1. Background
Nosocomial infections are infections that are obtained in hospitals and other healthcare environments. To be listed as a nosocomial disease, the patient must have been admitted for causes different from the infection. He or she needs also have shown no signs of active or incubating infection (1). Hospital-acquired infections have a high prevalence, and the incidence of these infections is different in various healthcare facilities. According to various global statistics, the prevalence of these infections is estimated on average from 5% to 15% in developed countries and up to 25% in developing countries (2). Approximately 2 million people have been involved with this issue and it has remained a large cause of loss of life and money. Extensive use of immunosuppressive medications and broad-spectrum antibiotics has to lead to an increase in people prone to these infections and resistance of the infections to those antibiotics. These infections are difficult to treat and sometimes lead to the death of patients (3). The most important pathogens in nosocomial infections are microorganisms available in the body of patients, which are carried through direct contact between an infected and colonized patient and susceptible health care personnel or another person (4). Common pathogens causing nosocomial infections include (1) bacteria: they are basically from any species, but Enterobacteriaceae (often E. coli) is the most common among them, which live in the intestine. In the case of transfer of bacteria to sterile areas of the body, they can cause infection (5). Staphylococcus aureus lives on the skin surface of 20% of adult individuals and in appropriate circumstances can cause wound or lung infections. Pseudomonas aeruginosa normally lives in the body of 5% of adult individuals and increases in water and moist environments. In the case of consumption of contaminated water, it causes severe and deadly infections in immunosuppressed patients. Staphylococcus epidermidis is present as a part of the normal flora of the skin, and almost all of its infections are hospital-acquired types and are resistant to many antibiotics (6, 7). (2) Viral pathogens: the most common viruses are enteroviruses, influenza, hepatitis B, hepatitis C, and AIDS. (3) fungal pathogens: such as Aspergillus and Candida. (4) Protozoa: such as Pneumocystis carinii and Toxoplasma gondii (6). These microorganisms are transferred in the hospital environment through different ways which include person to person contacts, contact with the body secretions, hospital food and medical equipment as well as the release of aerosol (8). In terms of the prevalence of nosocomial infections in the body organs, the genitourinary system is the most commonly affected, and after that respiratory, circulatory system and the skin are the most vulnerable sites for the nosocomial infections (9). The duration of hospitalization in the intensive care unit (ICU) is directly related to the creation of urinary tract infections. The duration of catheterization, patients with female gender, and time of administration of the first antibiotic are directly related to the prevalence of urinary tract infection. The most common bacteria causing urinary tract infections are Escherichia coli, Candida albicans, and Pseudomonas aeruginosa. Pneumonia, which is reported as the second most common nosocomial infection, has claim to the highest level of mortality. Endotracheal intubation is the most common risk factor for the development of nosocomial Pneumonia (10). Coagulase-negative staphylococci, especially Staphylococcus epidermidis as a pathogen of serious hospital-acquired infections have been isolated in recent years in the neonatal intensive care unit and from the blood cultures of patients with septicemia (which is the third most frequent nosocomial infection) (11). The central Venus catheters cause most of the septicemia, so particularly when the catheter is inserted in the intensive care unit (10, 12), these infections can be prevented, and their rate can be reduced with appropriate measures such as hand washing by staff of health centers, personal hygiene by patients, environmental health control and reduction in indiscriminate use of antibiotics (9).
2. Objectives
This study is aimed to investigate the frequency of nosocomial bacterial infections with multidrug-resistance in hospitalized patients referred to Amir Al-Momenin Hospital, Gerash, Iran, for six months.
3. Methods
This cross-sectional study was handled over six months from the beginning of October 2015 to the end of October 2016 in Amir Al-Momenin Hospital, Gerash, Iran. Nosocomial infection diagnosis criteria were according to the Center for Disease Control and Prevention (CDC) definitions (13). A population containing 300 patients hospitalized in surgical, internal medicine, pediatric, and gynecology wards, as well as ICU, neonatal intensive care unit (NICU). Not including urinary tract infections in this study, based on the case, different specimens including the wound, the eyes, blood, peritoneal fluid, and sputum were prepared by the nurses or the physicians from the investigated population and were sent for investigation to the microbiology laboratory of the hospital. Castaneda and trypticase soy broth (TSB) media were used for blood cultures. Eosin methylene blue agar (EMB), blood agar and chocolate agar were used for wound culture, and blood agar and chocolate agar and Macconkey agar were used for culture of sputum, the eye, and peritoneal fluids. After 24 hours of incubation, some differential tests including, catalase, oxidase, coagulase, indole, sulfide-indole-motility (SIM), triple sugar iron (TSI) media, methyl red/voges proskauer (MR-VP), citrate and urease were used to identify bacteria at the species level. Antibiotics were selected according to isolated bacterial strains, and antibiogram was performed by disc diffusion method on Mueller Hinton agar medium. Also, disc diffusion method is based on the CLSI standard (14). Antibiotics resistance to at least one agent in three or more antimicrobial categories was considered as criteria for multidrug resistance. The obtained data were then recorded in a specific questionnaire for each patient. The information related to hospitalized patients in each ward was extracted separately from the hospital information system.
4. Results
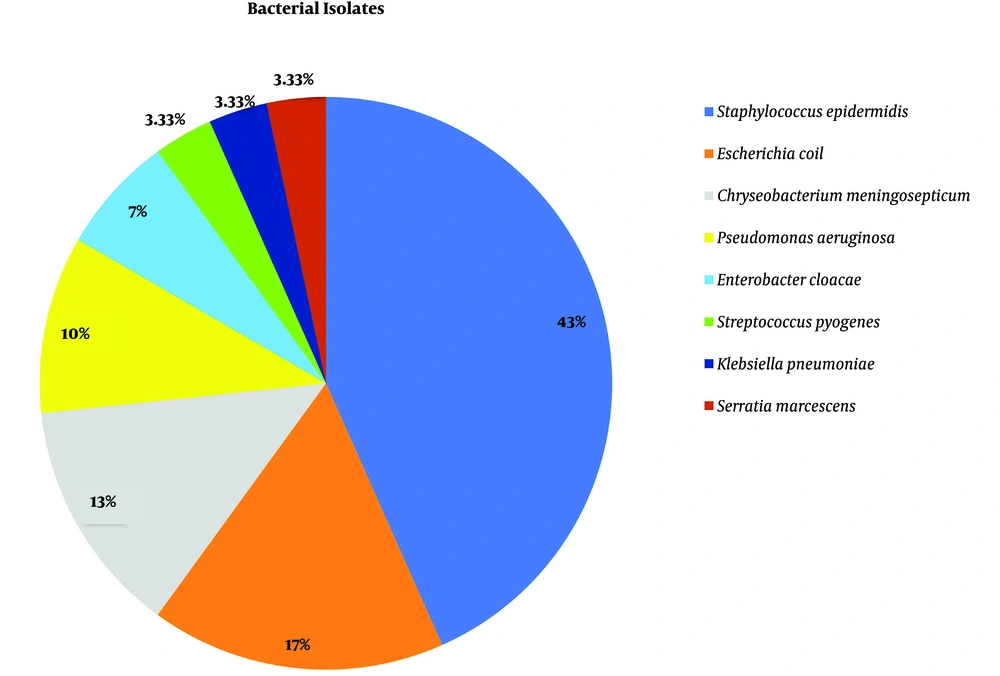
Among 300 patients that were evaluated in this study, 30 patients had been infected with nosocomial bacterial infections, and among them, 18 patients were recognized with nosocomial bacterial infections due to multidrug-resistance. The amount of nosocomial bacterial infections and multidrug-resistance with nosocomial bacterial infections were calculated to be 9.6% and 6%, respectively. In this study, 18 (60%), 6 (20%), 3 (10%) and 3 (10%) cases of nosocomial infections were respectively isolated from the blood, sputum, ocular fluid and wound samples (Table 1). The most frequent bacterial isolate was related to Staphylococcus epidermidis, including 13 cases (43.33%), and then Escherichia coli with 5 cases (16.66%), Chryseobacterium (Flavobacterium) meningosepticum with 4 cases (13.33%), Pseudomonas aeruginosa with 3 cases (10%), Enterobacter cloacae with 2 cases (6.66%), and Streptococcus pyogenes, Klebsiella pneumoniae and Serratia marcescens each with 1 case (totally 10%) (Figure 1). The highest resistance in Staphylococcus epidermidis was first to cefixime (46%) and then sulfamethoxazole (38%). The most resistance in Escherichia coli was at first to cefixime (60%) and then ceftriaxone (40%). Chryseobacterium meningosepticum did not show specific resistance to antibiotics. In general, the highest bacterial resistance to antibiotics used in this study includes cefixime, ampicillin, nalidixic acid, ceftriaxone, sulfamethoxazole, ciprofloxacin, gentamicin, nitrofurantoin, cefotaxime, and vancomycin, respectively.
| Sample Type | No. (%) |
|---|---|
| Blood | 18 (60) |
| Sputum | 6 (20) |
| Wound | 3 (10) |
| Eye | 3 (10) |
| Total | 30 (100) |
Number of Nosocomial Infections Were Respectively Isolated from Different Samples
5. Discussion
The frequency of nosocomial infections with multidrug-resistance, excluding urinary tract infections, was calculated 6% in the investigated health center in this study. The estimated incidence of this kind of disease in studies conducted by different researchers varied roughly between 5% to 10% (11). For example, this amount was reported 3.4% in the study conducted by Qorbanalizadehgan et al. in Baqiyatallah Hospital, Tehran, Iran, in 2005. The result is consonant with the results obtained in the investigation of other researchers. Elderly age group due to changes in cellular and humoral immunity, physiological changes, blood flow disorders and delayed wound healing and newborn babies because of the failure of the immune system are more prone to this type of infection (11). The most significant percentage of nosocomial infections with multidrug-resistance in this study is related to blood infections. In studies performed by other researchers, urinary infections and pneumonia were respectively the first and the second most common nosocomial infections that led to death. Age, gender, occupation, ethnicity, as well as the history of hospitalization, immunological status, and chronic diseases, are the factors that affect this type of infection (15). The prevalence of nosocomial pneumonia was reported 5 to 10 cases per 1000 patients. The incidence of nosocomial pneumonia and wound infection was found to be 10% and 10%, respectively. Nosocomial infections in globally performed researches have mainly been isolated from various types of wounds.
The Staphylococci are a diverse group of bacteria that cause complications ranging from minor skin infections to life-threatening bacteremia. They persist as a principal cause of both hospital and community-acquired diseases worldwide. In the hospital setting, they are responsible for upwards of one million serious infections per year. The two main opportunistic pathogens of this genus, Staphylococcus epidermidis and Staphylococcus aureus, colonize a sizable portion of the human population (16). Staphylococcus epidermidis is a part of the normal flora of the body, which nearly all of its diseases are hospital-acquired types (6). Staphylococcus epidermidis was the most significant cause of blood infections in this study. Unfortunately, about 46% of Staphylococcus epidermidis strains isolated in this research from hospital-acquired diseases were resistant to cefixime. Some researcher noted that these pathogens could produce biofilms that play a significant role in its virulence and pathogenicity and even prevent the penetration of antibiotics at the time of pathogenicity (16, 17).
Various types of bacteria can survive in a hospital environment and have high genetic diversity. Pseudomonas aeruginosa is a gram-negative organism common in nosocomial infections in extensive burns, surgical wounds, as well as in individuals with cancer and people with immune deficiency (18).
Many researchers have studied the prevalence of nosocomial infections worldwide. In a similar study, Baghaei et al. investigated the epidemiological status of nosocomial infections in the Imam Reza Hospital ICU, Urmia, Iran. Their findings showed that the incidence of nosocomial infections was 8.45 percent. The most common types of disease were pneumonia (59.5%) and UTI (21.3%), respectively. Also, the most common microorganisms in pulmonary infections were Pseudomonas aeruginosa, and in UTI E. coli, respectively (19).
Recent data from the U.S. National Healthcare Safety Network indicate that gram-negative bacteria are responsible for more than 30% of hospital-acquired infections, and these bacteria predominate in cases of ventilator-associated pneumonia (47%) and urinary tract infections (45%) (20).
In another study, Behzadnia et al. investigated the nosocomial infections in the pediatric group and antibiotic resistance of the causative organisms in the north of Iran. They showed that the most common type of nosocomial infection (49.18%) was wound disease. Pseudomonas isolates (36.84%) and Acinetobacter isolates (28.02%) were the most common bacteria isolated from the clinical specimens. Also, all the Acinetobacter spp. were multidrug-resistant (21).
Medical equipment used in hospitals plays an essential role in the transmission of infectious agents to patients and the occurrence of hospital-acquired infections (4). Hand washing can be considered as necessary, since it is the easiest and cheapest way to prevent the spread of diseases in ICU. But several factors such as lack of a suitable location for hand washing, inadequate information, poor quality of hand washing liquid, high density of working, lack of knowledge, loss of motivation and willingness of staff, tiredness and so on, have caused this method to be ineffective in some cases.
Training and continued emphasis and providing suitable facilities such as considering a suitable location for hand washing and appropriate hand washing liquid, simple washing with water and soap, using paper towels with adequate quality and paying attention to the desire and demands of staff are recommended. Some necessary measures to control hospital-acquired infections in intensive care unit are policy planning and disinfection and sterilization of equipment and materials in this unit since the risk of transmission of disease to patients always exists following contamination of equipment (22, 23). Disinfection level is also different proportional to the use of equipment. Hospital-acquired infection control recommendations include: (1) activation of hospital infection control committees, (2) establishment of a surveillance system for hospital infection, (3) training of staff and especially nurses of infection control department, (4) emphasis on hand washing, (5) suitable isolation of patients, (6) evaluation of the epidemic cases and performance of necessary interventions, (7) complying with the rules and principles of disinfection and sterilization, and (8) sanitary elimination of the garbage, caring for employees and their immunizations and restriction of the consumption of broad-spectrum antibiotics (23). It is worth noting that, despite employing all measures, the hospital-acquired infections are preventable in only one-third of the cases (24).
5.1. Conclusions
Nosocomial Infections are major infectious disease problems in most hospitals today. However the incidence rate of nosocomial infections in this hospital was low, medical and hygienic interventions such as wearing sterile gloves, hand washing, education on health, continuous supervision, correct use of disposable equipment, controlled use of antibiotics, precise care of surgical wounds and appropriate nutrition are the most important to be considered to reduce nosocomial infections and their adverse effects.