1. Introduction
Acute colonic pseudo-obstruction (ACPO) or Ogilvie syndrome is a rare condition identified with colon dilatation without any mechanical obstruction, usually involving caecum and right hemi-colon. ACPO usually occurs following a surgery, mostly after cesarean section, and rarely occurs spontaneously (1, 2).
The symptoms or signs of ACPO, which are related to bowel obstruction, include abdominal pain or tenderness, nausea and/or vomiting, constipation, and fever. Early diagnosis of ACPO is critical because of its subsequent morbidity, including bowel ischemia, necrosis and perforation, and colon torsion; its mortality rate can also reach 50% (3, 4).
Although pseudo-obstruction of the colon has been investigated in previous literature, to the best of our knowledge, no case of pseudo-obstruction of the ileum has been reported so far. Herein, for the first time, we report a case of pseudo-obstruction of the ileum following a total laparoscopic hysterectomy (TLH) treatment because of menorrhagia.
2. Case Presentation
A 40-year-old woman with a chief complaint of prolonged and heavy menstrual bleeding resistant to medication therapy was a candidate for a total laparoscopic hysterectomy at our hospital. She had a history of two cesarean sections with no remarkable past medical history.
Before the surgery, bowel preparation was performed with two dimeticon tablets and two bisacodyl rectal suppositories. Deep vein thrombosis prophylaxis with enoxaparin was given, and cefazolin was administrated as antibiotic prophylaxis.
Surgery was performed under general anesthesia. There was no remarkable finding in abdominopelvic exploration. Uterus, fallopian tubes, and ovaries were normal. There were no bowel adhesions or evidence of endometriosis. The total operating time was 75 minutes with minimal intra-operation blood loss.
On the second postoperative day, the patient complained of rising abdominal pain in the right upper quadrant. She tolerated a liquid diet without nausea or vomiting. She also passed flatus. There was no abnormal finding in her physical exam except for a mild abdominal distention.
On the third postoperative day, she suffered from watery diarrhea. Oral intake was prohibited, and intravenous fluids were started. Her abdominal imaging, including abdominal x-ray and computed tomography (CT) scan were normal. Increasing C-reactive protein (CRP) level was the only positive finding in her lab tests.
On the fourth postoperative day, diarrhea ceased, and there was no change in abdominal distension. The abdominal pain decreased substantially. She asked for discharge, but due to a significant increase in quantitative serum CRP level, the gynecologist decided to continue hospitalization for close observation, and conservative management continued.
On the fifth postoperative day, abdominal distension progressed and bilious vomiting occurred. Physical examination demonstrated generalized abdominal tenderness. General surgery consultation was requested, and emergent laparotomy was scheduled for clinically suspected bowel problems resistant to conservative management. The rapid deterioration within 24 hours did not allow new imaging requests.
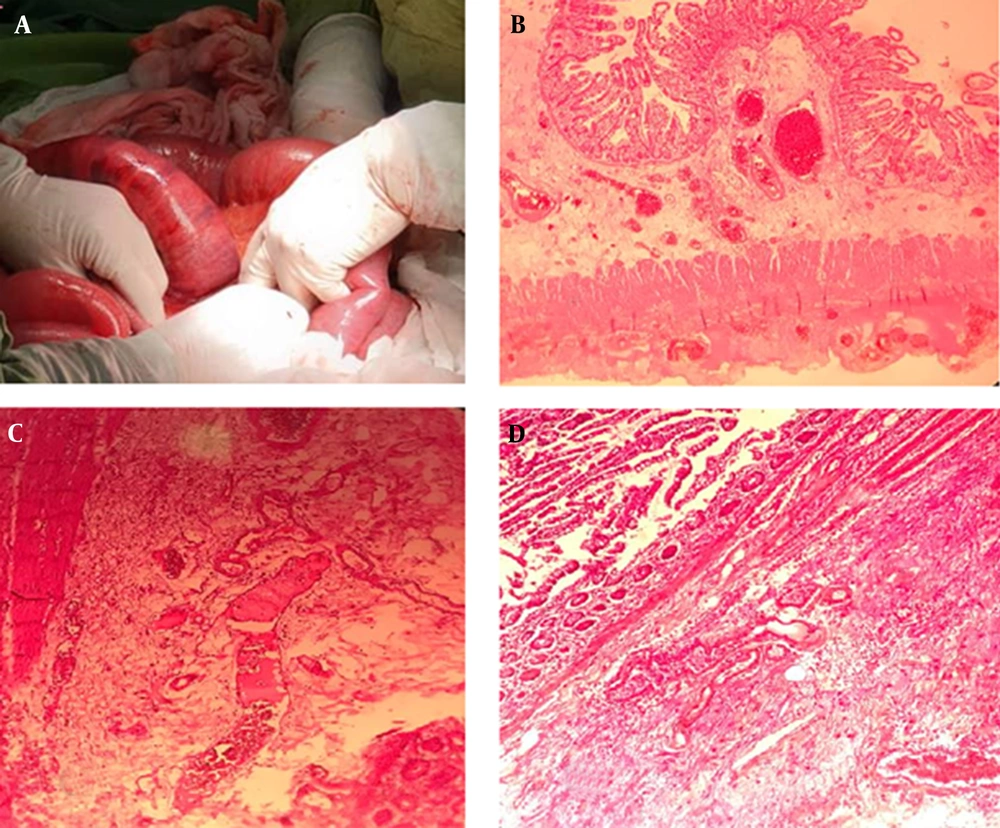
During re-operation, the previous surgical site was normal. There was no suspicious lesion of thermal injury on the rectosigmoid and colon. The small bowel was dilated and congested about 30 cm proximal to the ileocecal junction. The condition necessitated segmental bowel resection and re-anastomosis. No other bowel injury was identified. There was no mass or band, or loop to propound mechanical obstruction. Histopathology report of the resected bowel showed ischemia secondary to congestion (Figure 1A-D). The patient's postoperative course was satisfactory, and she was discharged on day 15.
3. Discussion
The definite pathogenesis mechanism of ACPO remains unclear. However, change in the balance of bowel parasympathetic and sympathetic function, secondary to predisposing clinical condition and trauma to spinal and retroperitoneal area, are the probable causes (5).
Without considering the cause of ACPO, its early detection and proportion management can significantly reduce the related morbidity and mortality following intestinal ischemia and perforation (5, 6).
Although the features of ACPO can present rapidly over the first 24 hours after the surgery, the average time for developing ACPO manifestation was five days post-operation. ACPO diagnosis is done mostly according to the patient's symptoms and signs and imaging findings. The common ACPO features include abdominal distension, abdominal pain, nausea, and vomiting (6).
However, in our case, since the functional obstruction was in the small intestine (ileum), the related symptoms progressed slowly, and abdominal, and bowel distension was not significant in early physical examination and imaging, respectively. So, the diagnosis was done according to the post-operation CRP level rising.
Former evidence investigated the important role of CRP in the early diagnosis of anastomotic leakage following colorectal surgery. Furthermore, it seems that the increasing CRP level in open or laparoscopic surgeries is an important clue to diagnose cases with major post-surgery complications (7, 8).
While it is expected after 48 hours in uncomplicated surgery, the CRP levels decrease and return to their normal ranges (9). In our study, the lack of CRP decline on day 2 after surgery was the key point for more investigation and the absence of her discharge.
ACPO after total laparoscopic hysterectomy (2) or laparoscopic appendectomy (10) were reported; in this study, we identified a rare case of ACPO following a gynecologic minimally invasive surgeries.
3.1. Conclusions
The CRP value can help to predict latent complications. It is also necessary to observe these patients closely to detect and manage probable post-operation complications.