1. Background
Labor is the process by which a baby and the placenta are delivered from the uterus. It has four stages, and stage one is divided into the latent phase and the active phase (1). Digital vaginal examination is a well-known method for determining the progress of labor (2). It shows cervical dilation, effacement, and the presenting part, but despite its low accuracy, it is still commonly used to determine labor progression (3). However, studies have found that the actual number of examinations performed is significantly higher than recommended (4). Therefore, a vaginal examination may not be a reliable scale for measuring cervical dilatation, especially when different examiners perform it, as it is operator-dependent (5, 6).
In February 2018, the World Health Organization (WHO) published a consolidated set of recommendations on intrapartum care. In low-risk pregnancies, it is recommended that digital vaginal exams be performed at four-hour intervals (7). Other types of examinations used include assessing the frequency and quality of uterine contractions, fetal descent by abdominal palpation (8), rectal examination (9), and ultrasound (10). Maternal behavioral and physiologic changes are also considered markers of labor progress (11). Repeated vaginal examinations can be unpleasant and stressful for the patient (12). The use of intrapartum ultrasound can reduce the number of digital cervical examinations needed during labor and, consequently, the incidence of intrapartum fever and chorioamnionitis (13).
Another non-invasive way to detect the progress of labor is to assess the length and width of the purple line and fetal head descent in the active stage of labor. The purple line is a red-purple spot that appears around the anus with the progression of cervical dilation in labor (14-16).
There is a limited amount of literature on indicators that predict whether labor will result in a vaginal delivery. Diagnosing abnormal labor progress, despite the existence of many solutions, is still based on the labor trial, considering the painfulness of vaginal examinations (2). This study was designed to investigate an alternative and innovative method for determining the association between cervical dilation and the distance between the fundus and the xiphoid process of the sternum during uterine contraction. It is expected that during contraction, the greater the cervical dilation, the shorter the distance between the uterine fundus and the xiphoid process of the sternum.
2. Objectives
In this study, the aim was to assess the relationship between the distance of the xiphoid to the fundus and cervical dilatation during the latent and active phases.
3. Methods
This cross-sectional study included pregnant women who were referred to the maternity ward of an academic center and provided informed consent. The inclusion criteria were women aged 16 to 40 years of age with a gestational age of 36 to 42 weeks of gestation, vertex presentation, singleton pregnancy, and sonographically estimated fetal weight between 2000 and 4000 grams. The exclusion criteria included patients with systemic disease, unwillingness to cooperate, elective cesarean section, emergency cesarean section, and sonographically estimated fetal weight below 2000 grams or above 4000 grams.
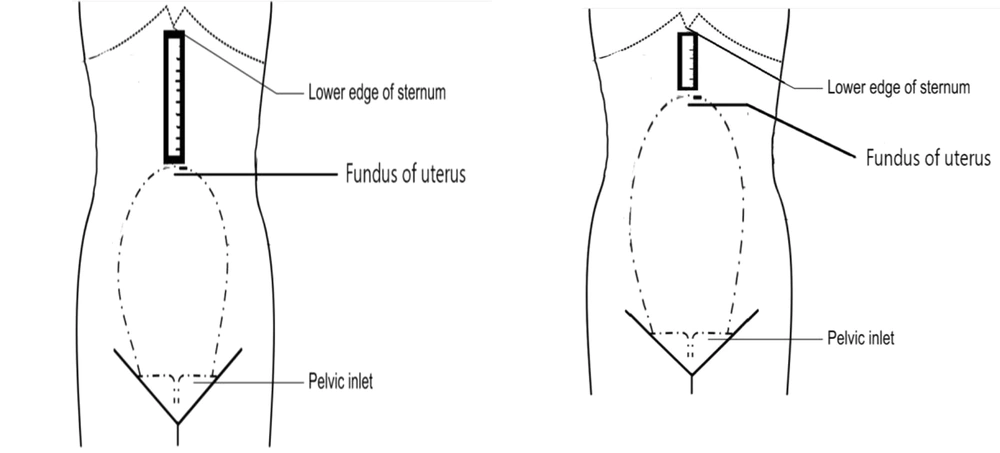
Data were collected through questionnaires from the authors, including age, gestational age, body mass index, parity, history of chronic diseases, history of obstetrical complication, stillbirth, recurrent abortion, and preeclampsia. During contractions, every 3 hours in the latent phase and every 1-2 hours in the active phase, the distance from the fundus of the uterus to the xiphoid process of the sternum was measured in centimeters, the cervical dilation and labor progress was checked and recorded simultaneously. The schematic image (Figure 1) illustrates the method of measuring the fundus of the uterus and the xiphoid process. The collected data, including demographic information, clinical examinations, and the progress of labor, were entered into an electronic case report form (ECRF).
3.1. Statistical Analysis
Data analysis was done using SPSS version 25 statistical software. The mean and standard deviation of quantitative data and qualitative data frequency were calculated. Independent t-tests and Spearman's correlation coefficient with a significance level of less than 0.05 were used.
4. Results
In total, 352 patients aged 16 - 40 participated. Table 1 shows the age and gestational age of mothers (Table 1).
| Variable | Result, No. (%) |
|---|---|
| Age | |
| 16 - 24 | 93 (26.4) |
| 25 - 29 | 145 (41.2) |
| 30 - 34 | 74 (21) |
| 35 - 40 | 40 (11.4) |
| Gestational age | |
| 36 - 37 weeks | 70 (19.9) |
| 37 - 42 weeks | 282 (80.1) |
Table 2 shows dilation according to different distances from the uterine fundus to the xiphoid process.
| Dilation (cm) | Frequency, No. (%) | Mean ± SD Distance from the Xiphoid Process to the Uterine Fundus |
|---|---|---|
| 1 | 14 (3.97) | 7.5 ± 3.02 |
| 2 | 12 (3.40) | 4.66 ± 3.33 |
| 3 | 26 (7.38) | 6.01 ± 2.12 |
| 4 | 26 (7.38) | 5.46 ± 2.13 |
| 4.5 | 6 (1.70) | 2 ± 1.54 |
| 5 | 38 (10.79) | 3.81 ± 1.24 |
| 5.5 | 2 (0.56) | 7.5 ± 0 |
| 6 | 59 (16.76) | 4.47 ± 2.06 |
| 6.5 | 2 (0.56) | 2 ± 0 |
| 7 | 41 (11.64) | 3.81 ± 1.61 |
| 8 | 35 (9.94) | 3.14 ± 0.76 |
| 8.5 | 5 (1.42) | 1.4 ± 0.89 |
| 9 | 50 (14.20) | 2.8 ± 1.14 |
| 10 | 36 (10.22) | 3.44 ± 1.91 |
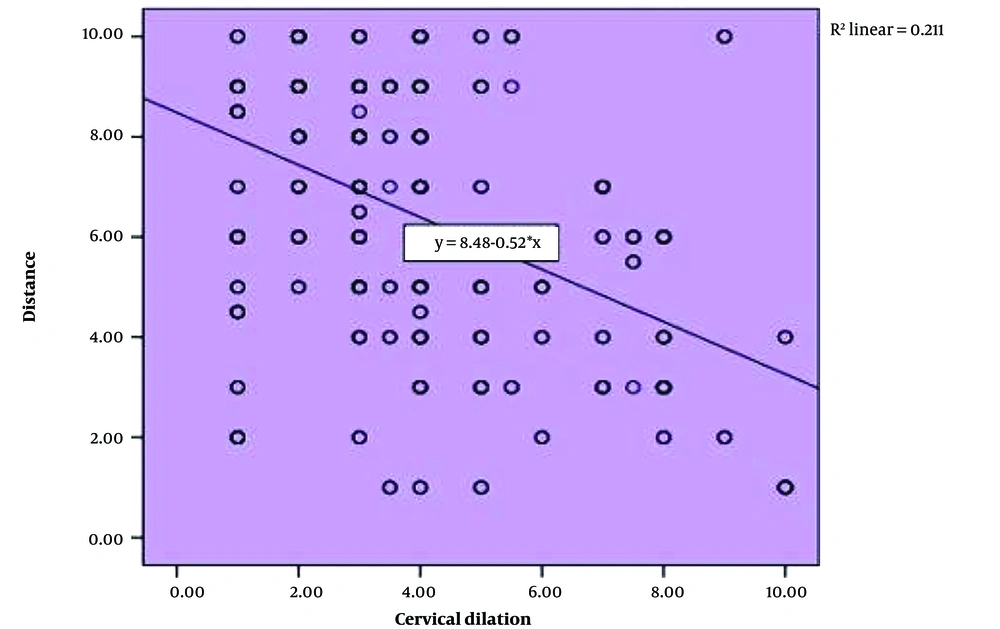
According to Table 2, the calculated Pearson correlation coefficient shows that there is an inverse and significant relationship between the uterus-xiphoid distance and cervical dilation (P<0.01, r = 0.45) (Figure 2).
Table 3 shows the relationship between cervical dilation and the distance between the xiphoid process and the uterine fundus during the active and latent phases of labor. A statistically significant relationship was observed between these two factors in both phases (P = 0.000). The average cervical dilation was higher when the distance between the xiphoid process and the uterine fundus was less than 6 cm (P = 0.001) (Table 3).
| Phase | Cervix Dilation | P-value a |
|---|---|---|
| Latent phase (distance of 1 - 5.5) | 5.09 ± 2.51 | 0.001 |
| Active phase (distance of 6 - 10) | 3.54 ± 1.72 |
a Independent t-test.
| Variable | The Distance of the Xiphoid Process to the Uterine Fundus in Contraction |
|---|---|
| Dilatation | |
| R | - 0.45 |
| P-value a | 0.000 |
| NO. | 352 |
a Pearson correlation test was used for analysis.
5. Discussion
The purpose of this study was to investigate the relationship between the distance between the uterine fundus and the xiphoid process of the sternum during contraction and cervical dilation. According to Table 4, the calculated correlation coefficient shows a significant inverse relationship between the distance between the uterine fundus and the xiphoid process of the sternum and cervical dilation. This means that as the distance between the uterine fundus and the xiphoid process of the sternum decreases during contractions, the size of cervical dilation increases. In other words, as the size of cervical dilation increases, the distance between the uterine fundus and the xiphoid process of the sternum decreases.
With a significance level of 0.95, the hypothesis of the study that the distance between the uterine fundus and the xiphoid process of the sternum during contraction is consistent with cervical dilation is confirmed.
There was a statistically significant correlation between cervical dilation and the distance between the xiphoid process and the uterine fundus during both the active and latent phases of labor. The average cervical dilation was higher when the distance was less than 6 cm (P = 0.001). As shown in Table 3, the highest average dilation was at a distance of one centimeter from the xiphoid process to the uterine fundus during contraction, and the lowest average dilation was at a distance of 8.5 cm from the xiphoid process to the uterine fundus. Rashidi et al. conducted a study on 174 pregnant women, which yielded similar results to ours. The study found a significant negative correlation between the length of the xiphoid to the fundus and cervical dilation, which was consistent with our findings (17).
One of the limitations of this study was the lack of similar studies. According to the limitations of this study, it is suggested that future studies investigate the distance between the uterus fundus and the xiphoid process to confirm the hypothesis of the results of this study and fill this research gap. One of the strengths of the study is the appropriate number of participants in the study, which makes the results reliable. Indeed, the xiphoid fundus measurement can avail as an alternative prediction model in cases that need frequent vaginal examination.
5.1. Conclusions
In conclusion, the distance between the uterine fundus and the xiphoid process of the sternum is related to cervical dilation, and there is a significant inverse relationship between distance and cervical dilation. As the distance between the uterine fundus and the xiphoid process of the sternum decreases during contractions, cervical dilation increases. Therefore, the distance between the xiphoid process and the fundus of the uterus can be utilized as an alternative method for predicting the need for frequent vaginal examinations.