the KS as a resource for the rehabilitation of postural control in patients in the spastic phase of stroke recovery; they observed a significant difference between pre- and post-intervention results. One of the relevant aspects of the intervention proposed by the present study is the duration of the sessions, which at only six minutes is relatively short when compared to the previously described clinical trials (47, 51).
Other devices that can be used as short-term therapeutic modalities, such as the Wii, also demonstrated an increase in the BBS score. According to Bateni (53), the sessions performed with this device improved postural balance through a four-week protocol with an intervention period of four weeks, with three sessions performed each week. However, the KS allows greater freedom for the lower and upper limbs in relation to other platforms and thus is able to cover a greater number of body functions.
The relevance of our study is the playful approach for the elderly through a treatment protocol with short-duration sessions and the search for an integration of several systems involved in postural balance using a low-cost and widely available device. However, like any study, ours also has its limitations. First, the sample size is relatively small. Second, we did not evaluate the vestibular system before the intervention; the vestibular system provides major information on the maintenance of balance, and rehabilitation plans are often designed based on vestibular system disorder. Third, we did not use a more objective method to evaluate balance, such as a force platform. Finally, the participants did not undergo training to perform the sessions with the KS. Despite these limitations, the findings of the present study may serve as a starting point for future trials with subjects with one of the many clinical conditions known to alter postural control.
In conclusion, the treatment protocol involving the KS was able to promote an improvement in postural control in elderly subjects as evaluated using the BBS, and this improvement helped them reach levels close to those observed in younger adults. For the TUG test and tandem Romberg test, there was also improvement in the postural balance of the elderly subjects despite the absence of a significant difference between the pre- and post-intervention values. Thus, our findings suggest that VRR is an interesting resource that promotes positive effects on adherence to treatment and improves clinical outcomes. The use of VRR technology to design games focused on augmenting traditional rehabilitation interventions will likely play an important role in the future treatment of older adults with and without disabilities. Larger clinical studies are needed to establish the efficacy of VRR on the sensorimotor system using various clinical populations.