1. Background
Pregnancy is one of the natural events in every woman's reproductive age, and prenatal care can reduce the possibility of death and problems caused by pregnancy and childbirth by identifying and reducing potential risks during pregnancy and helping women to correct the factors. Reduce behavior that leads to adverse pregnancy outcomes (1, 2). Insufficient care of a pregnant woman during pregnancy, in addition to causing health problems for the pregnant woman, can lead to adverse consequences for the baby, such as miscarriage, stillbirth, premature birth, low birth weight baby, and many other problems. This can cause the family to spend a lot of medical expenses, which may affect their childhood health; to give birth to a healthy baby, women need a wide range of care to ensure their and their children's health. These cares start from the woman herself, her family, and her home, in other words, from the pregnant woman's self-care (3, 4).
Many changes occur in pregnant women during pregnancy, including anatomical changes (increase in the volume of the uterus) and physiological changes (changes in the release of body hormones). These changes in the pregnant woman's body cause a change in the person's physical state and decrease the ability to bear weight and heavy loads and increase muscle and skeletal pain (5, 6). On the other hand, immobility during this period brings many problems, including back pain, constipation, excess weight, edema, problems caused by pelvic floor muscle relaxation, and psychological problems. The most important physiological changes during pregnancy that cause these pains include (1) creation and increase of interstitial edema; (2) loosening of ligaments due to increased release of relaxin and estrogen hormones; (3) about 20% weight gain; (4) lordosis increases in the lower back due to biomechanical changes (7, 8).
Mobility of the joints may be involved in changing the mother's position, and this change may also cause discomfort in the lower back. This condition is especially problematic at the end of pregnancy, and at this time, burning pain, tingling, and weakness in the upper limbs also occur. This finding may be due to severe lordosis with anterior flexion of the neck and sudden descent of the shoulder girdle. Progressive lordosis is one of the characteristic features of normal pregnancy. To compensate for the anterior position of the growing uterus due to lordosis, the body's center of gravity is diverted to the back and lower limbs (9). Another problem during pregnancy is back pain, one condition that makes women prone to back pain. For many pregnant women, back pain is considered a natural process during pregnancy, which resolves itself after the end of the period. However, studies show that this condition should be considered a serious issue. For some women, back pain during pregnancy begins a chronic pain process that can lead to significant disorders and disabilities (10, 11). On the other hand, some studies indicate that exercise can be used as a prophylaxis method to reduce back pain in pregnant mothers (12, 13). The results of studies on the effect of exercise during pregnancy have been different. Despite the uncertainties, most scientific sources related to prenatal care have recommended teaching the correct principles of exercise and physical activity (14, 15). Because pregnancy is a new experience for most mothers, they should be made more aware of their body postures. The body's position is the way of standing, sitting, sleeping, changing from one position to another, such as standing up, rolling over in bed, and other movements. The correct position of a pregnant mother is necessary for her health and well-being (16).
Because these changes happen to many people during pregnancy, and on the other hand, a pregnant woman cannot visit a doctor or a midwife frequently. Therefore, more attention should be paid to self-care activities that include different aspects, such as physiological, social, emotional, and spiritual. Self-care is an active and practical process that the individual guides and is necessary to prevent short-term and long-term complications (17). Self-care during pregnancy consists of care principles and programs to provide conditions that lead to favorable clinical outcomes (18). According to the definition, self-care is conscious, learned, and purposeful actions and activities to preserve life and improve the health of himself and his family. As a result, self-care activities during pregnancy, which are consciously adopted by the pregnant woman, can lead to maintaining the health of her and the fetus during pregnancy, during delivery, and after delivery. Pregnant women need information, skills, and social support for self-care during pregnancy to be effective. Pregnant women, especially young women, must be empowered to care for themselves during pregnancy to ensure their health and their babies (19, 20). If pregnant women consider themselves vulnerable and sensitive to the adverse outcomes of pregnancy, believe that self-care activities can be useful in reducing these adverse outcomes, and believe that the benefits of adopting these activities are greater than the costs or barriers to doing them, they will probably adopt these behaviors. As a result, the measurement of these constructs can predict performing self-care behaviors during pregnancy.
2. Objectives
This study aims to investigate the effectiveness of self-care training in improving the physical health status of pregnant women.
3. Methods
This semi-experimental study with two control and intervention groups with pre-test and post-test stages on pregnant mothers referred to the health centers of Sabzevar University of Medical Sciences in a simple random fashion based on permutation blocks based on a similar study (21) and considering Taking the confidence level of 95% and the test power of 90%, and using the following formula; the sample size was calculated to be 104 people. Considering the possibility of dropping out, the sample size was 116 people
where in: 1-β = 0.90, 1-α = 0.95, Z1-α/2 = 1.96, Z1-β = 1.28, σ1 = 8.56, σ2 = 7.17, d = 5.
Fifty-eight people were considered for the control group and 58 people for the intervention group. The criteria for entering the study are 20 - 24 weeks gestational age, non-pathological back, chest, and back pain, the maximum number of pregnancies 2 times, age between 18 and 35 years and singleton pregnancy, no underlying disease or fetal abnormality, no Uterine bleeding, no history of orthopedic diseases, back pain, pathological chest, and back pain before and during pregnancy, no history of accidents that caused skeletal-muscular problems, no history of congenital skeletal-muscular problems, having minimal literacy, not losing one's job or spouse during pregnancy, the absence of death of relatives, and the criteria for withdrawing from the study: Refusal to participate in educational programs, the occurrence of disease (blood pressure, diabetes, etc.) and known complications of pregnancy (polyhydramnios, oligohydramnios, known fetal abnormality, intrauterine death of the fetus, etc.) abnormal bleedings included placenta previa, dekalman, death of relatives, loss of spouse's job. In order to carry out work and training more effectively and based on the working group rules, the intervention group people were divided into groups of 8 to 12 people for training. To collect data from two demographic questionnaires including information (age, weight, height, education, occupation, employment history, employment status, gestational age, number of deliveries, age of the last child at delivery, type of delivery method, type of anesthesia, performed exercise and exercise time), and the body map questionnaire, which plays a role in recognizing body areas involved in musculoskeletal disorders, and it is one of the most reliable questionnaires in the field of ergonomics and has a favorable application in ergonomic evaluations. Its validity and reliability have also been calculated (22). Then, in the intervention group, three 1-hour training sessions were conducted. The first session started with welcoming and introducing the members. Then, the people were asked to perform daily and repetitive activities, and their activities (such as sitting, standing, lifting, picking up objects, clothing, and type of shoes) were evaluated by the senior ergonomic design colleague without the people's knowledge. The questionnaire was completed, and the training was multimedia using PowerPoint, practical demonstration, group discussion, pamphlets, and educational CDs. Thus, in the first session, educational materials, including physiological and anatomical changes during pregnancy and common complaints during pregnancy, were explained using PowerPoint and group discussion. In the second session, the contents of the previous session were first reviewed, and the correct postures, including how to get up from the floor, standing for long periods and washing dishes, ironing, sitting on the floor, sitting in a chair, sleeping, fastening the seat belt in the car, wearing clothes and shoes. Carrying heavy equipment with a slide was also taught practically by the researcher. People were asked to implement these situations in a practical way. Each person individually performed all the situations under the supervision of the researcher and the assistant of the researcher to ensure the accuracy of their performance; correct pregnancy breathing techniques were also taught in a simple way, including deep, chest, abdominal, and conscious breathing, calm and regulated breathing, and patterned breathing. In the end, illustrated pamphlets were given to the members for more practice at home. In the third session, the previous materials were reviewed. People are asked to repeat the correct activities. In this session, strength and stretching techniques were taught, followed by correct pregnancy breathing techniques and their combination with movements and activities. Finally, the questions were answered. Since continuous attendance is difficult for the group, and to strengthen self-care, people are given training CDs and exercises are continued at home, and follow-ups are done in the center's care for the correct performance of activities. Also, weekly counseling and follow-up on the use of pieces of training and clarification of ambiguities were done over the phone, and if a repeat visit was needed, the researcher made an appointment with the pregnant woman in the care center and answered the questions. After dividing into groups, the control group completed the questionnaire and received the center's routine care; in the 36th week, the questionnaires were completed again in 2 groups. Other questions required after delivery were completed from the file. After collecting the data, the information was entered into SPSS 18 software and analyzed using descriptive statistics, independent t-test, paired samples t-test, and ANOVA.
4. Results
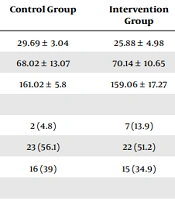
In this study, the results showed that out of 116 pregnant mothers participating in the study, 58 were in the intervention group, and 58 were in the control group, and the average age, weight, and height of the participants in both groups were similar. Most of the mothers in both groups had 9 - 13 years of education, and most of them were employed. There was a significant relationship between the variable of physical health and the variable of age (P = 0.001) and occupation (P = 0.003), and there was no significant relationship with the variables of weight (P = 0.899), height (P = 0.521), education (P = 0.622), and employment time (P = 0.536) (Table 1).
| Variables | Control Group | Intervention Group | P-Value |
|---|---|---|---|
| Age | 29.69 ± 3.04 | 25.88 ± 4.98 | 0.001 |
| Weight | 68.02 ± 13.07 | 70.14 ± 10.65 | 0.899 |
| Height | 161.02 ± 5.8 | 159.06 ± 17.27 | 0.521 |
| Education by year | 0.622 | ||
| 1 - 8 | 2 (4.8) | 7 (13.9) | |
| 9 - 13 | 23 (56.1) | 22 (51.2) | |
| 13 and up | 16 (39) | 15 (34.9) | |
| Job | 0.003 | ||
| Housewife | 44 (89.8) | 42 (79.2) | |
| Employed | 5 (10.2) | 11 (20.8) | |
| Employment time (y) | 5 (100) | 10 (100) | 0.536 |
Abbreviation: SD, standard deviation.
a Values are expressed as mean ± SD or No. (%).
There was a significant relationship between the variables of job status (P = 0.042), gestational age (P = 0.001), number of deliveries (P = 0.001), exercise (P = 0.002), and exercise time (P = 0.003) with physical health. There was no significant relationship between the age of the last child (P = 0.495), type of delivery method (P = 0.163), and type of anesthesia (P = 0.589) with physical health (Table 2).
| Subgroup | Control Group | Intervention Group | P-Value |
|---|---|---|---|
| Status in the job | 0.042 | ||
| Walking | 2 (28.6) | 0 (0) | |
| Carrying things | 0 (0) | 0 (0) | |
| Long-standing | 2 (28.6) | 2 (16.7) | |
| Long sitting | 2 (28.6) | 7 (58.3) | |
| Other cases | 1 (14.3) | 3 (25) | |
| Gestational age | 29.69 ± 3.04 | 25.88 ± 4.98 | 0.001 |
| Number of births | 0.001 | ||
| 1 | 12 (47.1) | 25 (86.2) | |
| 2 | 9 (42.9) | 4 (13.8) | |
| Age of the last child | 6.5 ± 3.14 | 5.6 ± 2.64 | 0.495 |
| Type of procedure, childbirth | 0.163 | ||
| Natural | 12 (80) | 19 (70.4) | |
| Cesarean | 3 (20) | 8 (29.6) | |
| Type of anesthesia | 0.589 | ||
| In public | 2 (66.7) | 4 (57.1) | |
| Epidural | 1 (33.3) | 3 (42.9) | |
| Do you exercise | 0.02 | ||
| Yes | 11 (84.6) | 12 (100) | |
| No | 2 (15.4) | 0 (0) | |
| What time do you exercise? | 0.03 | ||
| Daily | 1 (7.7) | 1 (8.3) | |
| Weekly | 4 (30.8) | 11 (91.7) | |
| Professional | 8 (51.5) | 0 (0) |
Abbreviation: SD, standard deviation.
a Values are expressed as No. (%) or mean ± SD.
And finally, the average physical health in the control group before the intervention was 29.74 ± 6.97 and after the intervention was 28.41 ± 7.44 and in the intervention group before the intervention, it was 30.82±6.38, and after the intervention, it was 27.7±6.33; also, there was a significant relationship between physical health and intervention (P = 0.014) (Table 3).
| Variable | Control Group | Intervention Group | P-Value |
|---|---|---|---|
| Physical health | 0.014 | ||
| Before | 29.74 ± 6.97 | 30.82 ± 6.38 | |
| Next | 28.41 ± 7.44 | 27.7 ± 6.33 |
5. Discussion
One of the challenges of maternal and child health specialists is to provide pregnant women with the correct information and support them during pregnancy with the aim of creating positive changes in their activities. This can effectively lead to the improvement of pregnancy outcomes and empower women to improve their activities and use support resources.
In this study, the results showed a significant relationship between the mother's age, occupation, gestational age, work status, exercise, number of births, and exercise time with the physical health of pregnant mothers. This is consistent with the study of Ghaderi et al. (21), Dorner et al. (23), Ghaffari et al. (24), and Thiese et al. (25). which shows the impact of these variables on the physical health of pregnant women, which should be strictly investigated. For example, the condition of the mother at work and her job plays a very important role in her health because doing activities, standing for a long time, and resting are among the factors affecting the mother's physical health during pregnancy. On the other hand, the variables of doing exercise and the time of exercise, which strengthen her skeletal and muscular system, are important during pregnancy because weight gain and postural-motor changes and analysis of the skeletal system can be predicted during this period. On the other hand, the number of births and the gestational age is also important. It can be investigated due to the mother's physical condition, which increases the possibility of physical problems in her as the pregnancy age increases (21, 26-28).
Also, other results showed that the physical health in the control group was 29.74 ± 6.97 before the intervention and 28.41 ± 7.44 after the intervention, and in the intervention group, it was 30.82 ± 6.38 before the intervention and 27.7 ± 6.33 after the intervention. There was a significant relationship between physical health and the intervention, which shows the effect of this self-care training on the physical health of these women, with the studies of Ghaderi et al. in 2012 under the title of skeletal and muscular pains and factors related to it (21), by Soleiman Ekhtiari et al. in 2015 under the title of self-care in pregnant women (29) and in the study of Mohseni Bandpei et al. in 2010 with the title of examining the effect of exercise on the treatment of back pain during pregnancy (30) and in the study of Heidarzadeh et al. (31) in 2010 was consistent with the title The effect of physical exercise on physical and psychological problems . This issue indicates that women have muscular and skeletal problems during pregnancy, but the necessary training during pregnancy, especially the adoption of self-care behaviors, increases and ultimately improves their health during pregnancy. On the other hand, it can be effective even after childbirth, and this self-care can be used as a tool in designing educational programs that can be used at a relatively low cost compared to other programs. But in general, it is necessary for pregnant women to become aware of their body's anatomy and its changes during pregnancy, and this awareness and preventive measures play a very important role in their physical health.
This study is important because self-care programs are an important health tool, and self-care is a very important and practical tool for people's health, and it is one of the tools in formulating health strategies and educational programs. On the other hand, in recent decades, self-care programs have successfully solved many health problems in our country. These successes have made health activists pay attention to these issues in their programs and in creating or promoting healthy behaviors such as AIDS preventive behaviors, patient self-care in patients undergoing coronary artery surgery, breast self-examination, walking and following a diet in patients with type 2 diabetes, not self-medicating, not consuming smoking and many other physical and mental health issues are used.
One of the strengths of this study is the absence of such a study at the university level, and that too on an important issue such as the effectiveness of self-care in the physical health of pregnant women because pregnant mothers suffer from physical problems during and after pregnancy. The limitation of this study was the lack of cooperation and poor cooperation of mothers to hold meetings and, on the other hand, the problem of following them up as much as possible; these problems were solved with the coordination of the authorities, which suggests that in order to improve the conditions of mothers to perform self-care activities, efforts should be made to remove existing obstacles and increase their awareness of the benefits of performing such behaviors. In order to improve the self-care activities of mothers, these programs should also be organized for pregnant mothers free by the personnel of women's community health centers across the country.
5.1. Conclusions
In this study, the results showed that the use of self-care training increases the health of mothers, and on the other hand, implementing such programs improves the health of mothers and babies and ultimately reduces their health costs.