1. Background
Maintaining clinical competence is a critical component of professionalism in medicine, and competence requires knowledge and skills obtained through textbooks, medical journals, and experience (1). However, without proper programming for continuing medical education (CME), no physician remains competent for more than a few years after graduation (2). It is indicated that patient outcomes may be worse if physicians practice for longer periods (3).
Therefore, identifying the educational needs of clinicians and involving their participation increases effectiveness and improves medical service quality (4). Consequently, designing CME courses based on needs assessments improves physician performance (5).
The skills learned during the residency program may not meet a specialist’s new clinical challenges (6). Despite the standard educational curriculums in gynecology and obstetrics residency programs, there may be differences in access to resources, resident supervision, and evaluation between academic centers. Indeed, remaining updates for gynecologists and obstetricians are not always easy. Therefore, they may gradually accept specific or simple cases, which, especially in small cities, increases referrals without indication, thereby increasing the economic burden on the health system as well as the morbidity and mortality cases. One of the most critical maternal and neonatal health factors in rural areas is punctual access to competent healthcare providers in obstetrics and gynecology. It is known that the rates of primary and non-indicated cesarean delivery are higher in rural hospitals in the United States, which may be related to limitations in maintaining the skills of the staff (7). Therefore, initiating maintenance of certification (MOC) for physicians was the main purpose of many guidelines and programs (8).
On the other hand, there is a gap between the learning demands of physicians and the educational programs introduced by the stakeholders of continuing medical education (9). Learning needs are specific and personal, whereas educational needs usually are identified via questionnaires or evaluations of CME programs (10). To find and fill this gap, it is necessary to conduct an assessment system to evaluate clinical capability among gynecologists and obstetricians to design proper CME courses.
In many national curriculums in residency training, competency is assessed through a structured assessment program. For example, in the Australian curriculum, the program includes written and oral examinations and workplace-based assessments (11). It is proven that competency-based education is a vital component for practicing physicians to improve patient outcomes. Furthermore, several approaches for assessing physicians, including audit and multi-source feedback and direct observation, are introduced (12).
2. Objectives
To improve the quality of education, we took a new look at continuing education. We presented a more precise way to enhance the value of education and draw it from purely theoretical methods. Therefore, this study was designed to conduct an online clinical capability assessment questionnaire among gynecologists and obstetricians to understand their educational needs to have a further proper plan for its implementation.
3. Methods
3.1. Study Setting
An online self-administered questionnaire was sent as a hyperlink via social media to gynecologists and obstetricians who graduated from medical universities in Iran from July 2021 to August 2021. A total of 286 general gynecologists and obstetricians responded. The research project began after the ethical board approved the study. All participants signed electronic consent forms, and their privacy was respected. The inclusion criteria were all general gynecologists and obstetricians who graduated from universities in Iran. The subspecialized clinicians were excluded.
3.2. Questionnaire Design
A self-administered questionnaire was designed to obtain the educational needs of gynecologists and obstetricians. The questionnaire design was based on Stone considered the decision on what data we needed, selection of the issues for inclusion, designing each question, making the words, designing the layout, coding, preparing the draft, piloting, and evaluating the form and accomplish the questionnaire (13). This questionnaire had four parts:
Part 1: Demographic information, including age, having a private office, graduation date, university of graduation, being a faculty member, and their current working place, was asked. The level of cities was defined by population size.
Part 2: Clinical capability assessment in general skills such as stress management, legal knowledge, cardiopulmonary resuscitation, computer skills, and documentation.
Part 3: Based on the residency educational curriculum, clinical capability assessments of specialized skills, including medical and surgical management.
Part 4: The section that reports the clinician preference training method as virtual vs. practical vs. theoretical.
The validity of the questionnaire was evaluated by presenting it to five experts in medical education, gynecologists, and obstetricians. Experts were asked to rate the relevance and appropriateness of the questionnaire in a 4-point ranking. The scales are: 1 = inappropriate, 2 = slightly appropriate, 3 = appropriate and 4 = very appropriate. They were also asked to apply their corrective comments to the questionnaire. Expert opinions were analyzed, and the questionnaire’s validity was determined.
After editing and preparing the final version, the questionnaire link was sent to clinicians. The information obtained was recorded and analyzed on an online platform with high security.
3.3. Statistical Analysis
To analyze the data, we used descriptive statistics, including mean ± standard deviation and percentages. All analysis was performed by SPSS version 26, and a P-value is less than 0.05 considered significant.
4. Results
4.1. Respondents
In total, 286 gynecologists and obstetricians participated in the study and completed the questionnaire. All of them were women (35 years ago, all gynecologists in Iran were women). Their mean ± SD age was 48.7 ± 8.05 years. The demographic information of the participants is listed in Table 1. Most participants were non-academic staff (87.3%) and had private offices (61.3%). More than half of them had more than 10 years of experience in obstetrics and gynecology. Also, most (73.2%) graduated from type 1 universities and worked in big cities (77.9%).
| Demographic Information | Values |
|---|---|
| Age (y) | 48.7 ± 8.05 |
| Academic staff | |
| Yes | 36 (12.7) |
| No | 250 (87.3) |
| Private Office | |
| Yes | 175 (61.3) |
| No | 111 (38.3) |
| Graduation date (y) | |
| 0 - 2 | 30 (10.6) |
| 3 - 5 | 30 (10.6) |
| 6 - 10 | 42 (17.6) |
| > 10 | 184 (61.2) |
Demographic Information of the Gynecologist and Obstetricians (n = 286) a
4.2. General Skills
4.2.1. Stress and Anxiety Management
Approximately 93% of the participants had experienced severe stress during the treatment of patients. The common reasons were the mortality and morbidity of their patient (72.9%) following the possibility of patients’ complaints to legal authorities (20%). More than 70% believed the residency training was inadequate, and near to three-quarters needed practical bedside training in academic hospitals.
4.2.2. Morbidity and Mortality
Nearly 60% of clinicians have encountered severe morbidity and mortality cases during their careers. Near 40% of them believed the inefficiency of the medical team following the lack of experience (19.7%) and lack of facilities and equipment (15.1%) were the main concerns. More than 80% felt deficient in this area 68.8% believed residency training was insufficient to manage such cases. Most of them preferred practical bedside training in academic hospitals as CME courses.
4.2.3. Documentation
More than half of the participants (54.7%) had insufficient information in the documentation field, including file completion and informed consent, and 80% felt deficient in this area. Most of them preferred virtual CME in this field.
4.2.4. Legal and Ethical Knowledge
Nearly 80% had insufficient information about legal considerations in gynecology and obstetrics, more than 90% had insufficient residency training, and most preferred virtual or face-to-face theoretical training.
4.2.5. Computer Skills
It was reported that nearly half of the clinicians did not have enough experience using computers and searching scientific information in electronic sources, 93% were unsatisfied with residency training, and most preferred theoretical and virtual training.
4.2.6. Cardiopulmonary Resuscitation
Nearly 35% of the participants had insufficient skills in cardiopulmonary resuscitation and felt deficient (85%) in this area. In approaching shock, using blood products, and regulating water and electrolytes in unstable patients and neonatal resuscitation, the same concern is seen, and most clinicians prefer practical bedside training in academic hospitals.
4.2.7. COVID-19 Information
Nearly 70% knew how to deal with COVID-19 patients and new instructions; however, 81.4% needed more information, preferably through theoretical virtual training.
4.3. Obstetrics Skills
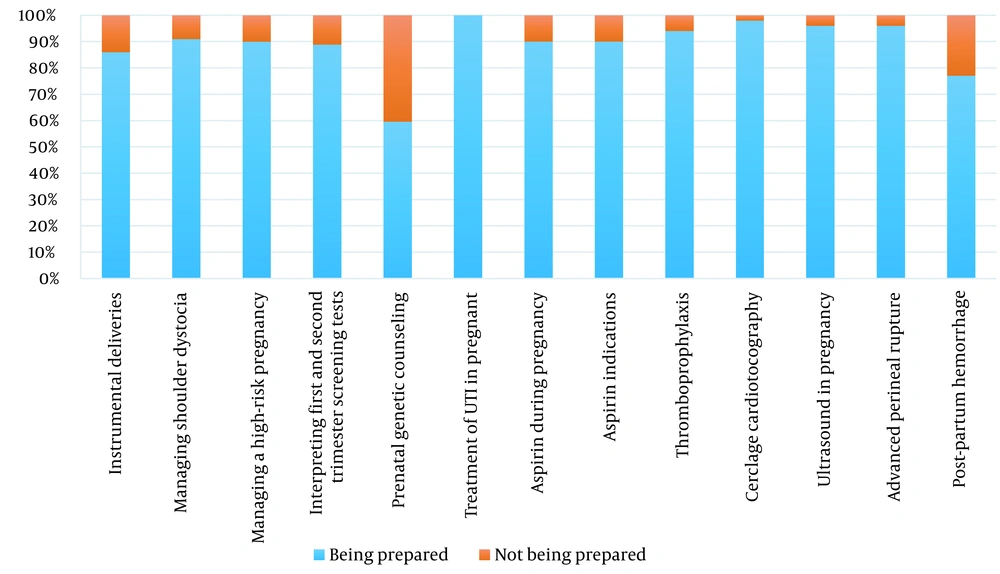
In obstetrics skills, we asked about instrumental deliveries, managing shoulder dystocia, managing a high-risk pregnancy, interpreting first and second-trimester screening tests, prenatal genetic counseling, treatment of urinary tract infection (UTI) in pregnancy, aspirin indications during pregnancy, thromboprophylaxis, cerclage, cardiotocography, ultrasound in pregnancy, advanced perineal rupture and post-partum hemorrhage. Respondents’ preparedness for obstetrics skills is summarized in Figure 1. Nearly 60% believed residency training was enough for these skills, although more than two-thirds of the participants felt they needed more training. The utmost educational challenge in this area was providing prenatal genetic counseling. Most clinicians preferred practical bedside training in academic hospitals for most skills.
4.4. Infertility Skills
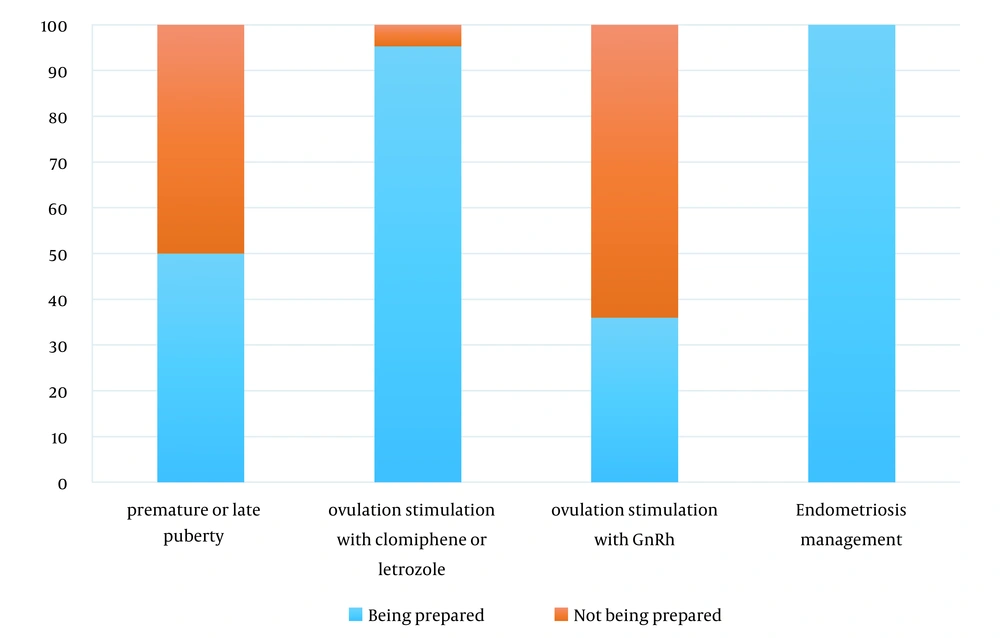
In infertility skills, we asked about managing premature or late puberty, ovulation induction with various regimens, and endometriosis management. Respondents’ preparedness for infertility skills is summarized in Figure 2. The lowest level of preparedness was in ovulation stimulation with GnRH and premature or late puberty management. On average, 70% were skillful, although more than 80% felt they needed more training. Figure 2 summarizes the preferred education method. Their preferred training methods were theoretical virtual training following practical bedside training in academic hospitals.
4.5. Gynecological Skills
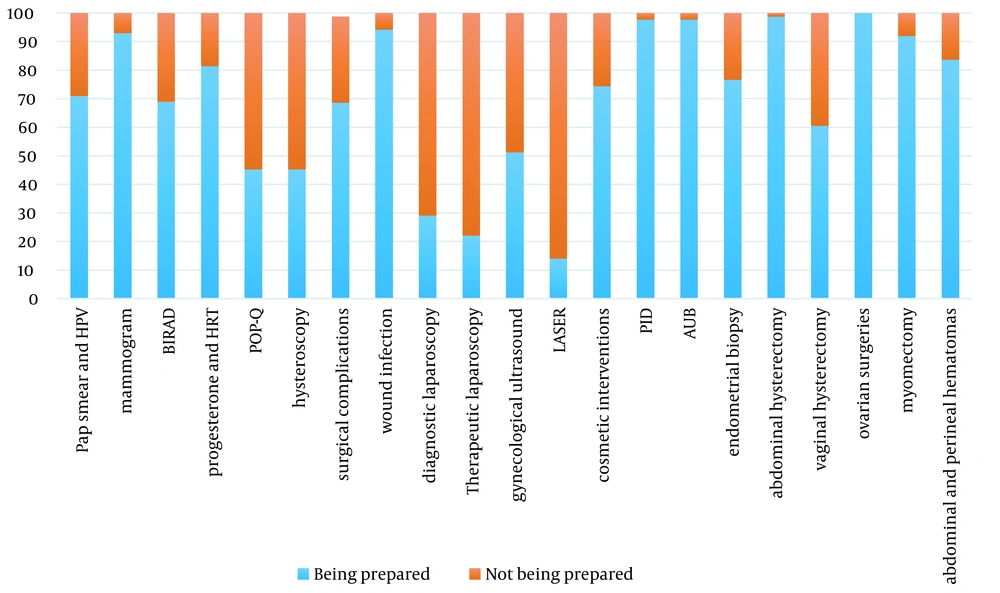
In gynecological skills, we asked about the management of pap smear and HPV, indications for requesting a mammogram and Breast Imaging-Reporting and Data System (BIRADS), hormone replacement therapy, hysteroscopy and laparoscopy, prolapse staging, surgical complication, wound infection, gynecological ultrasound, laser surgeries, gynecological cosmetic surgeries, pelvic inflammatory disease (PID) and abnormal uterine bleeding (AUB) management, endometrial biopsy in office, abdominal and vaginal hysterectomy, myomectomy, ovarian surgeries and managing the abdominal and perineal hematomas. Respondents’ preparedness for infertility skills is summarized in Figure 3. On average, 70% were skillful, although more than 60% felt they needed more training. The lowest level of preparedness was in laser (14%), following therapeutic (22.1%) and diagnostic laparoscopy (29.1%). Their preferred training methods were practical bedside training in academic hospitals in most skills.
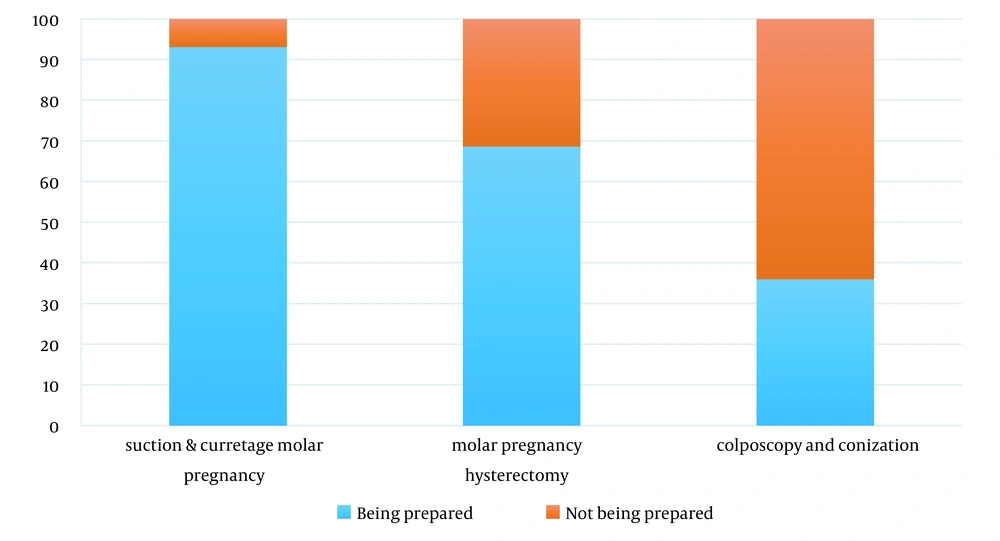
4.6. Oncology Skills
This field evaluated the ability to perform suction and curettage for molar pregnancy, molar pregnancy hysterectomy, colposcopy, and conization. Respondents’ preparedness for oncology skills is summarized in Figure 4. On average, 65.6% were skillful, although more than 65% needed more training in this area, and the lowest level of preparedness was in colposcopy and conization. Their preferred training methods were practical bedside training in academic hospitals in most skills.
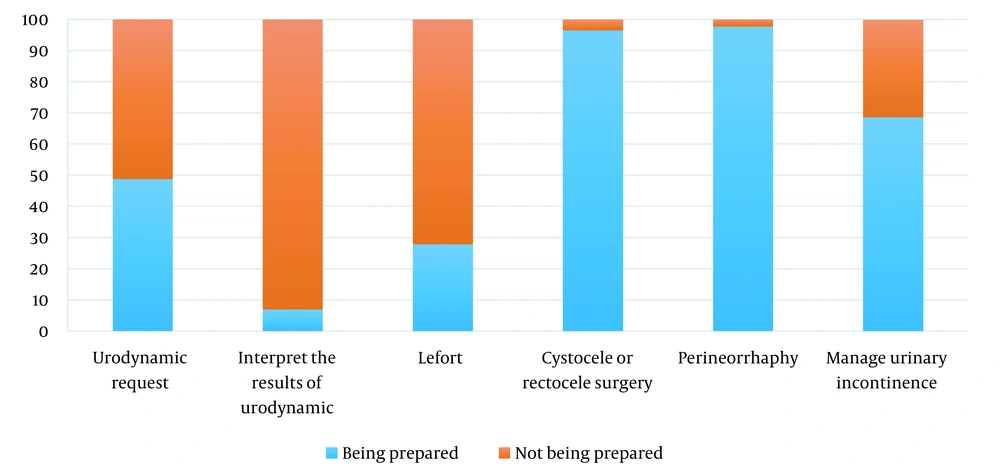
4.7. Urogynecology Skills
In this field, the indication of urodynamic request and interpretation, performing Lefort surgery, cystocele or rectocele surgery, perineorrhaphy, as well as managing urinary incontinence were asked. Respondents’ preparedness for urogynecology skills is summarized in Figure 5. On average, 57.7 % were skillful, although more than 62.5% of the clinicians felt they needed more training in this area, and like other subspecialties, the preferred methods of training were practical bedside training in academic hospitals.
5. Discussion
This study revealed that near to 70% of the participants were able to perform common procedures and management in various fields of obstetrics and gynecology, including obstetrics, general gynecology, infertility, oncology, and urogynecology skills, although more than two-thirds of them felt they needed more training. Physicians’ lowest level of preparedness was in urogynecology skills, while the highest level of educational needs was reported in the field of infertility.
In general skills, approximately 93% of the participants experienced severe stress during the treatment of patients due to potential mortality or morbidity of their patients. Gynecologists and obstetricians are very high-risk specialties for burnout that could be prevented and reduced by implementing needed interventions. Although, there are not enough studies on long-term outcomes and structural strategies to manage (14). Indeed, most of the physicians had insufficient proficiency in legal challenges and proper documentation related to their field. It is reported that 76% of gynecologists and obstetricians have been sued at least once, and these doctors have one of the highest malpractice insurance rates of any medical profession. Obstetrics litigation can be prevented by learning medical laws and guidelines related to their practice, ensuring adequate communication with patients, and proper documentation (15).
One of the questions we asked in the questionnaire was the preference of clinicians to conduct CME courses. It was noteworthy that in most cases, specialists preferred to have bedside training in academic centers to learn the procedures scientifically and correctly from the instructors. Traditional continuing medical education based on lecture only have little chance of impacting clinical practice (16). These courses are preferred to be interactive case discussions allowing individuals to practice new learnings and skills (17). Even experienced physicians tend to receive practical training from mentors in any field after graduation, just like during their residency. Most CME program evaluations focus on topic relevance and speaker quality. Other programs include pre-and post-tests to assess. However, the main goal of CME planners is improving clinicians’ practice (18), and we believe this goal could be achieved via bedside teaching.
In this study, we tried to have a more comprehensive view than previous studies in this field (19). The strength of this study is its specification. Despite limited previous studies (20), we asked for more skills to provide specific CME programs based on a needs assessment for gynecologists and obstetricians. Therefore, according to the study, we suggest CME courses would be conducted as bedside training in the clinics or operating room of academic centers.
5.1. Conclusions
Despite the mastery of gynecologists and obstetricians are skillful, most of them needed more training, and in most cases, their chosen method was face-to-face and bedside training in academic centers. Therefore, specialized planning based on this clinical capability assessment in different fields of obstetrics and gynecology and holding practical and theoretical CME courses seems necessary.