1. Introduction
In December 2019, a cluster of pneumonia cases, caused by a newly identified coronavirus, occurred in Wuhan, China, which was named COVID-19 by the World Health Organization (WHO) (1). The disease was constantly growing with human-to-human transmission and soon spread to most countries so that the WHO has identified COVID-19 as a public health emergency of international concern (2). The transmission of COVID-19 is primarily through the respiratory tract via droplets and respiratory secretions, as well as direct contact (3). Common clinical manifestations of the disease include fever, cough, fatigue, shortness of breath, sore throat, and headache (4).
According to studies, the complications of COVID-19 include Acute Respiratory Distress Syndrome (ARDS), shock, acute kidney injury, acute cardiac injury, arrhythmia, liver dysfunction, and secondary infection (5, 6). Therefore, patients with underlying diseases such as high blood pressure, respiratory disease, and cardiovascular disease have a higher risk of mortality than other patients; so, they should be given more care (7). In this case study, we report a patient with early signs of headache and myalgia who had thrombocytopenia while other examinations were normal.
2. Case Presentation
A 60-year-old woman with a four-day history of headache, myalgia, and weakness presented to our emergency department. Her body temperature was 37.5°C by a thermal scanner. On admission, she reported no shortness of breath or chest pain. Her blood pressure was 15/6 mmHg, and she had a history of hypertension. On a physical examination, the patient was found to have dry mucous membranes. The remainder of the examination was generally not significant. The laboratory tests showed only thrombocytopenia with a platelet count of 30 × 109 /L.
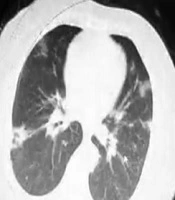
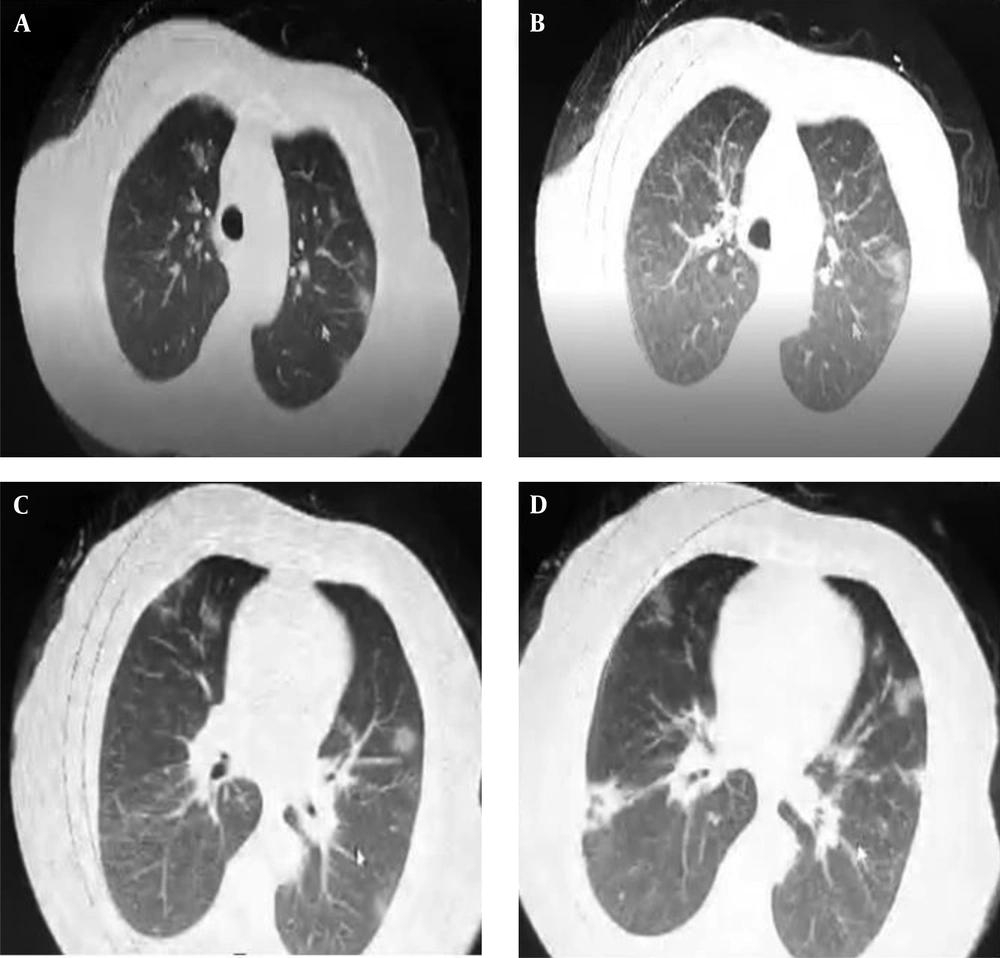
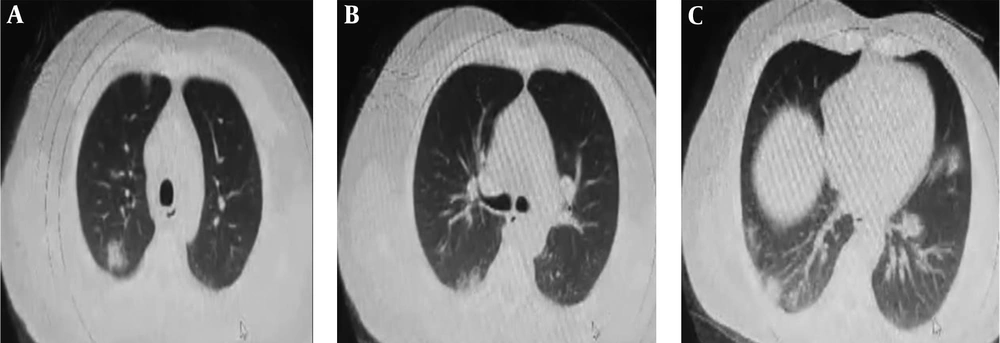
Although early symptoms such as myalgia, fever, weakness, and headache are common to any acute respiratory viral infection, the patient was suspected of having COVID-19 due to the patient’s history of non-compliance with health conditions and contact with others. The patient underwent chest CT and was hospitalized with suspected coronavirus disease. Chest CT showed bilateral ground-glass opacity with no evidence of pleural effusion (Figures 1 and 2). Therefore, she was treated with three drugs (oseltamivir, hydroxychloroquine, and lopinavir), and a nasopharyngeal swab specimen was obtained to send for COVID-19 examination. After three days, the platelet count increased to 70 × 109 /L.
After three days, nasopharyngeal swabs were tested positive for COVID-19 by the real-time Reverse-Transcriptase-Polymerase Chain Reaction (rRT-PCR) assay. Therefore, treatment continued for another six days. On a ninth day, the patient was discharged from the hospital in good general condition and with normal tests to continue the care at home. On the tenth day, on March 26, 2020, she suffered from cardiopulmonary arrest at home and attempted to contact emergency medical services. However, CPR was not successful.
3. Discussion
In this report, the patient presents with headache, weakness, and myalgia, while studies show that the most common clinical symptoms of COVID-19 include fever, cough, and myalgia or fatigue. Indeed, some patients may also present with hemoptysis or headache (4, 8). However, the disease can even be relatively asymptomatic (9). The symptoms of most acute respiratory viral infections are common. Demonstrations of COVID-19 are various and the report cases are increasing; so, the early detection based on imaging findings can be helpful, and ground-glass opacities or consolidations at chest imaging should be considered as possible diagnosis (10).
In this patient, thrombocytopenia was observed, which is a less common, but dangerous, complication of COVID-19. The exact mechanism of reducing platelet counts in patients with COVID-19 is unclear; however, some studies have suggested that coronaviruses can disrupt hematopoiesis by directly affecting the bone marrow or stimulating the immune system against blood cells (11, 12). Some studies have shown that since the lungs are the local site for the release of platelets from mature megakaryocytes, the impairment of the pulmonary capillary bed is a reason for the decrease of platelet counts (12). Patients with COVID-19 can have normal or low platelet counts (1). In Guan’s study, thrombocytopenia was reported in 36.2% of patients with COVID-19, which was significantly observed in patients with high disease severity (4). However, thrombocytopenia has not been substantially found in most COVID-19 studies (13). Studies show that platelet reduction is associated with an increased risk of mortality in patients with COVID-19 and is more frequently seen in patients with higher disease severity; so, it should be recognized as an important clinical indicator during hospitalization (4, 14).
The patient in this study was discharged from the hospital in good general condition and with normal tests, but a day later, she suffered from cardiopulmonary arrest at home. She had a history of hypertension, which is a risk factor for COVID-19. In general, the risk of cardiac arrest occurs in 3% of people with pneumonia, which is related to aging, cardiovascular disease, and the severity of pneumonia (15, 16). This means that patients with cardiovascular disease need more care during and after treatment.
3.1. Conclusion
Because the initial manifestations of COVID-19 are varied and the number of reported cases is increasing, the early diagnosis of the disease based on history, imaging, and rapid isolation of patients who may be at risk of COVID-19 is essential. Patients with cardiovascular disease are at higher risk of COVID-19 infection. Therefore, it is necessary to pay particular attention to cardiac injuries caused by viral infections both during and after the treatment of these patients.