1. Background
Despite the relative control of COVID-19 by vaccination, we are facing a new wave of disease with increasing hospital administration. Until now, more than half a billion people have been affected globally. The long-term sequels of SARS-CoV-2 are not limited to the respiratory system, and the complications at one-year post-infection included fatigue, erythromelalgia, depression, and anxiety (1).
Women's menstruation cycle is under the delicate regulation of the hypothalamic-pituitary-ovarian (HPO) axis. The disturbance in this axis can result from any derangements in the normal hemostasis of the human organs, including infections and other febrile illnesses, mental stresses, and certain medications (2). This malfunction results in alterations in the volume, length, frequency of bleeding, inter-menstruation bleeding, and spotting. Meanwhile, Ovarian cells express ACE2 receptors (3). SARS-COV is known to have affected ACE pathways, indicating that COVID-19 infection or vaccination against COVID-19 can lead to menstrual disturbance (4, 5).
2. Objectives
Hormonal disturbances should be considered in patients with COVID-19 and post-COVID-19 syndrome (6). Although COVID-19 vaccines reduce mortality and morbidity rates, it is essential to understand potential complications and side effects. Therefore, this study aimed to evaluate short-term menstrual distributions after COVID-19 infection and determine whether vaccination and type of vaccine could alter menstrual cycles.
3. Methods
3.1. Study Design and Participants
In this online survey study, the participants were asked about possible alterations in their menstruation cycle features. The inclusion criteria were women aged between 18 and 45 years with regular menstrual cycles who had confirmed COVID-19 infection by the positive result of a polymerase chain reaction (PCR) test. The exclusion criteria were current pregnancy and/or lactation within the last one-year, using hormonal contraceptives, a positive history of gynecologic surgeries, including hysterectomy, oophorectomy, and tubal ligation, and positive history of the following conditions: Polycystic ovarian syndrome (PCOs), endometriosis, pelvic adhesions, uterine fibroids, uterine polyps, pelvic inflammatory disease (PID), primary ovarian failure (POF), and infertility. The participants were asked about the changes in their duration of menstruation and cycle, irregular cycles, the volume of bleeding in each cycle, exacerbation of premenstrual syndrome (PMS), dysmenorrhea, and intermenstrual bleeding (IMB). The history of using vaccines before COVID-19 infection was also recorded, and the menstrual irregularity (if occurred) was compared between the vaccine types. All participants followed at least three months after COVID-19 infection.
3.2. Statistical Analyses
Data were represented using frequencies for categorical variables, mean ± standard deviation (SD), and n (%) as appropriate for continuous variables. The Χ2 test and independent-sample t-test were used to compare two by two contingency data and continuous data between the groups, respectively. Statistical analyses were conducted using SPSS Statistics for Windows, Version 27.0 (IBM Corp, Armonk, NY, USA). A P-value < 0.05 was considered statistically significant.
3.3. Ethical Approval
All participants accepted and signed the online informed consent. The study was approved by the Iran University of Medical Sciences ethics committee (IR.TUMS.IKHC.REC.1400.351). This study was conducted according to the principles of the Helsinki Declaration.
4. Results
Totally, 268 (46%) individuals participated in the study. The mean ± SD age of the participants was 36.2 ± 6.4 years. Sixty-two individuals (23.1%), with a mean age of 36.6 ± 5.8 years, had alterations in at least one of their menstruation-related parameters. In this regard, 46.7% had IMB, 66.1% experienced exacerbation in PMS, 67.7% had increased bleeding volume, and 62.9% had dysmenorrhea or exacerbation in dysmenorrhea. Also, 27.4% and 35.4% experienced a shorter or longer duration of menstrual cycles, respectively. All menstrual cycle distributions returned to normal after a maximum of two cycles.
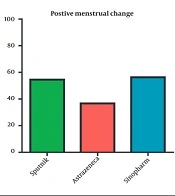
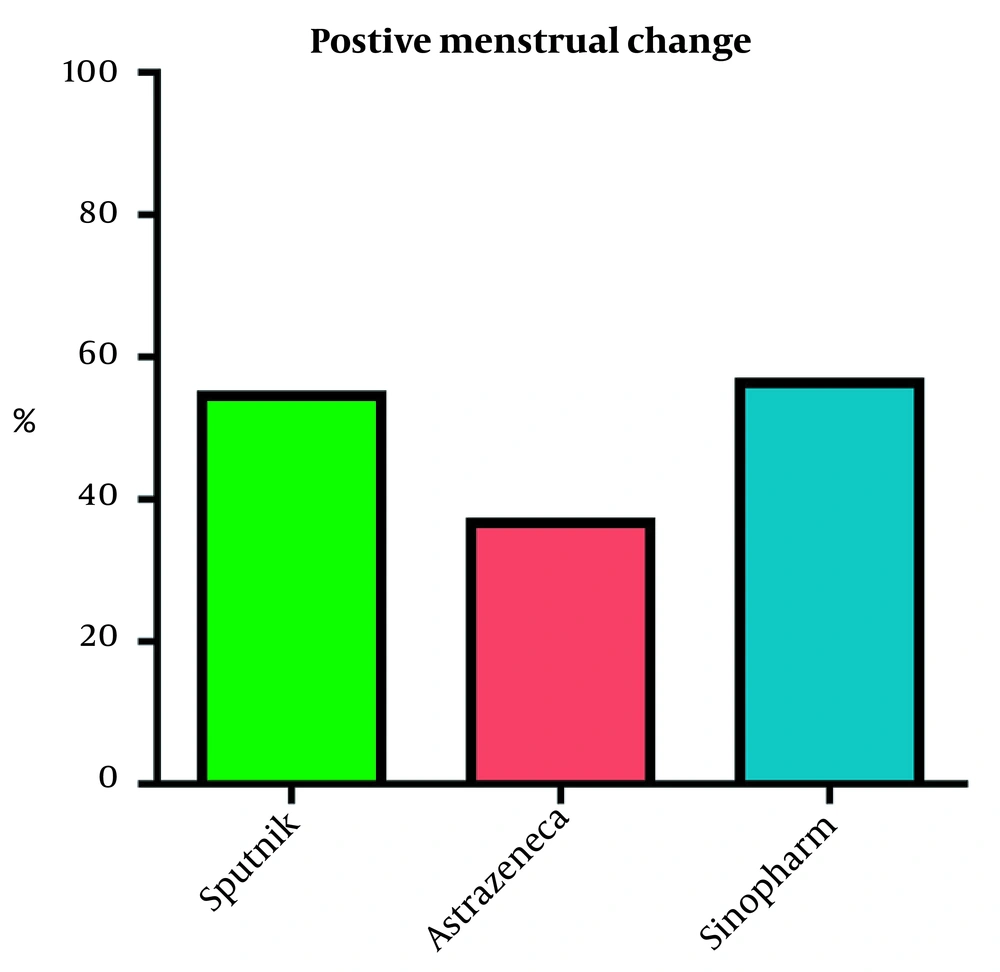
Due to the fact that the majority of participants were vaccinated (before COVID-19 infection) by three vaccine types (Sputnik, Sinopharm, and AstraZeneca) available, we assessed whether the individuals experienced menstrual irregularity after vaccination. Surprisingly, we found a significant difference between patients receiving AstraZeneca and those receiving Sinopharm (Pearson chi-square: 5.12, P-value: 0.024) (Figure 1).
5. Discussion
This study demonstrates that menstrual distribution is primarily common among reproductive-age women. Our data shows a substantial difference between the AstraZeneca 19 vaccine and the Sputnik and Sinopharm vaccines, as the number of patients who experienced changes in duration was relatively lower.
This is the first time the menstrual distributions are compared between COVID-19 vaccine types. Although, few studies have evaluated the effects of COVID-19 on the menstruation cycle. The result of a survey study has shown that 54% of participants (who have been U.S. residents) have experienced alterations in their menstrual cycle (including 54% in length, 50% in PMS, and 34% in the duration of menses). In addition, this study has found a correlation between perceived stress scale scores with the duration and volume of bleeding episodes (7). In a Turkish study of 952 female healthcare workers, about 29% reported having irregular menstrual cycles, similar to ours. In addition, such individuals have had higher COVID-19 Stress Scales scores than those with regular menses. Univariate and multivariate logistic regression models have also corroborated this difference (8).
Of note, the prevalence of menstrual disorders has been higher than that of the general Turkish female population (8). The descriptions of another Turkish study further corroborate the increased frequency of menstrual abnormalities after the spread of COVID-19 infection (9).
However, the findings regarding the trend in the frequency of menstrual disorders are discordant. For example, in a survey-based study from Jordan, the rate of menstrual problems during the total curfew has decreased from 17.5% to 10.5% (10). Likewise, a survey study on Turkish women has reported the decreased duration of menses and pads used per day compared to each individual’s parameters before the pandemic (11).
The detrimental effects of psychological stresses on the menstruation cycle are evidenced decades ago (12). For instance, post-earthquake middle students (13) and females that have experienced a short period of war (14) have higher complaints about menstrual abnormalities. It seems that the fluctuations in the sympathetic activity will affect the neural activities of the amygdala and medial prefrontal cortex, thereby causing abnormal alterations in the level of pregnanolone, with the net result of menstrual abnormalities (15). Another study has found that pre-menopausal women with higher stress levels experience shorter durations of their intermenstrual cycles and bleeding episodes (16). Also, regarding the impact of stress on the menstrual cycle, we have found that the alterations are only limited to the irregularity of menses and not the volume and duration of menses (17). The detrimental effects of COVID-19 infections on ovarian function and reserve are also reported (18).
Our study faces several limitations. There was no control group (i.e., without recent COVID-19 infection) to further delineate the relationship between COVID-19 and menstrual abnormalities. Moreover, our survey did not include any additional questionnaires to evaluate the level of stress and anxiety among the respondents.
5.1. Conclusions
Menstrual distributions are common but temporary in the short term following COVID-19 infection in women of reproductive age. Although, the recombinant vaccine (AstraZeneca) was associated with lower menstrual disturbance rates compared to the Sinopharm and Sputnik vaccines. Further large-scale studies evaluating the HPG axis serum markers are required to decipher this dilemma appropriately.