1. Background
Laparoscopy is now the preferred method for most gynecological surgeries. Minimally invasive surgery, including laparoscopic surgery, is widely accepted as an alternative to conventional exploratory laparotomy for managing various benign gynecological conditions (1). Compared to laparotomy, laparoscopy involves less morbidity, pain, and a shorter recovery period. Its advantages include smaller incisions, shorter hospital stays, fewer complications, and faster recovery. These benefits have led to a growing preference for laparoscopy as an alternative to open surgery (1, 2).
During laparoscopy, creating adequate space for the surgical instruments requires inflating the abdomen with gases such as nitrogen, helium, or CO2, each with its own set of advantages and disadvantages (2). Although pain is generally less with laparoscopy compared to open surgery, patients may still experience pain post-operatively. This pain can occur at the surgical site or refer to the shoulder. Shoulder pain typically decreases or resolves when sitting or walking but intensifies when lying down (3, 4). The prevalence of shoulder pain syndrome following laparoscopic surgery in women has not been precisely determined, and understanding of this phenomenon remains limited due to its relatively recent recognition (4).
Residual CO2 gas in the peritoneal cavity can stimulate the phrenic nerve, inflame the peritoneum, and stretch the intra-abdominal cavity, all contributing to shoulder pain (5). The discomfort may be exacerbated by longer operation times and the tightness of abdominal muscles. In women with multiple pregnancies and deliveries, the abdominal muscles are more relaxed and flexible, resulting in milder abdominal and shoulder pain (6).
Postoperative nausea and vomiting (PONV) are common and troublesome complications, with a prevalence reported between 20 - 30% (6-8). Postoperative nausea and vomiting is not always directly related to the type of surgery; patient factors and the anesthetic procedure are significant contributors (6-8). Although PONV is generally self-limiting, it can lead to serious complications such as aspiration of stomach contents, suture dehiscence, esophageal rupture, subcutaneous emphysema, and pneumothorax (8). Additionally, PONV can delay patient discharge (9).
2. Objectives
Given the importance of addressing these issues, this study was conducted at Yas Hospital in Tehran in 2023 to evaluate whether manual abdominal massage maneuvers can reduce post-laparoscopic shoulder pain and nausea.
3. Methods
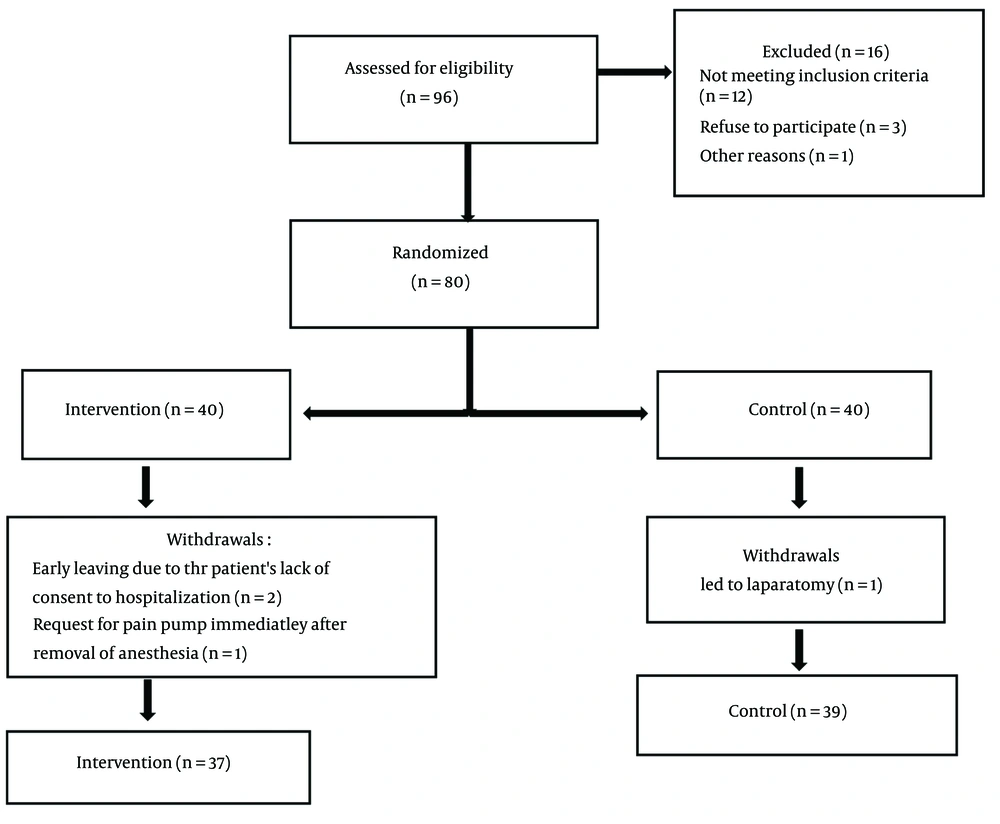
This parallel clinical trial was conducted from January to August 2023 at Yas Hospital in Tehran, Iran. A total of 80 women, selected through simple random sampling, were candidates for gynecological laparoscopic surgery. These participants were randomly divided into two equal groups using an allocation randomization rule. Sampling began on January 30, 2023, and concluded on August 1, 2023, after evaluating and selecting eligible women for the laparoscopic surgery.
Inclusion criteria was women aged 15 to 60 years who were candidates for gynecological laparoscopy and who provided written informed consent to participate in the study.
Exclusion criteria was need for laparotomy surgery; presence of blood or coagulation disorders or concurrent use of anticoagulant drugs; body mass index (BMI) greater than 40 kg/m²; and refusal to participate in the study.
For randomization, sealed envelopes were used. Forty envelopes containing the letter "A" and forty envelopes containing the letter "B" were placed in a bag, and one envelope was randomly selected for each patient. Blinding was not implemented in this study.
In this interventional study, 80 women were randomly assigned to either the intervention group or the control group, with each group consisting of 40 participants. All patients in both groups underwent standard general anesthesia and were placed in the lithotomy position. Each patient underwent the same gynecological laparoscopic procedure. The CO2 gas flow was set to 5 L/min, and the maximum intra-abdominal pressure was maintained at 12 mmHg. The number, size, and location of the trocars were consistent across all patients. The trocars used were: Two 10 mm trocars (umbilical and suprapubic) and two 5 mm lateral trocars.
Ultimately, 76 patients participated in the trial (37 in the intervention group and 39 in the control group). However, three patients from the intervention group and one patient from the control group were excluded from the study for various reasons.
In the intervention group, following the surgery, CO2 gas was evacuated from the abdomen through a two-handed massage applied across the entire diameter of the abdomen, targeting the umbilical and suprapubic trocars, for a duration of 30 seconds.
In the control group, CO2 evacuation was performed traditionally and passively by allowing the gas to exit through the umbilical and suprapubic trocars. The duration of laparoscopy was measured from the moment of skin incision to complete suturing. Pain intensity was assessed 6 and 24 hours after the operation using the Visual Analogue Scale (VAS). The VAS is a 10 cm line with endpoints labeled 0 (“no pain”) and 10 (“pain as bad as it could possibly be”). Patients were asked to mark their current level of pain on the line. Additionally, the consumption of analgesics and anti-nausea drugs was recorded on each patient’s specific sheet. Variables related to the patients included age, BMI, number of previous pregnancies, history of underlying diseases and their treatment, and chronic drug use. The primary outcome variables for this study were shoulder pain and nausea after laparoscopy. The study flow chart is shown in Figure 1.
3.1. Statistical Analysis
All eligible cases who were referred to Yas Hospital Complex in Tehran between January and August 2023 were included in the study after obtaining informed consent. Descriptive statistics, including mean, standard deviation, and relative frequency, were used to describe the data. For data analysis, the exact Pearson chi-square test and Fisher's exact test (for correlation between qualitative variables) and t-test (for correlation between quantitative variables) were employed. All analyses were performed using SPSS version 23 software with a significance level of less than 0.05.
All participants provided verbal consent and cooperated in the research. No additional costs were imposed on the subjects, and their right to withdraw from the study was guaranteed. The study was ethically approved by the Institutional Review Board of Tehran University of Medical Sciences (IR.TUMS.MEDICINE.REC.1400.1308) in accordance with the Declaration of Helsinki. The study was registered with the Iranian Clinical Trials System under code IRCT20201028049169N4, with a prospective registration date of March 28, 2023.
4. Results
Out of the 77 cases investigated, the average age of the women was 39.4 ± 10.1 years, and the average BMI was 27.5 ± 2.5 kg/m2, with no significant difference observed between the two groups. Additionally, there were no significant differences between the groups regarding genital system disorders and underlying diseases. The demographic and clinical history of the women, separated by the two patient groups, are shown in Table 1.
| Variables | Intervention Group (n = 37) | Control Group (n = 39) | P-Value b |
|---|---|---|---|
| Mean women age (y) | 45.1 ± 10.7 | 37.4 ± 9.5 | 0.080 |
| Mean women BMI (kg/m2) | 27.9 ± 2.6 | 27.2 ± 2.4 | 0.158 |
| Genital system disorders | 0.504 | ||
| AUB | 10 (27.1) | 11 (28.2) | |
| Endometriosis | 13 (35.1) | 9 (23.1) | |
| Ovarian cyst | 8 (21.6) | 15 (38.5) | |
| Myoma | 4 (10.8) | 3 (7.7) | |
| Others | 2 (5.4) | 1 (2.6) | |
| Underlying disease | 0.523 | ||
| No | 35 (94.6) | 34 (87.2) | |
| Hypertension | 1 (2.7) | 3 (7.7) | |
| Hypertension/DM | 1 (2.7) | 2 (5.1) | |
| History of surgery | 0.353 | ||
| Yes | 12 (33.3) | 17 (43.6) | |
| No | 25 (66.7) | 22 (56.4) | |
| Average laparoscopy time (min) | 118.1 ± 55.3 | 112.2 ± 58.3 | 0.651 |
Abbreviation: BMI, body mass index.
a Values are expressed as mean ± standard deviation or No. (%).
b The exact Pearson chi-square test and Fisher exact test were used to evaluate the relationship between the group and categorical variables. Independent sample t-test was used to compare the mean of age, body mass index and average laparoscopy time between intervention and control group.
It was observed that, 6 hours after the operation, the pain intensity in the intervention group was 4.6 ± 0.86, compared to 6.2 ± 1.1 in the control group, which was significantly lower in the intervention group (P = 0.001). Similarly, 24 hours after the operation, the pain intensity in the intervention group was 2.7 ± 0.79, whereas in the control group it was 4.2 ± 1.1, with the intervention group experiencing significantly lower pain (P = 0.001). The need for analgesics was also significantly less in the intervention group (P = 0.001). Results related to the final outcomes for the two groups of women are shown in Table 2.
| Variables | Intervention Group (n = 37) | Control Group (n = 39) | P-Value b |
|---|---|---|---|
| VAS | |||
| Average pain intensity 6 hours after the operation | 4.6 ± 0.86 | 6.2 ± 1.1 | 0.001 |
| Average pain intensity 24 hours after the operation | 2.7 ± 0.79 | 4.2 ± 1.1 | 0.001 |
| The average severity of nausea 24 hours after the operation | 2.1 ± 1.1 | 2.5 ± 1.2 | 0.065 |
| Need anti-nausea medication | 0.359 | ||
| Yes | 1 (2.7) | 4 (10.3) | |
| No | 36 (97.3) | 35 (89.7) | |
| Need for analgesics | 0.001 | ||
| Yes | 2 (5.4) | 15 (38.5) | |
| No | 35 (94.6) | 24 (61.5) |
Abbreviation: VAS, visual analogue scale.
a Values are expressed as mean ± standard deviation or No. (%).
b Fisher exact test was used to evaluate the relationship between the group and categorical variables. Independent sample t-test was used to compare the mean of pain intensity between intervention and control group.
5. Discussion
The current study's findings demonstrated that the intervention group's pain intensity was significantly lower than that of the control group at both 6 and 24 hours after laparoscopic surgery (P = 0.001). Additionally, patients in the intervention group, who received manual maneuvers, required analgesics at a considerably lower rate compared to those who did not receive any maneuvers (P = 0.001). However, there was no substantial difference between the two groups in terms of nausea intensity. These results are consistent with the research conducted by Rasooli et al. (9) and Verma and Parashar (10).
The advancement of minimally invasive techniques for surgical intervention, used for diagnostic and therapeutic purposes, has led to a significant shift away from open surgery for the management of various diseases. Despite the advantages of minimally invasive surgery, up to 80% of patients still experience significant pain following the procedure, necessitating strong analgesics for pain relief. Pain characteristics can vary between minimally invasive surgeries, such as laparoscopic procedures, and open surgeries (11). Notably, upper abdominal pain and shoulder pain syndrome are common issues. Effective management and control of shoulder pain are crucial for women undergoing gynecological laparoscopy (11, 12).
The current research showed that manual abdominal massage maneuvers significantly reduced shoulder pain both immediately after the operation and 24 hours later. Bataineh et al. studied 104 women undergoing laparoscopy and found that mild hyperventilation during the procedure, which reduces the amount of air pumped into the abdomen, can greatly lessen shoulder discomfort. This result aligns with the findings of the current study (13).
In Kiyak et al.'s research, it was found that positioning the head at a higher elevation during laparoscopy (semi-Fowler's position) can significantly reduce shoulder pain after the procedure. Although this method is not directly comparable to our study due to differences in the study design, it supports the idea that effective shoulder pain reduction can be achieved through methods such as gas evacuation from the abdominal cavity (14).
In Yang et al.'s study, it was stated that various methods for evacuating gas from the abdominal cavity following laparoscopy in women, such as massage, position changes, or surgical evacuation, can significantly reduce shoulder pain in these patients. This finding is entirely consistent with the results of the present study and highlights the importance of using a standardized amount of CO2 gas during laparoscopy and ensuring the evacuation of residual gas at the end of the procedure (15).
Post-laparoscopic shoulder pain often leads to the use of common painkillers like naproxen and acetaminophen, and occasionally stronger narcotic painkillers may be necessary (1-3). Our study found a significant decrease in the need for analgesics among patients in the intervention group who underwent manual maneuvers, which was anticipated given the reduction in pain intensity following these maneuvers.
Adlan et al. study showed that injecting normal saline into the abdominal cavity during laparoscopy reduces shoulder pain at rest and during movement. This finding aligns well with the results of our study (16).
In a 2012 study, Asgari et al. demonstrated that physical therapy and various laparoscopic techniques for gas removal did not effectively alleviate shoulder discomfort or reduce the need for painkillers. This discrepancy may be attributed to differences in surgery duration, anesthesia type, and the expertise of the gynecological surgeon (17).
Nausea and vomiting after laparoscopic surgery and anesthesia are other common complications that can cause significant discomfort for patients. Various interventions have been tried to reduce these symptoms, with varying results (4, 5). The present study found that manual abdominal gas evacuation following laparoscopy did not significantly affect the severity of postoperative nausea.
Echeverria-Villalobos et al. showed that different manual maneuvers did not reduce the severity of nausea following laparoscopy and recommended using appropriate medications, such as a combination of dexamethasone 8 mg and granisetron 1 mg. While this finding (the lack of effect of abdominal maneuvers on nausea) is somewhat consistent with our study, a direct comparison is not possible since different drugs were not investigated in our research (18).
Samarah et al. examined the impact of manual abdominal decompression techniques on postoperative shoulder pain in patients undergoing laparoscopic cholecystectomy. In this randomized controlled trial involving 60 participants, the intervention group received manual abdominal massage to evacuate CO2 gas, while the control group did not. The results showed a significant reduction in shoulder pain intensity in the intervention group, supporting our research findings and indicating that manual abdominal maneuvers are effective in alleviating shoulder pain following laparoscopic surgeries (19).
Several alternative methods have been proposed for managing shoulder pain following laparoscopic surgery. These approaches emphasize the importance of comprehensive pain management strategies in enhancing patient outcomes after laparoscopic procedures. These methods include:
1. Saline irrigation: Injecting normal saline into the abdominal cavity to dilute and evacuate residual CO2 gas has been shown to reduce shoulder pain and the need for postoperative analgesics (16).
2. Hyperventilation technique: Mild hyperventilation during the procedure to minimize the amount of air introduced into the abdomen has been effective in reducing shoulder pain post-surgery (13).
3. Semi-Fowler's position: Adjusting the patient's head height during laparoscopy, known as the semi-Fowler's position, can significantly alleviate shoulder pain after the operation (14).
4. Pharmacological management: In addition to NSAIDs, combining medications such as dexamethasone and granisetron has shown efficacy in managing postoperative nausea and shoulder pain in some studies (18).
5. Transcutaneous electrical nerve stimulation: Asgari et al. explored the use of transcutaneous electrical nerve stimulation (TENS) in combination with fentanyl for pain management. Transcutaneous electrical nerve stimulation was found to be an effective adjunct in reducing shoulder pain during laparoscopic procedures (17).
5.1. Limitations
One of the key limitations of this research was the involvement of different gynecology and obstetrics surgeons, each with varying techniques and methods. Additionally, some patients' lack of cooperation was another limitation, although efforts were made to minimize this issue through patient education. This study focused solely on laparoscopic surgery for benign gynecological conditions, and further research is needed to explore other methods. Pain assessment could also be influenced by variations in surgery type and duration, indicating a need for refinement in these strategies to enhance clinical efficacy. Moreover, factors such as the retention of intraperitoneal blood, inflammatory cystic fluid, or residual carbon dioxide may have affected our evaluations.
5.2. Conclusions
Finally, the findings of this research demonstrate that manual abdominal massage following women's laparoscopy can significantly reduce shoulder pain, decrease the need for analgesics, and subsequently increase patient satisfaction. Therefore, this method can be considered an effective approach to mitigating complications associated with laparoscopic gynecology.