1. Background
Stillbirth is defined as the death of a fetus after 20 weeks of pregnancy. There are some established risk factors for this condition, including nulliparity, advanced maternal age, minority ethnic groups, hypertension, maternal obesity, and smoking (1). Pregnancies leading to stillbirth are more frequently associated with dramatic changes in fetal movements in the last two weeks (2). Therefore, monitoring fetal movement could be a simple and effective approach to assessing fetal wellbeing. In this regard, maternal perception of reduced fetal movements (RFM) has attracted particular research attention (3).
RFM can be a sign to alert physicians that pregnancy is at risk. It has been argued that RFM is associated with placental dysfunction and, as the result, it may produce adverse outcomes in pregnancy (4). Several recent studies have suggested that excessive fetal movement, in addition to RFM, can be a risk factor negatively contributing to stillbirth (2, 5). In contrast, some other studies have found that fetal hyperactivity produces no adverse outcome (6). The pattern of hyperactivity is controversial but important to estimate the prognostic risk (7). The present study aimed to report a case of stillbirth with increased perceived fetal movements in the last week of pregnancy in the 34th week of gestational age.
2. Case Presentation
A 32-year-old woman in week 34th of her first pregnancy attended the emergency room while she had no chief complaint of fetal movement from the previous night. She had no medical or surgical history, and she had a wanted, spontaneous pregnancy. Routine prenatal screening and laboratory test results showed no significant problem or adverse pregnancy outcome in our case. She had attended all prenatal visits in a private clinic under an obstetrician supervisor. The results of ultrasound scanning, including anomaly scan, had been normal, and no anomaly had been detected. The last ultrasound had been performed in 32th week of gestational age with a normal Doppler study, but no sign of fetal distress or placental dysfunction had been observed.
She had attended her physician one week earlier and reported an increased perception of fetal movements. In the physical examination, the fetal position had been transverse, and fetal heart rate (FHR) of 144 beats/minute had been recorded. The physician had reassured her and warned her about the signs such as bleeding, decreased fetal movement, and rupture of membrane.
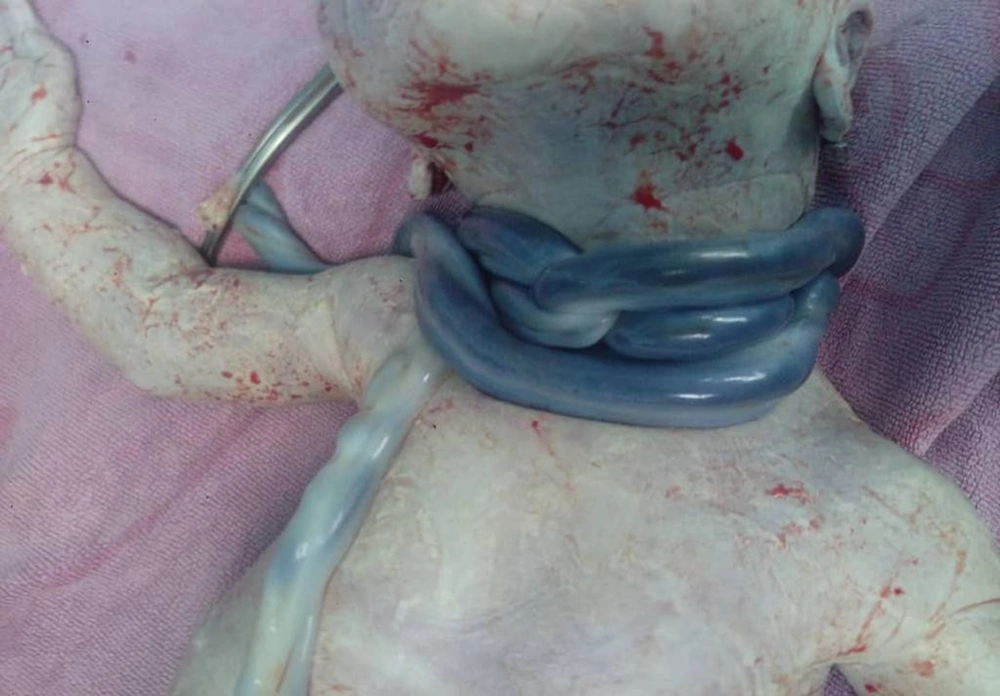
In her visit to the emergency room, the physical examination result was normal. Blood pressure was 115/77 mmHg, and ultrasound scanning revealed breech position of the fetus with no cardiac activity. The lab data, including complete blood count (CBC), liver, renal, and coagulation tests were in the normal range. She underwent cesarean section upon her request and delivered a macerated stillborn girl with triple loops of tied nuchal cord (Figure 1). Fetal weight was 2450 grams and the full body x-ray image was reported normal.
In the follow-up stage, she was discharged after 48 hours. Placental pathology was normal, and the parents did not consent to send the embryo to the laboratory for further genetic evaluation.
3. Discussion
Mother perception of fetal movement has long been known as a factor suggesting fetus health condition. IFM has a clear association with late stillbirth (3). This association is explained through placental dysfunction leading to insufficiency of oxygen and nutrients. The fetus copes with deprivation firstly by restricting the growth and then by activating mechanisms such as re-direction of blood flow to more essential organs (e.g., brain sparing effect) and reduction of energy consumption through reducing movements. If the dysfunction resumes, ultimately fetal demise may occur (4).
Increased fetal movement is a more controversial finding. It has been long considered a reassuring fact (8), but some studies have reported that sudden excessive fetal movement reflects acute fetal distress and IFM is actually the attempt of fetus to resolve an existing problem (e.g., chord compression or nuchal chord) (9). Another potential cause of IFM is fetal seizures due to structural, intracranial, and metabolic abnormalities in the fetus (10).
Most of these potential pathological explanations cause a single episode of IFM followed by RDM and fetal demise, whereas multiple episodes of increased strength or frequency in fetal movements are assumed normal and reassuring or even protective (5, 8). Therefore, it is important and challenging to differentiate between patterns of IFM.
Our case reported episodes of IFM within a week, which is not usually considered worrisome. This case may have been attributed to two risk factors: First, an acute pathological event caused distress for the fetus and, therefore, the fetus increased the movements in order to cope with the risky situation; or some seizure activities occurred. Potential distress in this case can be the triple loop nuchal chord or asphyxia. In this scenario, the main reason for stillbirth is distress, and IFM is just a representative of the event, but not the main cause of stillbirth. Second, fetal activity increased physiologically and, regarding the transverse position of the baby, the resulting movements caused nuchal chord; therefore, dysfunction of oxygen and nutrient delivery was the main cause of fetal demise.
3.1. Conclusions
Contrary to our expectation, the pattern of IFM detected in this case was not associated with or the result of stillbirth. Moreover, studies on the given issue have produced controversial findings and it’s not still clear when exactly a pregnant woman with IFM should be closely monitored. Most of the studies investigating alternation in fetal movements are in case-control design and are unlikely to be free from biases such as recall and negativity biases. Therefore, it was suggested that the alteration in fetal movement should be further evaluated. It was also recommended that further prospective studies should be carried out in order to clarify the association between IFM patterns and pregnancy adverse outcomes.