Dear Editor,
More than a third of maternal deaths, half of the stillbirths, and a quarter of neonatal deaths result from complications during childbirth (1). Two seminal studies regarding the partograph were published in 1972 (2). The partograph is a simple, inexpensive, and cost-effective tool that provides a continuous graphic overview of labor and prevents prolonged and obstructed labor (3). Despite widespread support from health experts, there are concerns that the partograph has not yet fully realized its potential to improve treatment outcomes. Even though it is widely used, there have been reports of utilization and correct completion rates as low as 31% and 3%, respectively (2).
In February 2018, the World Health Organization published a consolidated set of recommendations on prenatal care for a positive birth experience (4). In response to recent evidence, including a better comprehension of the individual variability of the progress of labors leading to positive perinatal outcomes and many women not having labors that progress at the average rate on which the partograph design was based, the World Health Organization (WHO) started a process to update the partograph (2). So far, the partograph has undergone many changes, and studies have been conducted to investigate the obstacles and factors affecting it (5).
The partograph recommended by the WHO is based on the work of Friedman and Philpott and a guideline based on Zhang's research (6). The new partograph aims to diagnose maternal and fetal problems more quickly (7). The labor care guide is a simple tool to monitor delivery to reduce the rate of early cesarean deliveries (8). One of the causes of death among pregnant mothers is uterine rupture, and many deaths caused by uterine rupture are preventable. With the labor care guide, these problems can be prevented to some extent by recognizing the warning signs and reacting in time (9).
The labor care guide is designed for all deliveries in health centers, including primary, secondary, and tertiary care centers. Women who give birth in low-level centers may be referred to a higher level if needed, and this roadmap can promote women-centered care (10).
The difference between the labor care guide and the partograph is in dealing with labor length and focusing on maintaining the mother's safety (5). Alterations to the Labour Care Handbook include the following: During the active first stage of labor, evidence-based time limits at each centimeter of cervical dilatation replaced the 1 cm/hour 'alert' line and its corresponding 'action' line; the cervical dilation of 5 cm marks the beginning of the first stage of active labor (instead of 4 cm or less); during the second stage, a monitoring section was added; a part that evaluates and encourages the utilization of supportive care to improve the entire delivery experience; the intensity of uterine contractions, which is challenging to clinically measure and standardize, is no longer recorded; it mandates that any labor parameter observations that deviate from predicted observations be noted, and the provider must record the relevant reaction (2).
In the partograph, two lines of awareness (alert) and action (action) were determined. Still, in the labor care guide, the delivery progress is checked differently, and each person is compared with himself and with warning signs (containing the reference threshold).
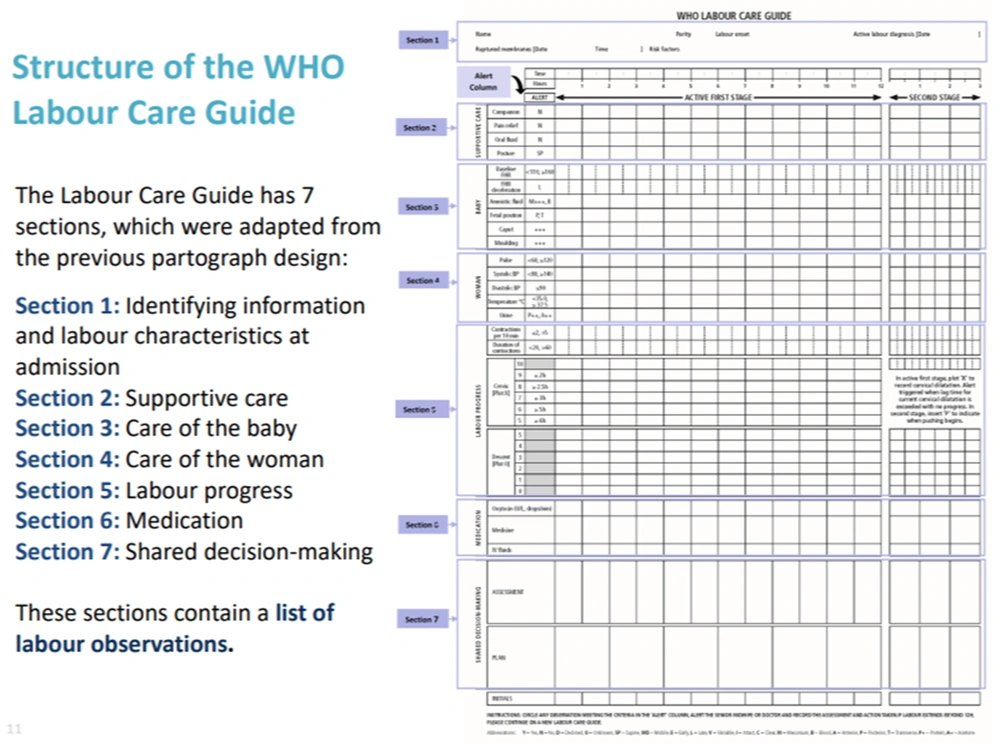
The pregnancy care guide has seven sections adapted from the previous partograph design. These sections are as follows (Figure 1):
World Health Organization (WHO) labor care guide (11)
(1) Identification of the person's information and the state of delivery at the time of admission; (2) supportive care; (3) neonatal care; (4) women care; (5) childbirth progress; (6) medications; and (7) shared decision-making.
According to WHO recommendations, respectful maternity care is a basic human right for pregnant women and is the core of prenatal care.
Effective communication between maternity care providers and women in labor, using simple and culturally acceptable methods, is recommended by the World Health Organization.
Clear explanations about the actions and their purpose should be provided to each woman. The physical examination findings should be explained to the pregnant woman and her companion, and the next course of action for shared decision-making should be clarified. To ensure the systematic and consistent application of maternity care guidelines, health providers are encouraged to use the assessment, record, review, and decision scheme.
Supportive care includes having a companion and using analgesia methods, oral fluids, and the position of the pregnant mother. In fetal care, her health is monitored by regular monitoring of the basic fetal heart rate (FHR), the reduction in FHR and amniotic fluid, fetal position, fetal head molding, and development of caput succedaneum (diffuse swelling of the scalp) are among the things that should be considered.
In the maternal care department, vital signs are noted and compared with abnormal thresholds. In the next stage, attention is paid to the progress of childbirth, and the status of the progress of childbirth is checked with abnormal thresholds and new definitions.
The next part is the administration of injectable fluids and drugs; finally, the table's last part is shared decision-making.
The purpose of this section is to facilitate continuous communication between the pregnant woman and her companion. Continuous recording of all assessments and agreed plans is desired.
To use this new guide, consultation with professors and practitioners can help to localize it. Appropriate educational and monitoring programs are also the determinant of this road map (11).