1. Background
Nearly one-third of the world’s population (two billion people) is infected with Mycobacterium tuberculosis and is at risk of developing tuberculosis (TB). Every year, about nine million people get infected with active TB and approximately 1.5 million people die of this disease (1). More than 90% of the infections and deaths arising from TB occur in developing countries and 75% occur in the most economically-active age group (15-54 years old). In such regions, an adult infected with TB misses an average of 3-4 months of work each year, which accounts for a 20-30% loss of annual revenue (2).It is clear that TB, besides economic loss, has indirect negative effects on the quality of life of patients and their families. These include infected women being shunned by their families or expulsion from or dropping out of school of a patient's children. Concurrent infection by HIV and environmental factors can decrease the activity of immune T cells significantly and increase the risk of infection by TB. Countries with a high incidence of HIV, especially in southern Africa, have experienced a dramatic increase in the number of TB patients. The rates of reported patients with TB raised two to three folds over those recorded in the 1990's (2, 3). Genetic variation contributes to the risk of TB and polymorphism of different genes can increase the risk of infection by active TB (4). Macrophages are the primary host cells for proliferation of intracellular mycobacteria. They are responsible for killing internalized bacilli by reacting with nitrogen and oxygen intermediates (ROI, RNI) and lysosomal destructive enzymes (5). The entry of M. tuberculosis into the body induces activation of cellular immune mechanisms which play important roles in the mechanism of T cells. TH1 cells induce macrophage activation and phagocytosis reactions. These cells mediate the acquired immune response against live phagocytic microbes in phagosomes of macrophages. They recognize microbial antigens and activate phagocytes to destroy the ingested microbes. Activated macrophages kill the microbes that exist inside the vesicle most effectively. Microbes that directly enter the cytoplasm (e.g. viruses) or are released from phagosomes into the cytoplasm, however, are relatively resistant. Eradication of these pathogens requires secondary administrative cellular immune mechanisms such as cytolytic T lymphocytes (CTL) (6).CTL-associated antigen 4 (CTLA-4) is a CD28 receptor that inhibits T cell proliferation through combination with B7 molecules (7). The human CTLA-4 gene is located on chromosome 2q33 and the single-nucleotide polymorphism (SNP) +49A/G (rs231775) is located in the first exon of CTLA-4. A +49A/G base substitution can cause a change from threonine to alanine amino acid in the coding region of CTLA-4 (8). The CTLA-4 +6230 (rs3087243) and CTLA4 +49 SNPs have shown strong linkage disequilibrium, which have resulted in excellent combinations for haplotype analysis (9, 10). Previous studies have demonstrated that the +49 SNP of CTLA-4 played a role in the development of Graves’ disease (11), systemic lupus erythematous (12) and other autoimmune diseases. CTLA-4 +6230 SNP is associated with susceptibility to hepatitis B (13) and inflammatory bowel disease (14). Thye et al. (15) found that the CTLA-4 +6230G allele contributed to the pathology of TB in the African population. Reif et al. found an association between genetic changes and extra-pulmonary TB (16).
2. Objectives
The present study investigated a possible correlation between CTLA-4 gene polymorphism and the risk of TB in a sample of the Iranian population.
3. Patients and Methods
3.1. Sample Collection
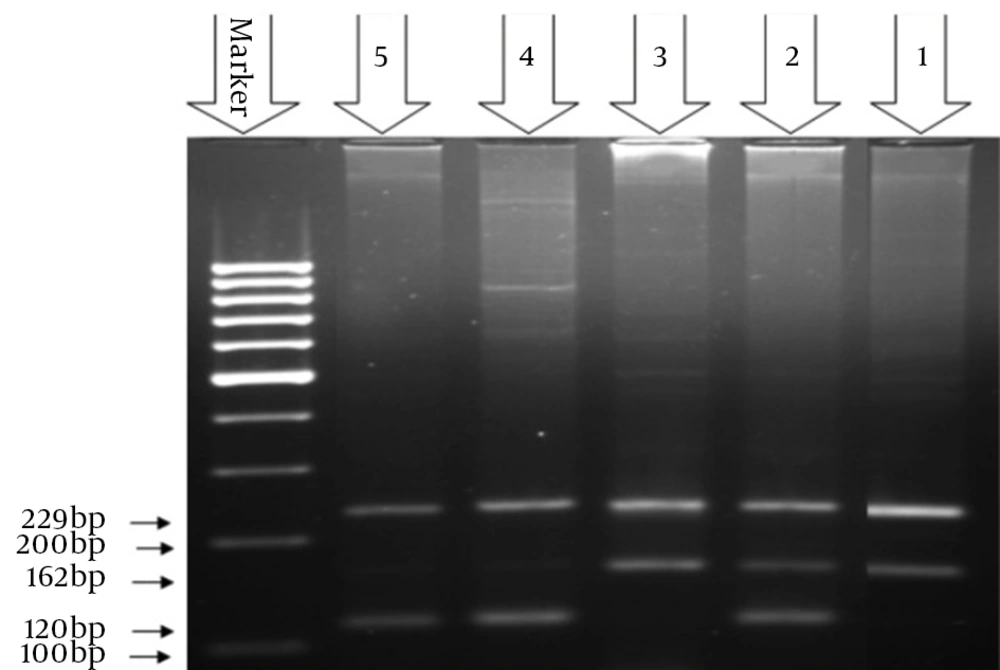
Subjects diagnosed with TB and healthy controls were selected from Chabahar Health Center, Iran. After the subjects signed written informed consent forms, 5 mL of blood was taken from each individual in an EDTA K2 tube. The subjects with TB were selected from those who had had a confirmed diagnosis by a healthcare professional and who presented clinical symptoms, radiological evidence and positive sputum acid-fast bacillus (AFB) smears. The control subjects had no previous history of TB, autoimmune disease, diabetes, or any inflammatory or respiratory disorder. A total of 191 blood samples were collected (106 subjects with TB and 95 healthy controls). DNA extraction was accomplished using an IQ2000 kit according to the manufacturer’s instructions. After estimation of the quality of DNA by spectrophotometer, the tetra-primer amplification refractory mutation system-polymerase chain reaction (ARMS-PCR) method was used to analyze the genotyping of CTLA4 (+49A/G) with the primers given in Table 1. The PCR conditions for the amplification of CTLA-4 were as follows: initial phase comprised 10 minutes at 95°C; next 40 cycles (30 seconds at 94°C, 30 seconds at 62°C, and 30 seconds at 72°C); then, seven minutes at 72°C. The samples were stored at 4°C until electrophoresis.
| Primers | Primer Sequence(5→3) | Length, bp |
|---|---|---|
| Outer primer | ||
| Forward | GTGGGTTCAAACACATTTCAAAGCTTCAGG | 229 |
| Reverse | TCCATCTTCATGCTCCAAAAGTCTCACTC | 229 |
| Inner primer | ||
| Forward, A allele | ACAGGAGAGTGCAGGGCCAGGTCCTAGT | 162 |
| Reverse, G allele | GCACAAGGCTCAGCTGAACCTGGATG | 120 |
Tetra-Primer Amplification Refractory Mutation System-Polymerase Chain Reaction Primer Sequences
3.2. Statistical Analysis
SPSS version 19.0 (SPSS, Chicago) was used for all the statistical analyses. These included categorical data (Pearson’s χ2), adjustment of P values with variables using the binary logistic regression test for estimation of thee odds ratios (OR), 95% confidence intervals, and the relationship between CTLA-4 gene polymorphism and the risk of TB. The significance level was set at P ≤ 0.05 for all the tests.
4. Results
From a total of 100 patients with TB, 68 (35.6%) had positive smears and 15 (7.9%) had negative smears for pulmonary TB. An additional 9 (4.7%) had extra-pulmonary TB and 8 (4.2%) showed recurrent disease after the treatment. The AA genotype +49A/G was found in 42 (42%) subjects with TB as well as in 43 (47.3%) controls subjects. The AG genotype was observed in 38 (38%) subjects with TB and 47 (51.6%) control subjects. The GG genotype was observed in 20 (20%) patients with TB and 1 (1.1%) control subject.
The A allele frequency was 122 (61.4%) in subjects with TB and 133 (73.08%) in control subjects. Allele frequency for the G allele was 78 (38.6%) in subjects with TB and 49 (26.92%) in control subjects (Table 2).
| Genotype | Cases | Controls | OR (95%CI) | P Value |
|---|---|---|---|---|
| AA | 42 (42) | 43 (47.3) | 1.00 | - |
| AG | 38 (38) | 47 (51.6) | 0.83 (0.45-1.51) | 0.645 |
| GG | 20 (20) | 1 (1.1) | 20.48 (2.63-159.60) | 0.0001 |
| AG + GG | 58 (58) | 48 (52.7) | 1.24 (0.69-2.19) | 0.471 |
| Allele | ||||
| C | 122 (61) | 133 (73.1) | 1.00 | - |
| G | 78 (39) | 49 (26.9) | 1.74 (1.13-2.68) | 0.013 |
5. Discussion
World Health Organization statistics has emphasized that in many parts of the world, females are more frequently diagnosed with TB than males and more frequently die from the disease. This disease is a major cause of death by causing infectious diseases in females and primarily affects females in their economically-active reproductive ages (17).The polymorphism in the promoter region of the CTLA-4 gene may play a role in expression of the CTLA-4 receptor in T cells. It can activate this receptor as a regulatory key to suppress the immune response induced, to inhibit transmission to T cells and interaction of these cells with antigen-acceptor cells. The result is the inability of the immune system to form an appropriate response to the pathogen to facilitate the disease progression. Zuh et al. demonstrated a significant association between theCTLA-4 gene polymorphism and the risk of chronic bronchitis (18). Motsinger et al. found a significant correlation between theCTLA-4 gene polymorphism and Graves’ disease. Studies have reported a significant link between theCTLA-4 gene polymorphism and inflammatory bowel disease, ulcerative colitis and Crohn's disease (16). The sparseness of data on the CTLA-4 gene variation and TB allowed only limited comparison of the data with that from previous studies. The data showed a significant link between the GG genotype of CTLA-4 and the increased risk of TB in this sample of the Iranian population.