1. Introduction
The COVID-19 pandemic has been a serious public health threat worldwide, putting millions of people at risk in many countries (1). Since pregnant women have weakened immune systems, they may be at higher risk of severe or critical diseases associated with COVID-19 (2). Evidence shows that COVID-19 can impact various human systems, such as the coagulation system, which can be more severe in pregnant women due to physiological and hormonal changes. These effects on the balance of serum coagulation factors can cause severe coagulation disorders and result in a prothrombotic state (3). Here we described a case of massive bleeding after C/S related to coagulopathies induced by COVID-19 infection in a pregnant woman.
2. Case Presentation
A 32-year-old gravida 3 para 2 pregnant woman, at 37 weeks gestation, was referred to Shohada Hospital of Qom, affiliated with Qom University of Medical Sciences, with fever, tachycardia, chills, and myalgia. Her symptoms had started the day before. She had a history of two previous C-sections (the first due to breech presentation and the second a repeat C-section), with no significant medical or drug history or pre-existing risk factors for intra-abdominal hemorrhage.
The patient’s initial vital signs were: T: 37.2ºC, PR: 136 beats/min, RR: 19 breaths/min, BP: 90/60 mmHg, and oxygen saturation at 92%. The COVID-19 polymerase chain reaction (PCR) test was positive. However, a lung CT scan was not performed due to her pregnancy. Ultrasound examination of the pregnancy and the fetus showed normal conditions.
The patient was immediately admitted to the gynecology department, and urgent blood and urine tests were conducted, followed by a pregnancy ultrasound. An infectious disease consultation was requested, and with an initial diagnosis of pneumonia, she was prescribed ceftriaxone at a dose of 2 grams twice a day, Apotel, and vitamin C. One day after admission, the patient began uterine contractions and labor, leading to a C-section. A healthy girl was born with an Apgar score of 9.
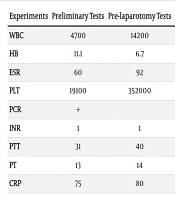
The patient was under close observation. About 30 hours after the C-section, her hemoglobin levels dropped dramatically (Table 1). Before this drop, her vital signs were stable, but she then experienced a decrease in blood pressure (BP: 80/50 mmHg) and an increase in heart rate (PR: 148 beats/min). An emergency ultrasound was performed, revealing abundant free fluid in the abdominal cavity. Consequently, the patient underwent a diagnostic laparotomy. During the laparotomy, two liters of blood with clots were found in the abdomen, but the source of the bleeding was inconclusive. The blood and clots were completely suctioned and removed, and an intra-abdominal drain was placed. Following the laparotomy, the patient was transferred to the ICU.
| Experiments | Preliminary Tests | Pre-laparotomy Tests | Post-laparotomy Tests | Discharge Day Tests |
|---|---|---|---|---|
| WBC | 4700 | 14200 | 14200 | 14200 |
| HB | 11.1 | 6.7 | 8.2 | 11.1 |
| ESR | 60 | 92 | 84 | 53 |
| PLT | 19100 | 352000 | 185000 | 180000 |
| PCR | + | + | ||
| INR | 1 | 1 | 1 | 1 |
| PTT | 31 | 40 | 36 | 35 |
| PT | 13 | 14 | 13 | 13 |
| CRP | 75 | 80 | 52 | 28 |
Summary of Patient Laboratory Research Results
The patient received a total of 2.5 liters of normal saline and lactated Ringer's solution, 6 units of packed cells, 6 units of cryoprecipitated antihemophilic factor, and 6 units of fresh frozen plasma (FFP). Additionally, she was administered Remdesivir. After 5 days, the patient was discharged in good general condition. Follow-up of the patient up to 40 days post-delivery, conducted in person and by phone, indicated the health and well-being of both the mother and her baby, with no signs of COVID-19 involvement in the baby.
3. Discussion
Recently, several studies have highlighted the role of COVID-19 in increasing morbidity and mortality among pregnant women (4, 5). Pregnant women, especially in the third trimester, have a heightened sensitivity to COVID-19 infection and are at risk for severe complications (6). Immune disorders are significant characteristics of patients with severe and critical COVID-19, and pregnant women with the disease often face severe or critical immune responses. In these patients, the coagulation and fibrinolysis systems are disrupted, significantly increasing the risk of bleeding (7). Additionally, SARS-CoV-2 infection during pregnancy can increase the incidence of thrombosis, particularly in patients with certain genetic disorders (8).
Only a few studies have been conducted on COVID-19-associated bleeding during pregnancy and childbirth (9-11). One study reported bleeding in COVID-19-positive patients after normal delivery, while another study reported bleeding in COVID-19 patients with preeclampsia (12).
COVID-19 in pregnant women is likely associated with an increased risk of premature birth, which can cause numerous problems for both the mother and the fetus (13). Inadequate growth of the placenta and fetus during early pregnancy, along with the impact of COVID-19 on the mother's immune system, causes hemodynamic changes in the maternal reproductive system and increases the risk of bleeding, thromboembolism, and other pregnancy complications. The long-term prognosis of COVID-19-infected pregnant women is unclear and requires more detailed investigation (13, 14).
SARS-CoV-2 leads to functional changes in both asymptomatic and symptomatic pregnant women, affecting the fetal-placental unit and neonate. This disease impacts the function of the placenta and fetus, causing a general inflammatory state, coagulation and hemolysis disorders, and more severe infections in pregnant women with COVID-19 (15). Obesity, diabetes mellitus, and high blood pressure may increase the vulnerability of pregnant women to SARS-CoV-2 infection (15, 16).
Probably the most important mechanism of bleeding in pregnant women with COVID-19 is cell necrosis and mucosal damage following long-term hypoxia. These factors can lead to increased bleeding due to vessel wall damage. Additionally, hormonal changes in pregnant women, especially in the third trimester and during delivery, along with the reduction in blood cell coagulation, increase the risk of bleeding in invasive procedures such as surgical incisions and cesarean sections (16-18).
Our study reported severe post-delivery bleeding in a patient infected with COVID-19. This case study highlights that pregnant women with asymptomatic or mildly symptomatic infections can quickly develop severe symptoms and complications during delivery. It should be noted that the administration of two doses of ceftriaxone could not have caused the patient's coagulation disorders, indicating that a more significant factor must have been involved. Furthermore, coagulation disorders can be the first presentation of COVID-19 infection and may even manifest similarly to pregnancy outcomes (3).
COVID-19 infection during pregnancy is associated with widespread systemic inflammation and a so-called cytokine storm. With the increase of acute phase reactants such as C-reactive protein, ferritin, and d-dimer, the risk of bleeding is heightened (19). The cytokine storm occurs more intensely in pregnant women, leading to an increased incidence of premature birth and a tenfold increase in the probability of bleeding. Therefore, bleeding during cesarean sections in COVID-19 patients experiencing a cytokine storm can be highly complicated (19, 20).
Pregnancy itself increases the risk of coagulation. In the third trimester, d-dimer and fibrinogen levels can increase by up to 50%. It is recommended that pregnant women infected with COVID-19 undergo routine lab tests, including measurements of activated partial thromboplastin time (APTT) and fibrinogen, to diagnose and estimate risk (21).
Moreover, due to the possibility of developing coagulopathies, close monitoring of the coagulation system in both the mother and fetus or offspring is necessary (22).
3.1. Conclusions
Accurate and complete recording of the patient's history and tests, early diagnosis of bleeding, and careful monitoring of newly operated patients, especially those with COVID-19, significantly reduce the risk of hemorrhagic shock, maternal complications, and mortality. Therefore, pregnant women positive for COVID-19 should be monitored and treated in maternity hospitals equipped with blood banks and internal surgery services.
3.2. Limitations
The limitations of this study include the lack of D-dimer measurement, the absence of prediction for cytokine storms, and the lack of approximate estimation of the amount of bleeding in the patient's file. It is recommended to ensure sufficient care in recording the D-dimer level, cytokine status, and other coagulation tests in the files of these patients.