1. Background
Labor is induced in 20 - 25% of all pregnancies (1, 2), and its prevalence is increasing, particularly in high-income countries (3, 4). Despite the documented advantages of labor induction (1), it presents some potential risks to both the mother and fetus, with the increased cesarean rate being one of the most notable complications (5-7). However, some studies argue that labor induction at term may not result in an increased cesarean rate (8, 9).
Oxytocin is the most common drug used for labor induction or augmentation, with significant variation in oxytocin regimens across different countries and even among hospitals within the same country in Europe. Some European countries have recently released shared guidelines (10, 11). Two main oxytocin protocols are proposed for labor induction: A low-dose regimen, in which the initial oxytocin dose is 0.5 - 2 mU/min, increased by 1 - 2 mU/min every 15 - 40 minutes, and a high-dose regimen, where the initial oxytocin infusion rate is 6 mU/min, increased by 3 - 6 mU/min at 15 - 40-minute intervals. The American College of Obstetrics and Gynecology (ACOG) states that both low and high - dose oxytocin regimens are suitable for labor induction but acknowledges that no specific maximum dose has been established for intrapartum oxytocin infusion (12).
Additionally, guidelines vary in special situations, such as whether oxytocin should be continued once adequate uterine contractions are achieved or when the cervix has dilated to 5 cm or more, and whether adjustments should be made for obese mothers or multiple pregnancies (10-12).
On the other hand, the European Association of Perinatal Medicine, in its guideline on oxytocin for induction and augmentation of labor, states that 5 IU oxytocin should be diluted in 500 mL of 0.9% Normal Saline, and an infusion pump should be used. It recommends that the initial oxytocin should be 2 mU/min, with increments of 2 mU/min at 30 - minute intervals up to a maximum rate of 30 mU/min or until 3 - 4 contractions per 10 minutes are reached or a non - reassuring fetal heart rate tracing is observed. This guideline also strongly recommends that recommendations regarding intrapartum oxytocin use should be regularly revised (10).
Despite the presence of many studies in this area, convincing evidence is still lacking regarding the cumulative oxytocin dose that women receive during labor. The variations in clinical practice should encourage scientists to develop a standard protocol that includes specific considerations for different clinical settings or populations (13). Moreover, studies focusing on the short or long-term effects of intrapartum oxytocin infusion are limited (13-17).
In Iran, the national guideline for providing midwifery and delivery services, in its third edition in 2017, proposed a protocol for labor induction or augmentation. It recommends an initial oxytocin dose of 4 - 8 drops/min of a 1-Liter crystalloid solution containing 10 IU of oxytocin. This dose can be increased by 4 drops/min at 15-minute intervals until a maximum dose of 64 drops/min is reached or whenever 3 strong uterine contractions are achieved in a 10-minute period, whichever comes first (18).
2. Objectives
Due to the aforementioned considerations, we decided to design a study to assess the oxytocin dose received by pregnant women during labor induction and evaluate any potential association between intrapartum oxytocin dose and short-term perinatal outcomes.
3. Methods
3.1. Study Design and Eligibility Criteria
This retrospective cross-sectional study was conducted on one hundred sixty-two term pregnant women, aged 18 - 46 year old, who had been admitted to the labor ward for normal vaginal delivery at two university-affiliated centers: Vali-E-Asr Hospital, Imam Khomeini Hospital Complex, Tehran, Iran, and 22nd Bahman Hospital, Masjed Soleiman, Iran, during 2021 - 2022.
The exclusion criteria were as follows: Non-cephalic presentations, multiple pregnancies, pregnancies conceived via assisted reproductive techniques, vaginal deliveries after cesarean sections, evidence of contracted pelvis or fetal macrosomia (estimated fetal weight of over 4000 grams) as noted by the physician, the presence of adequate uterine contractions defined as 200 - 250 Montevideo contractions throughout the whole labor, physiologic labors, and using oxytocin doses different from the national guideline. As previously mentioned, our national guideline recommends that intravenous oxytocin be initiated at a dose of 2.5 mU/min (4 drops/min of a 1 - liter crystalloid solution containing 10 IU of oxytocin) and increased by 2.5 mU/min every 15 minutes up to a maximum dose of 64 drops/min or until adequate uterine contractions are achieved, whichever comes first. Additionally, medical records lacking the study's main required data and outcomes were also excluded.
3.2. Data Gathering
Detailed obstetric and medical history-related data, including initial cervical dilation, effacement, position, consistency, fetal head station, each patient’s standard Bishop Scores, intrapartum oxytocin dose, and cervical dilation at which spontaneous or artificial amniotomy was performed, were extracted from patients’ medical records. Study outcomes were defined as latent and active phase duration, delivery mode, emergent cesarean indications, occurrence of immediate postpartum hemorrhage, neonatal Apgar scores at the first and fifth minute, and neonatal NICU admission. These outcomes were compared between two main groups: Those who received an intrapartum oxytocin dose of 2.5 - 10 mU/mL and those who received a dose of 10 - 25 mU/mL. Finally, the study outcomes, including delivery mode, postpartum hemorrhage rate, neonatal outcomes (birth weight, gestational age, NICU admission rate, and Apgar scores), were compared.
3.3. Statistical Analysis
SPSS version 23 (IBM, U.S.A.) was used for data analysis. To describe qualitative and quantitative variables, frequencies and mean values (± standard deviations) were expressed. For variables with non-normal distributions, medians (min-max) were reported. Chi-square tests and regression analysis were used to compare qualitative and quantitative variables, respectively. Additionally, multiple logistic regression tests were performed to account for confounding effects. P-values less than 0.05 were considered statistically significant.
3.4. Ethical Considerations
The Ethical Committee of Tehran University of Medical Sciences approved the study (code IR.TUMS.IKHC.REC.1402.387). However, as the study design was based on reviewing medical records, no informed consent was obtained from the patients.
4. Results
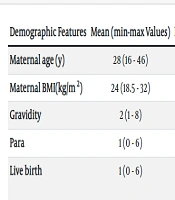
Among 225 included participants, 63 were excluded due to the presence of adequate uterine contractions and no further need for labor augmentation. Participants’ demographic, obstetric, and past medical history data are shown in Table 1.
| Demographic Features | Mean (Min - Max Values) | Past Medical History | No. (%) |
|---|---|---|---|
| Maternal age (y) | 28 (16 - 46) | No comorbidity | 125 (77.2) |
| Maternal BMI(kg/m2) | 24 (18.5 - 32) | Hypothyroidism | 8 (4.9) |
| Gravidity | 2 (1 - 8) | PTL | 7 (4.3) |
| Para | 1 (0 - 6) | GDM | 5 (3.1) |
| Live birth | 1 (0 - 6) | Chronic and/or gestational HTN | 5 (3.1) |
| - | - | Others a | 10 (6.1) |
Abbreviations: BMI, Body Mass Index; PTL, preterm labor; GDM, gestational diabetes Mellitus; HTN, hypertension.
a Two cases of iron deficiency anemia and a case of each of the following comorbidities: Allergy, lower UTI, Minor thalassemia, HBS infection, Asthma, Neurofibromatosis and pyelonephritis.
Sixty-seven women (41.3%) primarily complained of labor pain, 32 (19.8%) reported leakage, 23 (14.1%) had persistent decreased perceived fetal movement, and 26 (16%) were post-term pregnancies. Of the remaining participants, 4 had intrauterine fetal growth retardation, 4 had oligohydramnios, 3 had a diagnosis of preeclampsia, 2 were complicated with intrauterine fetal death, and 1 mother had cholestasis of pregnancy. Additionally, 113 women (69.7%) had maternally uncomplicated pregnancies, while among the complicated cases, gestational diabetes mellitus and hypothyroidism were the most prevalent comorbidities.
Among the study population, membrane rupture occurred spontaneously in 90 cases (55.6%) during labor, in 21 cases (13%) artificial amniotomy was performed, and in 51 women, the amniotic membrane status was not documented. Membranes ruptured at a cervical dilation of 4 cm or less in 65 women (40.1%) and at higher dilations in 46 cases (28.3%).
Regarding Bishop scores, the median score was 6 with a range of 3 - 10. The median (min-max) of cervical dilation and effacement were 3 cm (1 - 7) and 40% (20 - 80%), respectively. No fetal head was at - 1 station or lower, and the most common fetal head station was - 3, seen in 133 cases (82.1%), followed by - 2 in 29 cases (17.9%). The mid and anterior positions of the cervix were the most frequent, observed in 106 cases (65.4%) and 49 cases (30.2%), respectively. Additionally, in 139 cases (85.8%), the cervix was soft, and no cervix was firm on palpation. Cervical ripening agents were used in 43.8% of the population (45 cases of misoprostol and 26 cases of intracervical Foley catheter insertion).
Regarding the indication for oxytocin infusion, 106 women (65.4%) received oxytocin for uterine contraction augmentation, while the rest underwent labor induction. Additionally, in 136 out of 162 cases, oxytocin infusion was continued during labor, as illustrated in Table 2.
| Reasons | No. (%) |
|---|---|
| Fetal decelerations | 14 (53.8) |
| Achieving adequate uterine contractions | 10 (38.4) |
| Fetal tachycardia | 1 (3.8) |
| Suspected placental abruption | 1 (3.8) |
| Total | 26 (100) |
The median oxytocin infusion rate was 10 mU/min (min-max: 2.5 - 25 mU/min), and the median time interval to achieve adequate uterine contractions was 60 minutes (15 - 150 minutes). Additionally, the median (min-max) durations for the latent phase, active phase, and second stage were 9 hours (1.5 - 38), 4 hours (2 - 12), and 35 minutes (10 - 120), respectively.
Regarding neonatal outcomes, the median birth weight (min-max) was 3300 grams (1400 - 4165), and no cases of Apgar scores less than 9 at the 5th minute were observed. However, 22 neonates (13.6%) were admitted to the NICU, 12 of whom were delivered by cesarean section. The majority of these admitted neonates (13.6%) were at a gestational age of 37 weeks. 77.2% of participants delivered vaginally, while 37 cases (22.8%) required an emergent cesarean section. The distribution of cesarean section indications is shown in Table 3.
| Indications | No. (%) |
|---|---|
| Fetal distress | 14 (8.5) |
| Failure to progress | 13 (8) |
| Cord prolapse | 1 (0.6) |
| Second stage arrest | 5 (3) |
| Sever preeclampsia | 3 (1.8) |
| Meconium staining | 1 (0.6) |
| Total | 37 (22.8) |
Regarding early postpartum hemorrhage, 12 cases occurred in those who delivered vaginally and 2 cases in those who delivered via cesarean section. To assess any potential correlation between oxytocin infusion rate and other variables and outcomes, participants were divided into two main groups: Those who received oxytocin at a rate of 2.5 - 10 mU/min and those who received higher doses. The detailed results are shown in Table 4. Generally, fetal head station, cervix consistency, cervical dilation and effacement, cervical dilation at which membranes ruptured, gestational age, rupture of amniotic membranes before oxytocin infusion, and cesarean section rate were all correlated with the oxytocin infusion rate (P-values < 0.001).
| Indications | Oxytocin 2.5 - 10 mu/min | Oxytocin 10 - 25 mu/min | P-Value |
|---|---|---|---|
| Maternal age (y) | 26 (18 - 46) | 29 (16 - 41) | 0.634 |
| Gestational age (week) | 39 (37 - 41) | 40 (39 - 42) | < 0.001 |
| Maternal BMI (kg/m2) | 24 (19 - 32) | 29 (19.5 - 31) | 0.634 |
| Gravidity | 3 (1 - 8) | 2 (1 - 5) | 0.063 |
| Para | 1 (0 - 6) | 1 (0 - 3) | 0.082 |
| Live birth | 1 (0 - 6) | 1 (0 - 3) | 0.111 |
| Abortion | 0 (0 - 6) | 0 | 0.280 |
| Previous preterm delivery | 3 (4.3) | 1 (1.1) | 0.219 |
| Cervical dilation at ROM (cm) | 4 (3 - 6) | 4 (3 - 7) | 0.013 |
| Cervical dilation | 4 (3 - 6) | 2 (2 - 4) | < 0.001 |
| Cervical effacement (%) | 70 (50 - 80) | 40 (20 - 70) | < 0.001 |
| Cervix consistency | < 0.001 | ||
| Soft | 68 (97.1) | 70 (76.9) | |
| Medium | 2 (2.9) | 21 (23.1) | |
| Fetal head station | < 0.001 | ||
| -2 | 26 (37.1) | 3 (3.3) | |
| -3 | 44 (62.9) | 88 (96.7) | |
| position of the cervix | 0.054 | ||
| Posterior | 0 | 7 (7.7) | |
| Mid | 49 (70) | 56 (61.5) | |
| Anterior | 21 (30) | 28930.8) | |
| Bishop Score | 7 (7 - 10) | 5 (4 - 7) | < 0.001 |
| C/S (N) | 6 (8.6) | 30 (33) | < 0.001 |
| Latent phase duration (h) | 7 (1.5 - 24) | 12 (4 - 38) | < 0.001 |
| Active phase duration (h) | 3.5 (2 - 8) | 5 (2.5 - 12) | 0.003 |
Abbreviations: BMI, Body Mass Index; Rom, rupture of membranes; C/S, cesarean section.
a Values are expressed as median (min - max) or No. (%).
Finally, multivariate analysis using binary logistic regression showed that the odds ratio of requiring a higher oxytocin dose is 0.213 (CI: 0.111 - 0.409) for each decrease in the Bishop Score (P-value < 0.001).
5. Discussion
In this study, mothers with higher gestational age, lower Bishop Scores, and amniotic membrane rupture at cervical dilations of less than 4 cm were more likely to need higher oxytocin doses. Additionally, the latent and active phase durations were longer in those requiring oxytocin doses higher than 25 mU/min. However, delivery mode and neonatal outcomes were not correlated with the oxytocin infusion rate. The median oxytocin rate and the time interval to reach adequate uterine contractions were 10 mU/min and 60 minutes, respectively.
In a study by Baranowska et al., the mean oxytocin cumulative dose was 4402 mU in labor inductions and 2366 mU during labor augmentation. They did not find any statistically significant correlation between the cumulative oxytocin doses, delivery mode, immediate postpartum hemorrhage, or neonatal Apgar scores (14). Considering the median labor duration and oxytocin infusion rate, it seems that the assumed cumulative oxytocin dose was higher among our population, aligning with another study that reported higher cumulative oxytocin doses in labor induction (19).
Regarding oxytocin use and perinatal outcomes, Litorp et al. conducted a large-scale cohort study in 12 public hospitals in Nepal on 78,931 laboring mothers and concluded that labor augmentation was correlated with a lower CS rate and a lower proportion of neonates with Apgar scores of less than 7 at the 5th minute (20). Although the current study did not find any correlation between oxytocin dose and CS rate or neonatal outcomes, it should be emphasized that no comparison was made with a control group who delivered physiologically.
Ghanbarzadeh et al. conducted a study comparing high - dose versus low - dose oxytocin regimens for labor induction. They found that the first stage of labor was shorter in the high - dose oxytocin group (189.21 ± 61.57 vs. 125.72 ± 38.53 min), concluding that a higher rate of oxytocin infusion could lead to shorter labor duration. Additionally, delivery mode and Apgar scores did not differ between the two groups. However, in contrast to their findings, our study observed longer latent and active phase durations in those receiving higher oxytocin doses. This discrepancy might be explained by the differences in study design; Ghanbarzadeh et al. compared two distinct oxytocin regimens (low dose: Initial dose of 2.5 mU/min; high dose: Initial dose of 6 mU/min), while our study categorized participants based on the median dose of oxytocin within a single protocol. Furthermore, Ghanbarzadeh et al. did not assess potential effects of other variables, such as Bishop scores, cervical dilation at the time of amniotomy, and membrane status on admission, which were considered in our study (21).
Finally, it is emphasized that each midwifery service - providing center should have a protocol for labor induction and augmentation and, more importantly, audit its guidelines. Regarding study limitations, it should be noted that this was a retrospective observational study, and missing data limited the generalizability of the results. Additionally, long-term maternal and neonatal outcomes were not evaluated. Therefore, the authors highly recommend a larger, well-designed study to reach an evidence-based conclusion.
5.1. Conclusions
According to the study findings, the cervical Bishop score and its components, except for cervical position, were correlated with the intrapartum oxytocin dose. In other words, the less favorable the cervix, the higher the likelihood of requiring higher doses of oxytocin and consequently longer labor durations. Additionally, the cesarean rate was higher in those needing oxytocin doses greater than 10 mU/mL; however, short-term neonatal outcomes did not differ.