1. Background
Medical Errors (MEs) have been recognized as an inevitable event in the health system that can threaten patient safety (1). A medical error is defined as “an actual or a potential lapse in the care provided to a patient through the performance of a health service or a healthcare professional”. The exact rate of MEs prevalence is difficult to determine because the rate varies from study to study. However, studies report the ME rates in a range of 1 to 4% (2, 3), 6 to 13% (4, 5), and even as high as 51.8% (6). In Iran, based on a systematic review in 2019, the prevalence of MEs was reported as 50% (7). Thus, we can conclude that the MEs rate is higher in Iran than in most developed countries.
Although there has been some improvement in MEs reporting, some studies indicate that the vast majority of errors remain unreported (8, 9). The reported percentages of patient complaints reveal this fact (10). Despite the high prevalence of MEs, in almost half of the cases, they were considered to be preventable. According to investigations, reporting errors in Iranian hospitals is inefficient, and only a small number of errors are reported (11). In addition, nurses, as the significant frontline providers of healthcare services, are involved in MEs that result in patient harm. Nevertheless, like other medical staff, they remain reluctant to report or disclose any MEs (12). Fear of stigma, the effect of errors on the employee’s annual evaluation, and concerns of legal entanglements were recognized as the main barriers to reporting medical errors (13).
Medical error disclosure is recommended by ethical and professional guidelines and legislation (14). Currently, disclosing MEs is advantageous for patients, clinicians, and medical organizations for increasing patient satisfaction and decreasing patient lawsuits (15, 16). However, most health professionals are less inclined to disclose errors to patients (17), while patients are willing to inform about malpractices during medical care in hospitals (18). As a result, 50 to 96% of errors are under-reported to patients (19, 20). A review study reported the lack of a systematic mechanism for identifying, reporting and disclosing errors as one of the major weaknesses and challenges of the health system in the country to reduce similar medical errors in the future, which seriously requires the attention of healthcare policy-makers (11). Indeed, understanding the factors that influence error reporting is a fundamental issue for improving patient safety.
2. Objectives
This research aimed to identify the nurses' perceptions of barriers to error reporting and the nurses' concerns in the disclosure of MEs.
3. Methods
3.1. Design
This study, with an embedded mixed-method approach, was conducted in Iran in December 2018. In this study, quantitative data are the principal data sources, while qualitative data are used to support the quantitative findings based on several scenarios for more clarification.
3.2. Setting and Population
All the 16 hospitals under the supervision of Tehran University of Medical Sciences were included as the target study settings. The target population consisted of nurses who had at least one year of clinical experience (approximately 3,350 nurses). The hospitals were divided into three categories based on the number of beds: Category one (< 200 beds), category two (200 - 500 beds), and category three (> 500 beds) (21). Regarding the number of hospitals in each category, we randomly selected five hospitals. The required sample size was 600 nurses, calculated by Cochran's formula and determined based on a power of 90% (using 95% as the confidence level for confidence interval estimates). A P-value of < 0.05 was considered significant.
Next, for using a two-stage stratified sampling technique, we counted the number of participants in each selected hospital to determine the proportions. After that, we determined the required sample size in each type of ward in each hospital. Finally, the potential respondents were drawn from a complete list of the target population with a simple random sampling technique.
3.3. Data Collection Procedures
A questionnaire was developed based on the literature review. The questionnaire comprised two parts. The first part included seven questions enquiring about demographic information. The second part contained 34 questions in six domains. There were six items about managerial factors, 10 items about the consequences of reporting errors, six items about education, five items about motivation, and seven items about error-reporting mechanisms. The face and content validity of the questionnaire were confirmed considering the experts’ opinions (three nurse experts, four health service management professors, one epidemiologist, and two hospital executive staff). We were requested from the experts to respond to the questionnaire for the assessment of the instrument regarding the clarity, concreteness, centrality, importance, and content validity of each item using a four-point rating scale. Next, we continued the rounds until a 70% agreement was reached. The Content Validity Index (CVI) was used to estimate the content validity quantitatively. The scale CVI for the questionnaire was 0.95. To measure reliability, the questionnaire was distributed to 20 nurses two times at a two-week interval. In both times, the questionnaire was correlated with an 81% confidence. After confirming the reliability and validity of the questionnaire, it was distributed over the hospitals. Of the 600 distributed questionnaires, 491 were returned in a sealed box identifiable in the wards, resulting in a response rate of 81% (Appendix 1 in Supplementary File).
3.4. Ethical Considerations
Informed consent was obtained from participants. The study protocol was approved by the Ethics Committee of Tehran University of Medical Sciences (code: IR.TUMS.REC.1395.273818).
3.5. Qualitative Methods
This phase was designed as a scenario-based experiment and was conducted as a complementary phase to the quantitative counterpart. We sought to understand the nurses’ attitudes toward error definition, error reporting, and their preferences in error disclosure. The interviewers were guided by a script with open-ended questions. Five error scenarios were developed before initiating this phase. All of the interviewees studied and answered the questions (Appendix 2 in Supplementary File). Based on the literature review, the scenarios were prepared and modified by two physicians, two nurses, one quality improvement staff, and a patient safety specialist. In addition, the scenarios were piloted by a physician and a nurse for authenticity and relevance purposes. The scenarios differed in error nature, participants, error consequence, policy procedure protocol, the scope of actions, and team relationships.
We used a purposive sampling technique to identify interviewees from among participates in the previous phase (Appendix 3 in Supplementary File). We conducted 22 semi-structured face-to-face interviews with nurses. After describing the objectives and obtaining consent, information was collected through the scenarios. One of the researchers (ZN), an expert in qualitative interview techniques, conducted all the interviews. Interviews were conducted until they led to data saturation. Each interview lasted 40 minutes on average. Before initiating each interview, the interviewers asked if they had permission to record the conversation. During the interview, no definition of error was provided to the participants. First, participants studied the scenarios, and then the interviewer asked the questions. Interviews were recorded and transcribed verbatim. The transcribed interviews were returned to the interviewees for further checking.
3.6. Data Analysis
The collected data were analyzed both quantitatively and qualitatively. For the quantitative analysis, descriptive statistics, as well as inferential statistics, were operated. As the number of questions in each questionnaire domain varied, we standardized the scores of all domains. Structural equation modeling (SEM) was used to examine the relationship between different domains related to the non-reporting error barriers and compare each domain's effect on the overall score of non-reporting MEs. The significance level was assumed at 0.05 in all analyses. All analyses were carried out via SPSS and AMOS software.
For the qualitative phase, responses were analyzed using content analysis to identify, analyze, and report themes within our data. Coding was done using an inductive approach. Our coding process was developed in multiple stages. First, two of the authors independently carried out the overall readings, identifying aspects relevant to the aim of the study and coding relevant themes, categories, and sub-categories. Meanwhile, in the case of unsolved disagreements, a third researcher (KS) was consulted for a final decision. Next, all researchers reviewed the coded text to identify the concepts and relationships between themes and re-categorized the parameters of each code. In this study, the trustworthiness of the qualitative content analysis was maintained through credibility, dependability, conformability, and transferability (22). In general, the trustworthiness of our findings was enhanced by two investigators coding the raw data to ensure the authenticity of the coding scheme. The final coding scheme was developed by consensus and used for the analysis (Appendix 3 in Supplementary File). Quotes are presented in italic in the results section to bring out major opinions and conformity among the responses.
4. Results
4.1. Quantitative Phase
4.1.1. Demographic Characteristics
Table 1 presents the demographic and professional characteristics of the respondents. Of the participants, 434 (88%) were females, and 218 (44.4%) were married. The mean age of the nurses was 33 (± 7.9) years, and 60% of them had 10 years of experience. Besides, 316 (64%) nurses were working in rotating shifts (Table 1).
| Categories | No. (%) |
|---|---|
| Age | |
| Median (range) | 31 (21 to 57) |
| Mean ± SD | 33.4 ± 7.9 |
| Gender | |
| Female | 434 (88.4) |
| Academic degree | |
| Bachelor | 462 (94.1) |
| Master | 29 (5.9) |
| Nursing shift | |
| Fixed | 175 (35.6) |
| Rotating | 316 (64.4) |
| Marital status | |
| Married | 218 (44.4) |
| Work experience | |
| ≤ 5 | 171 (34.8) |
| 6 - 10 | 163 (33.2) |
| 15 - 11 | 80 (16.3) |
| 16 - 20 | 54 (11.0) |
| 21 ≥ | 23 (4.7) |
4.1.2. Barriers to Reporting Error
Concerning the participants' perceptions, educational factors (57.17%), motivational factors (56.77%), managerial factors (55.31%), error consequences (53.61%), and error reporting mechanism (46.29%) played the most critical roles in non-reporting error behaviors, in sequence. Based on bivariate analysis, statistical results approved a significant correlation between three domains, including error-reporting mechanisms, educational factors, and consequences of reporting errors, and independent variables such as age, sex, and work experience, respectively (P-Value ≤ 0.05) (Appendices 4 and 5 in Supplementary File).
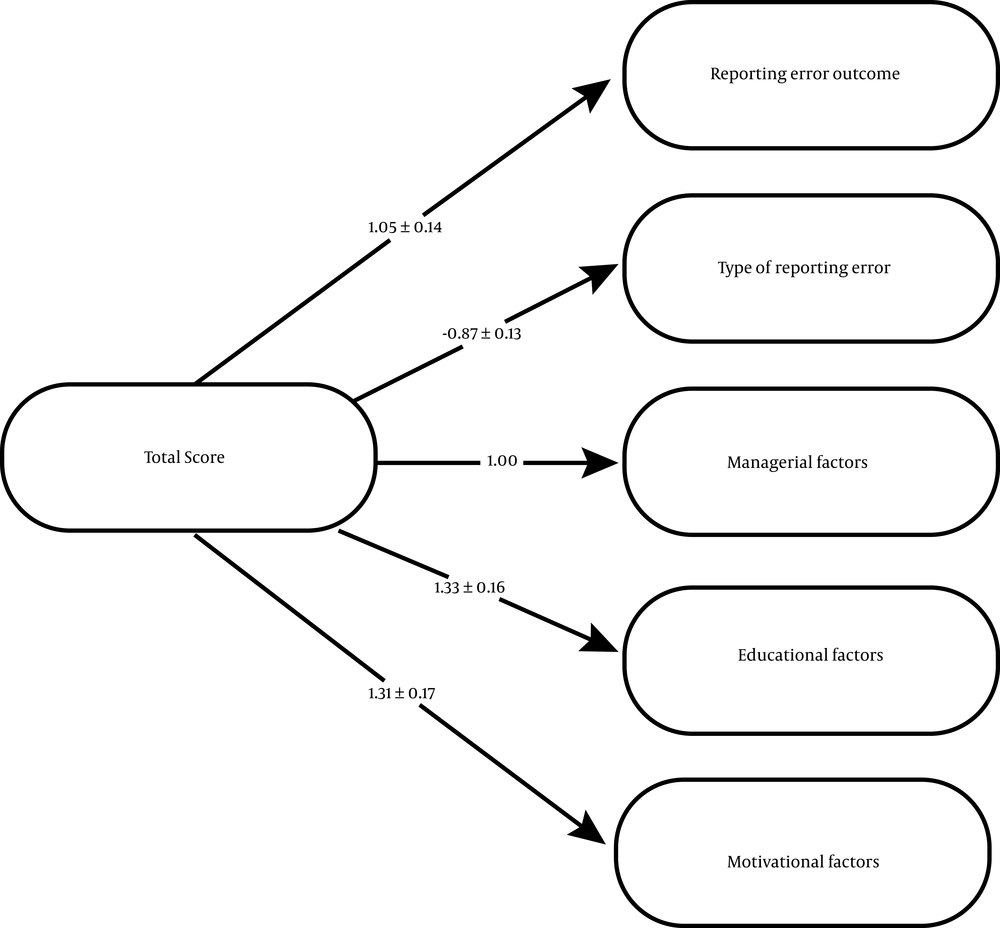
The relationship between the six domains of non-reporting error was examined based on the SEM analysis (Figure 1). The structural model revealed that all paths were of the absolute value of less than z-score (1.96), indicating no significant difference between them. Also, the most important perceived barriers with the highest impacts were educational and motivational domains (Table 2).
| Domains | Estimate | S.E | C.R. | P-Value |
|---|---|---|---|---|
| Managerial factors | 1 | |||
| Error consequences | 1.052 | 0.143 | 7.36 | < 0.05 |
| Educational factors | 1.333 | 0.169 | 7.87 | < 0.05 |
| Motivational factors | 1.310 | 0.176 | 7.44 | < 0.05 |
| Reporting error mechanism | 0.876 | 0.134 | -6.53 | < 0.05 |
a Correlation is significant at the 0.05 level (2-tailed).
4.2. Qualitative Phase
Twenty-two nurses were recruited to the study. All of the participants held a Bachelor of Science degree in nursing. Their average age and work experience were 36 and 10 years, respectively. They were interviewed according to the designed scenarios and responded to the questions revolving around the five scenarios. In addition, they expressed various points about error reporting (Box 1) and disclosing errors in each scenario (Box 2).
| Theme and Reasons for Not Reporting MEs |
|---|
| Error perception (types, causes, and consequences of the error) |
| Ambiguity and weakness in error definition (undefined a near miss as an error, ignoring communication failure); Deviation from standards and the physician’s order |
| The severity of the error and unimportant errors with no injury (less severe errors less likely to be reported or undefined a near miss as an error) |
| Nurses’ unawareness of guidelines, standards, and error management (especially for new staff) |
| Untrained staff (error identification, error type, lack of legal information) |
| Reporting error (formally vs. informally) |
| Ineffective reporting system: Time-consuming, the absence of feedback and communication about the error, without any significant change |
| Hesitation in reporting to the formal system (preference to report the error with no or less harm to the head-nurse instead of someone out of the ward) |
| Believing in reporting the error to be held by the head nurse |
| Increased workload (reporting needs free time, forgetting to make a report that occurs when the ward is busy) |
| The improper reaction of the nurse manager and lack of supportive colleagues (head-nurse) |
| Punitive responses to the error (future negative effects on annual evaluation, promotions, job position, or changing their ward) |
| Concerns about financial loss, legal consequences, and losing job |
| Themes and Reasons for Disclosure |
|---|
| No disclosure |
| Patient distrust toward caregivers |
| The improper reaction of patients or families |
| The error would be without injury |
| Being worried about legal consequences |
| Causing patient anxiety |
| Unawareness of whose responsibility it is and how it should be reported (Not my responsibility) |
| Patient request for discharge without physician decision and stopping the therapeutic process |
| Unsupportive cultures (especially managers) |
| Lack of transparency with explicit instruction and guideline |
| Ruined professional reputation |
| Partial disclosure |
| Building trust to caregivers |
| Improving communication |
| No more details needed |
| Punishment and legal problems |
| Full disclosure |
| Patient right |
| If a serious injury occurs to patients |
| Obvious error occurrence (disclose an error if it is apparent) |
| Having a malpractice insurance |
4.2.1. Error Perception
The nurses' perceptions of the error were directed toward the type and consequences of the error to patients. Of nurses, 55% identified the errors in scenarios (Appendix 6 in Supplementary File). They defined errors as "deviation from the standards, policy procedure, protocols, and physician's order". For example, in Scenario 3, the nurses interpreted errors as "deviation from the implementation of safety standards in blood transfusions such as lack of patient identification and control of vital signs in the first 15 minutes of blood transfusion". Distortion from the protocol in each scenario was also identified as an error by nurses. However, professional and communication skills were ignored in scenarios by most of the participants. A participant responded, "If I understood a problem or harm created by a physician for a patient, I would not prefer to confront the doctor; I will be silent as saving their reputation is very important among others (physicians, managers, nurses, and patients). Professional reputation and others' reactions are critical" (P 4). It seemed error definition was ambiguous; in Scenarios 1 and 2, more than half of the nurses did not detect the errors. Participants identified adverse outcomes in most of the scenarios, but they did not consider them to have the potential for actual harm. Therefore, there is no need to report a near-miss error. When nurses acted beyond their tasks, some of them did not consider it as an error.
Participants emphasized recruiting less-experienced nurses, particularly in high-risk wards such as intensive care and emergency wards, a high number of patients assigned to a nurse, and keeping patients with a critical situation in general wards without meeting the standard nurse-to-patient ratios as the main reasons for not reporting errors. One of the participants expressed, "You are expected to work flawlessly in a bustling environment as we are enforced to take care of intubated patients in general wards instead of the ICU." Generally, while most participants were under time pressure, only a few referred to the lack of time as a barrier. One of the nurses believed, "I think it's the system duty to teach a nurse who is newly introduced into the workplace with less experience. I think weak nursing performance is a sign of weaknesses of nursing education, especially in Continuing Education Centers at hospitals" (P 1).
4.2.2. Reporting Error System (Formal vs. Informal)
A paper-based reporting system was the main error reporting mechanism in the studied hospitals. Sixty-six percent of the participants said they would report the error in scenarios but not precisely through a formal error reporting system in the hospital. Also, they believed they received no feedback when they formally disclosed a mistake (especially an error without harm); this would reinforce the perception that reporting is not essential. In other words, nurses prefer to report the errors informally, such as discussing incidents with their director, other nurses, or physicians in the ward rather than to the hospital incident reporting system. In addition, the nurses strongly believed that there was no need to report erroneous incidents without harm. In general, it seemed the error-reporting mechanism was not an influential factor in not reporting errors. A participant said, “The head-nurse may prefer not to disclose the errors of the ward” (P 2). Error reporting was influenced by participants’ perceptions and the possible consequences. For instance, if a scenario illustrated an error that did not harm patients, the nurses believed that they choose not to report the error. The majority of the participants agreed on concerns of inappropriate reaction and lack of support by the hospital authorities, especially the nursing manager. A nurse stated, “Once I participated in a meeting of morbidity committee for an inadvertent error, I can remember that I was mistreated that I felt insulted as a human being” (P 6). In Scenario 1, a participant commented that he would not report the scenario “Because nothing has happened.” It seemed that error-reporting often varied depending on how much nurses trust others within the team. A nurse said, “Once I reported an error, the nursing manager decreased my annual evaluation score and also my payment. I’ve concluded that there is no need to report an error which wouldn’t cause harm to a patient” (P 4). The majority of the respondents agreed that “nurses’ insufficient familiarization with error documentation,” “fear of the legal liability,” and “concerns for financial losses” are not the reasons for non-reporting error. However, nurses face some workplace penalties such as changing their ward and payroll deductions, which can postpone being qualified as a head-nurse, supervisor, or nursing manager.
4.3. Disclosure of MEs to Patients
While describing the affairs in scenarios, nearly half of the participants did not intend to disclose the MEs to patients (Appendix 6 in Supplementary File). There is a typical disagreement (83%) toward fully disclosing the MEs to patients, especially when there is no severe harm caused to the patient. Although most respondents agreed that this is a patient’s right to know about any errors at the hospital, they tended to conceal errors to prevent any possible consequences after disclosures. Some reasons were missing patient trust, reactions from patients or their families, damage to professional reputation, and the possibility that a patient might sue or reprimand the nurse. On the other hand, some participants agreed with partial disclosure (to describe what had happened without specific details). They believed that providing details could disrupt the relationships between medical professionals and the public, but partial disclosure might improve communication. In general, respondents were not likely to provide full details of errors. For example, one of the participants said, “I committed a medication error, and I told the patient about it; I assured him that it had no side effect and was not risky. However, I was so desperate by the reaction of the patient and his family who asked the head-nurse to change the faulty nurse so that I had to leave my workplace that day, I felt so bad for a while” (P 13).
5. Discussion
Based on our analyses, the most important perceived barriers with the highest impact on not reporting errors coincided with educational, managerial, and motivational factors. Based on our scenarios, 55% of nurses identified the errors, and 66% of the participants pinpointed that they would report the error but not precisely through a formal reporting system. There was a typical disagreement (83%) toward full disclosing to patients.
The primary reason for not reporting errors was weaknesses in nursing training programs. Literature has consistently highlighted it (3, 23, 24). The lack of nurses’ necessary training makes it more difficult to understand the importance of incident reporting. Therefore, it seems that appropriate training about errors (25, 26) and safety requirements (27) is necessary to encourage error reporting. Although with the implementation of accreditation standards in Iranian hospitals from 2010 to the present, the education of health professionals underwent a considerable evolution [9], so that hospitals were obliged to hold annual educational courses and workshops on essential issues, including patient safety and error reporting (28, 29). However, further research is needed to assess the impact of the accreditation program on patient safety and error reporting in Iran.
Our findings are consistent with research results that allude to managerial and motivational factors as the reasons for not reporting errors (30, 31). Managers should not focus on the individuals but rather on the system, reinforcing the importance of complete reporting and providing feedback. What is more, the shortage of nurses and failure to allocate nursing services to patients concerning patients’ conditions inadvertently lead to negligence and defects in such duties (32, 33). Therefore, the reporting process should be simple and not need too much extra work or time, as otherwise, nurses will perceive it as a burden. Garbutt et al. stated that an error reporting system might cause under-reporting incidents due to a lack of feedback and time constraints (34). Finally, managers must create an open, trustworthy, and safe environment in the hospital to promote voluntary, anonymous, and confidential error reporting.
Based on our results, the nurses preferred to report informally when errors occurred within the ward. Also, error reporting was contingent upon the severity of the consequences to the patients; they would not instead report near-miss cases or errors without consequences, even informally. Toren et al. reported a discrepancy between what nurses describe as their intent to report a near-miss event and their actual reporting of an event (35). Nurses fear intimidation, retribution, or punitive measures. However, our results showed some ambiguities existed about error definition, and nurses hesitated to report errors, mainly to formal systems. Nurses perceived that they were blamed or criticized more for committing an error than were physicians. However, in one study published by Mayo Clinic, it was reported that the nurses tend to report the error to physicians (36).
Research has documented that disclosing errors and discussing details with patients are uncommon, and nurses do not intend to disclose fully to patients. O’Connor’s review reveals that healthcare professionals support the disclosure of errors that lead to adverse events, but there is a gap between ideal disclosure practice and reality (37). Other studies report that people firmly acknowledge the need for error disclosure to patients (38, 39), while most health professionals intend not to disclose MEs, especially the detailed information to the patients (40). To attain effective disclosure practices, a systematic training program in the healthcare system is needed to instruct professional ethics and communication skills.
This study encountered a few limitations; For instance, the interviewees' opinions are highly context-dependent, which may reduce the generalizability of the results. Also, we did not assess the patient’s approach toward error disclosing. Nevertheless, we attempted to provide a comprehensive approach by using two methods for more clarification about the accurate reasons to intend not reporting errors and disclosing.
5.1. Conclusions
Barriers to error reporting in hospitals are multifactorial. A lack of knowledge of errors and reporting mechanisms, inappropriate feedback, and adverse reactions are generally the most important inhibitors of error reporting. Such incidents generally occur due to some educational, motivational, and managerial factors. Moreover, nurses still believe that error reporting may bring about more subsequent harms. Combining these factors hinders error reporting and calls for interventions in several areas such as education, socio-cultural values, and managerial support to create a positive attitude, motivation, and incentive to disclose an error. The obtained results urge educational planning and system re-thinking to encourage error reporting.