1. Background
The menisci play a crucial role in protecting biomechanical operations of the knee. It also provides joint lubrication and cartilage nutrition as well as proprioception (1).
Meniscal injuries result in knee joint instability and hence, it is a strong predictor of later knee osteoarthritis (OA) (1). One of the procedures done to treat the injured menisci is partial or total meniscal excision. Though well-established knowledge found that all meniscectomies knees eventually develop arthritic changes as a long term sequalae (2-4). The severity of these changes is proportional to the amount of meniscus removed. Structural, biochemical, and mechanical articular cartilage changes following partial meniscectomy are thought to be due to increased intra-articular contact stresses and loss of the load distribution that operates to prevent the menisci from extruding out of the joint throughout axial loading and decreased stability of the knee (2, 5, 6). It was proved that articular cartilage loss following partial meniscectomy (6.9% per year) is significantly higher compared to healthy controls (2.3% per year) (7).
Arthroscopic repair of torn menisci has thus become the mainstay treatment methodology if the repair is feasible (8). All repair techniques are the accepted arthroscopic repair techniques (9). Many factors are thought to have effects on the results of meniscal repair; such as tear location, size, and chronicity, repair technique; patient age, body mass index (BMI), level of activity and habits, as well as the presence of associated injuries. Favorable results are observed after treatment of longitudinal acute tears within the peripheral vascular zone of the meniscus and in young people with stable knees (10). However, meniscal repair doesn’t consider the underlying biological changes to the microenvironment that is attributable to OA. In addition, repair of avascular meniscal tears is associated with high failure rate because of the limited healing capacity in the inner two-thirds of the meniscus, leading to biomechanical alterations and articular cartilage degeneration (8). Thus, biological therapy as well as tissue engineering may be used alternatively or complementary to repair the avascular zone of the menisci (11).
Platelet-rich plasma (PRP) as an autologous biologic therapy is a promising strategy to help induce tissue healing. It is considered as plasma with concentrated platelets above normal values (3 - 8 times the concentration of normal platelet levels) (12). It contains growth factors, chemokines, interleukins and cytokines released from platelets to enhance the natural healing process and tissue regeneration within the treatment site (13). It also contains proteins and bioactive molecules that play a crucial role in the cellular repair cascade (14, 15). Because PRP contains growth factors and plasma proteins, it will regulate pro- and anti-inflammatory signals causing angiogenesis equilibrium (16, 17).
Although PRP has been employed in clinical practice for a few times, to date, few clinical researches support its use in meniscal lesions and in improving meniscal repair outcomes (18). One matter of importance is the paucity of prior published randomized controlled studies assessing the effect of PRP on meniscal healing.
2. Objectives
The aim of this work was to assess the impact of 6- monthly intra-articular injection of PRP in patients who had undergone unilateral arthroscopic isolated meniscal repair for complete meniscal tears located at the red-white zone of the meniscus, performed by a single surgeon and presented with knee pain within 4 months after surgery. Our hypothesis was that intra-articular PRP injection may add beneficial effect on post-meniscal repair outcomes regarding pain and functional state of the operated knee.
3. Methods
3.1. Subjects
The study was done on 30 patients undergoing arthroscopic isolated meniscal repairs by single surgeon and presenting with knee pain within 4 months after surgery. Approval from local Ethics Committee was obtained and institutional review board approval was granted. A written informed consent was taken from all participants.
Inclusion criteria were patients aged 18 - 55 years undergoing complete meniscal tear in red-white zone repaired by single surgeon and complaining of pain within 4 months after repair.
Exclusion criteria were some systemic disorders, such as diabetes, autoimmune diseases, hematological disorders, cardiovascular diseases, infections, local knee injuries other than meniscal injury as well as patients receiving treatment with anticoagulants-anti-aggregates or use of non-steroidal anti-inflammatory drugs (NSAIDs) within 5 days before blood being taken.
Random, double blinded selection of 15 patients to constitute the PRP-group was injected intra-articularly with about 5 mL of PRP in the operated knee joint, at 1-month intervals, for 6 injections. The other fifteen patients were not injected and constituted the control group.
3.2. Study Design
At the first visit all patients were subjected to (1) thorough general and meniscus repair related history taking focusing on articular cartilage status, zone, type, chronicity of tear, and type of repair (2). General examination and complete knee joint examination. The severity of pain was assessed by visual analogue scale (VAS) (19). The Knee injury and osteoarthritis outcome score (KOOS) questionnaire was applied to all studied patients in order to evaluate the function of the operated knee (20). Patients were instructed to complete the KOOS form by considering their operated knee at first visit, 3 and 6 months following PRP injection for the PRP group and two times (baseline and 6 months later) for the non-PRP group.
High resolution ultrasonographic examination was performed by a single radiologist who was blinded for the studied subject by using Siemens Prima apparatus, utilizing high resolution multi-frequency probe (3.5 - 7 MHz). Using transverse suprapatellar scans tangential to the upper patellar pole at 90° knee flexion to assess for tibio-femoral cartilage thickness, regularity of the cartilage margins and knee effusion (21). Ultrasonography reports included comment on increased vascularity (Doppler activity), and synovial hypertrophy. The cartilage thickness was measured within the weight-bearing area from four anatomical locations; namely, the medial femoral condyle (MFC), the lateral femoral condyle (LFC), the medial tibial condyle (MTC), and the lateral tibial condyle (LTC). Measurements were done two times at the first visit (baseline) and after six months for the operated knees for both groups.
The PRP-group (15 patients) were injected at one-month intervals, for 6 injections. Pre-injection guidelines were given to all patients in the form of stopping steroidal and non-steroidal anti-inflammatory drugs for at least one week before the procedure, as well as stopping any anticoagulant drugs 5 days before the procedure, increasing intake of fluids within the 24 hours prior to the procedure and anti-anxiety medication were required for anxious patients. Injection, under complete aseptic technique, was performed while the patient was in supine position, and the knee was fully extended, using the lateral approach. Patients were instructed after injection to avoid using the injected leg for 24 hours, to use ice packs over the injected joint and not to use NSAIDs for another one week (22).
3.3. Platelet-Rich Plasma Preparation
Thirty milliliters of venous blood was taken from every patient and collected in sodium citrated sterile tubes. Platelet concentrates were obtained by adjusting centrifuge at 1800 rpm for 15 minutes to separate erythrocytes, then at 3500 rpm for 10 minutes to concentrate the platelets (23). Thus 5 mL of PRP was obtained, 0.2 mL of 10% calcium chloride was added to the final product to activate the platelets and injected immediately without storage. It is believed that freshly-harvested PRP would possibly preserve the platelet functions better (22).
Follow up was done following six PRP monthly injections; all patients were re-evaluated again by VAS, KOOS score as well as by musculoskeletal high-resolution ultrasonography. After 3 PRP injections, both groups were re-evaluated by VAS and KOOS only.
3.4. Statistical Analysis
Data of the patients were entered on the applied math package for Science (SPSS version 17, Chicago, IL, USA). Quantitative data were demonstrated as mean and standard deviation, whereas the qualitative data were demonstrated as number and percentage. Paired t-test and chi square test were used to study differences between quantitative and qualitative data at baseline and after 6 PRP injections. Spearman’s correlation coefficient analysis was performed to identify factors associated with better functional outcomes. A statistically significant cutoff value was set at P < 0.05.
4. Results
4.1. Participants’ Characteristics
Demographic data and clinical findings of our studied patients (PRP and non-PRP groups) are shown in Table 1. There was no statistically significant difference between both groups, (P < 0.05).
| PRP Group (N = 15) | Non-PRP Group (N = 15) | P Value | |
|---|---|---|---|
| Gender | 1.000 | ||
| Male | 14 (93.3) | 13 (86.7) | |
| Female | 1 (6.7) | 2 (13.3) | |
| Age, y | 27.7 ± 2.9 | 30.1 ± 4 | 0.068 |
| Height, cm | 173.1 ± 5.8 | 173.5 ± 8 | 0.876 |
| Weight, kg | 81.7 ± 14.4 | 77.1 ± 13.6 | 0.376 |
| BMI, kg/m2 | 27.2 ± 4.3 | 25.5 ± 3.3 | 0.230 |
| Operated side | 0.464 | ||
| Right | 7 (46.7) | 9 (60) | |
| Left | 8 (53.3) | 6 (40) | |
| Mechanism of injury | 0.273 | ||
| Significant trauma | 9 (60) | 6 (40) | |
| Repeated micro traumata | 6 (40) | 9 (60) | |
| Site of tear (zone of injury all were within the peripheral 10% to 30% of the meniscus) | |||
| Middle and posterior third of the medial meniscus | 8 (53.3) | 6 (40) | 0.414 |
| Middle and posterior third of the lateral meniscus | 7 (46.7) | 9 (60) | 0.464 |
| Tear pattern | 1.000 | ||
| Vertical longitudinal | 11 (73.3) | 11 (73.3) | |
| Transverse radial | 4 (26.7) | 4 (26.7) | |
| Chondral lesion at time of arthroscopy | 2 (13.3) | 3 (20) | 1.000 |
| Technique of meniscal repair | 1.000 | ||
| Inside out | 11 (73.3) | 12 (80) | |
| All-inside | 4 (26.7) | 3 (20) | |
| Local tenderness | 15 (100) | 13 (86.7) | 0.483 |
| Effusion | 9 (60) | 8 (53.3) | 0.713 |
| Instability | 2 (13.3) | 5 (33.3) | 0.390 |
| Alignment | 0.705 | ||
| Mild varus | 6 (40) | 5 (33.3) | |
| Normal | 9 (60) | 10 (66.7) | |
| Muscle wasting | 6 (40) | 5 (33.5) | 0.705 |
| ROM | 1.000 | ||
| Full | 10 (66.7) | 10 (66.7) | |
| LLD | 5 (33.3) | 5 (33.3) | |
| VAS | 9 (7 - 10) | 8 (5 -8) | 0.09 |
| KOOS scale | 62 ± 9.8 | 66.3 ± 8.7 | 0.217 |
Abbreviations: KOOS, knee injury and osteoarthritis outcome score; PRP, platelet rich plasma; VAS, visual analogue scale.
aValues are expressed as mean ± SD or No. (%).
bQualitative data were described using number and percent and was compared using Chi square test or Fisher Exact test, abnormally distributed data were expressed in median (min. - max.) and were compared using Mann Whitney test*, while normally distributed quantitative data were expressed in mean ± SD and were compared using student t-test Statistically significant at P ≤ 0.05.
4.2. Clinical Outcomes Comparison Analysis
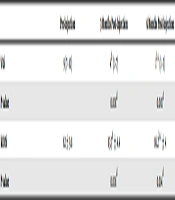
Comparison between pre-PRP injection (baseline), 3 months and 6 months post-PRP injection within the studied PRP-patient group regarding VAS and KOOS findings are reported in Table 2. There was a statistically significant decrease in VAS assessment at 3 months and more at 6 months post-PRP injection. Moreover, KOOS assessment was significantly increased at 3 months and more at 6 months following PRP injection.
Abbreviations: KOOS, knee injury and osteoarthritis outcome score; VAS, visual analogue scale.
aNormally quantitative data was expressed in mean ± SD and was compared using student t-test
bSignificant between pre and other periods.
cSignificant between 3 and 6 months.
dStatistically significant at P ≤ 0.05.
Comparison between both groups according to the VAS and KOOS findings at pre-injection, 3 months and 6 months post-injection are demonstrated in Table 3. There was statistically significant difference between both groups regarding both parameters at 3- and 6-months post-injection. The PRP-injected group showed more decrease in VAS assessment as well as more increase in KOOS assessment than non-injected group along the follow up periods (3 and 6 months post-injection).
Abbreviations: KOOS, knee injury and osteoarthritis outcome score; PRP, platelet rich plasma; VAS, visual analogue scale.
aNormally quantitative data was expressed in mean ± SD and was compared using student t-test
bSignificant between pre and other periods.
cSignificant between 3 and 6 months.
dStatistically significant at P ≤ 0.05.
4.3. Ultrasonographic Imaging Outcomes Comparison Analysis
Ultrasound findings of both groups and comparison between different parameters pre-injection (baseline) and 6 months post-injection are demonstrated in Table 4. There was significant decrease in the percent of degeneration of all US measurements between pre-injection and 6 months post-injection in both groups. Moreover, there was statistically significant difference between both groups according to the total change in the US findings after 6 months.
| US Findings | PRP Group | Non-PRP Group | P Value |
|---|---|---|---|
| MFC | |||
| Pre-injection | 2.5 ± 0.5 | 2.4 ± 0.5 | 0.725 |
| 6 months post-injection | 2.2b± 0.5 | 2.1b± 0.4 | 0.366 |
| % of degeneration | ↓9.7 ± 4.6 | ↓13.4 ± 5.6 | 0.059 |
| LFC | |||
| Pre-injection | 2.1 ± 0.4 | 2.2 ± 0.4 | 0.489 |
| 6 months post-injection | 2b± 0.4 | 2.1b± 0.4 | 0.562 |
| % of degeneration | ↓1.7 ± 2.5 | ↓2.2 ± 2.5 | 0.623 |
| MTC | |||
| Pre-injection | 2.6 ± 0.5 | 2.6 ± 0.4 | 0.782 |
| 6 months post-injection | 2.4b± 0.5 | 2.2b± 0.5 | 0.338 |
| % of degeneration | ↓9.7 ± 7.6 | ↓14.7 ± 7.9 | 0.089 |
| LTC | |||
| Pre-injection | 3 ± 0.5 | 2.7 ± 0.5 | 0.202 |
| 6 months post-injection | 2.9b± 0.5 | 2.6b± 0.5 | 0.122 |
| % of degeneration | ↓3.3 ± 4.1 | ↓5.3 ± 4.7 | 0.209 |
| Total US findings | |||
| Pre-injection | 10.12 ± 1.76 | 9.87 ± 1.62 | 0.693 |
| 6 months post-injection | 9.51 ± 1.80 | 8.99 ± 1.56 | 0.398 |
| % of degeneration | ↓6.16 ± 3.33 | ↓9.07 ± 3.66 | 0.031c |
Abbreviations: LFC, lateral femoral condyle; LTC, lateral tibial condyle; MFC, medial femoral condyle; MTC, medial tibial condyle; PRP, platelet rich plasma; US, ultrasonography.
aNormally quantitative data was expressed in mean ± SD and was compared using student t-test.
bSignificant between pre and other periods.
cStatistically significant at P ≤ 0.05.
4.4. Complications
No complications were noted among patients who enrolled in our study.
5. Discussion
In the current study, a statistically significant improvement was observed regarding pain (as assessed by VAS), knee function (as assessed by KOOS) as well as total ultrasound cartilage thickness (calculated as % of change) between both groups (PRP and non-PRP injected patients) at 6 months after PRP injection. In addition, there was statistically significant decrease in pain (by VAS) and increase in knee function (by KOOS) within the studied PRP-patient group between baseline, 3 months and 6 months after injection.
5.1. Previous Studies and Interpretation of the Results
In agreement with our findings, Pujol et al. (24) reported that PRP can slightly improve clinical outcomes, following open repair for horizontal cleavage. More recently, Kaminski et al. (25) found that PRP augmentation in meniscus repair results in a significant improvement in the rate of meniscus healing and improves the chances of meniscus healing by over six times with low adverse events related to it. They used MRI in follow up assessment but we favor the use of US as it’s an easy, rapid, as well as cost efficient method. On the other hand, Griffin et al. (26) found that outcomes, specifically International knee documentation scale and Tegner Lysholm knee scale scores, as well as clinical and patient-reported outcomes, as postoperative ROM, return to work, and return to sports/baseline activity after meniscus repair with and without PRP appear similar with no favor for PRP injection and there was no difference in any of these outcome measures between those patients who had PRP and those who did not. This disagreement may be due to several factors; firstly, they had done only one intra-surgical PRP injection not followed by repeated post-operative injections, secondly, lack of objective follow up measures as US or MRI findings, thirdly, no specific surgeon had done the arthroscopic meniscal tear so they have a confounding factor in their results, and finally, lack of power and nature of the study they reported in their work.
Interestingly, we found decrease in the percent of degeneration for each parameter measured in ultrasound before and 6 months after injection in both groups (injected and non-injected) but of no statistically significant level. This may be due to the small sample of our studied patients and short time of follow up. As noted by Cole et al. the value of PRP use in meniscal repair is the possibility of delivering a local concentration of growth factors and other cytokines directly to the repair site (18). The appeal of this is to enhance meniscal vascularity.
5.2. Clinical Implementation
The meniscus is critical for the knee's health and function, but is often injured especially in young athletes in whom unnecessary intervention with secondary cartilage destruction and joint failure may be unfavorable to a competitive future. Recently, greater efforts have been made to determine a more durable alternative to meniscectomy, as the procedure results in increased contact stresses on the articular surface of the knee (27, 28). Meniscal repairs have been studied extensively but are still failing for a number of reasons. The lack of vasculature that provides intrinsic nutrition is believed to be a reason for poor cure (29). The use of PRP was demonstrated to increase healing by introducing a higher concentration of multiple growth factors in the area of meniscal repair (30). The experimental studies’ results support the hypothesis that PRP could improve meniscus healing by activating fibro-chondrocytes in the avascular regions of the meniscus (31). The growth factors released from platelets are thought to be associated with the healing cascade initiation, with an increase in the deoxyribonucleic acid and extracellular matrix synthesis (32). To our knowledge, the previous research works considering this scope had done only one intra-operative PRP injection at the time of meniscal repair, not followed by other repeated PRP injections to study the maximal effect of it on augmenting the meniscal healing process.
The strengths of our study are its prospective, randomized, and blinded nature and the use of standard repair techniques by a single surgeon. In addition to objective measuring assessment tools by a single radiologist using US.
Limitations of our study are small number of the studied patients as well as short period of follow up.
5.3. Conclusions
At the end of our work we can conclude that intra articular PRP knee injection after arthroscopic meniscal repair may be effective in reduction of pain, improvement of knee function, and decreasing the percentage of cartilage degeneration following meniscal repair.