1. Context
In late December 2019, some mysterious cases of pneumonia with unknown aetiology were reported in Wuhan, China. The contagious virus has caused public health concerns worldwide, and the World Health Organization (WHO) declared the disease a pandemic on March 11, 2020 (1). The coronavirus disease 2019 (COVID-19) is transmitted through droplets, close interaction, aerosols, and the fecal-oral route. Patients in the latent period can transmit the virus to others. According to the literature, the symptoms of this infectious disease include chills, sore throat, dry cough, shortness of breath without or with fever, and severe acute respiratory infection (SARI) (2).
Coronavirus spread from China to other countries, such as Japan, Malaysia, Singapore, Nepal, South Korea, Thailand, Vietnam, Cambodia, Philippines, Russia, UAE, Australia, Canada, USA, and Europe (eg, France, Germany, Italy, UK, Finland, and Sweden (3). The disease is now a global pandemic that has affected more than 200 countries, and as reported by WHO on July 30, 2020, the total number of confirmed cases and deaths from COVID-19 were 16,775,633 and 661,244 people in the world, respectively (4). Various studies have cited hypertension as an essential risk factor for COVID-19-related deaths (5-9). High blood pressure is one of the most common health problems globally and is the cause of half of all chronic diseases worldwide (1, 2). A person is considered to have high blood pressure if the systolic pressure is over 140 mmHg and the diastolic pressure is over 90 mmHg.
High blood pressure annually claims the lives of 9 million people throughout the world. The causes of hypertension are diverse, and it influences 20 to over 50% of adults in developed countries (10, 11). A quarter of men and a fifth of women have hypertension. The factors effective in the occurrence and prevalence of hypertension encompass diet, smoking, genetics, economic status, gender, racial and ethnic differences, as well as some chronic diseases. The prevalence of hypertension varies in distinct parts of the world and is more observed in the lower socio-economic strata (12-14). Several studies have investigated the prevalence of hypertension in patients with COVID-19 worldwide (5-9). Nonetheless, the estimated prevalence rates of hypertension in these patients vary greatly depending on the country in which the studies were performed. Considering the importance of hypertension as a major risk factor for COVID-19-related deaths and contradictory results regarding the prevalence of hypertension in patients with COVID-19, the current meta-analysis and systematic review was conducted to determine the prevalence of hypertension in patients with COVID-19 worldwide.
2. Evidence Acquisition
This meta-analysis and systematic review was performed to estimate hypertension prevalence in patients with COVID-19. This article was written according to PRISMA standards (15).
3. Search Strategy
The articles published during January 2020-July 2020 in PubMed, Scopus, Web of Science, and Embase were reviewed using the keywords hypertension and COVID-19 patients. References to related papers were also reviewed, and if necessary, the authors of some publications were contacted to complete the information. The keywords used for each database were as follow:
3.1. PubMed
("COVID-19"[All Fields] OR "COVID-2019"[All Fields] OR "severe acute respiratory syndrome coronavirus 2"[Supplementary Concept] OR "severe acute respiratory syndrome coronavirus 2"[All Fields] OR "2019-nCoV"[All Fields] OR "SARS-CoV-2"[All Fields] OR "2019nCoV"[All Fields] OR ( ("Wuhan"[All Fields] AND ("coronavirus"[MeSH Terms] OR "coronavirus"[All Fields])) AND (2019/12[PDAT] OR 2020[PDAT]))) OR ("coronavirus"[MeSH Terms] OR "coronavirus"[All Fields] OR "coronaviruses"[All Fields])) OR ("coronavirus"[MeSH Terms] OR "coronavirus"[All Fields] OR "deltacoronavirus"[All Fields])) OR ("coronavirus"[MeSH Terms] OR "coronavirus"[All Fields] OR "deltacoronaviruses"[All Fields])) OR ("coronavirus"[MeSH Terms] OR "coronavirus"[All Fields] OR ("munia"[All Fields] AND "coronavirus"[All Fields] AND "hku13"[All Fields]) OR "munia coronavirus hku13"[All Fields])) OR ("coronavirus"[MeSH Terms] OR "coronavirus"[All Fields] OR ("coronavirus"[All Fields] AND "hku15"[All Fields]) OR "coronavirus hku15"[All Fields])) OR ("coronavirus"[MeSH Terms] OR "coronavirus"[All Fields] OR ("coronavirus"[All Fields] AND "rabbit"[All Fields]) OR "coronavirus, rabbit"[All Fields])) OR ("coronavirus"[MeSH Terms] OR "coronavirus"[All Fields] OR ("rabbit"[All Fields] AND "coronavirus"[All Fields]) OR "rabbit coronavirus"[All Fields])) AND ( ("hypertension"[MeSH Terms] OR "hypertension"[All Fields] OR ("high"[All Fields] AND "blood"[All Fields] AND "pressures"[All Fields]) OR "high blood pressures"[All Fields]) OR ("hypertension"[MeSH Terms] OR "hypertension"[All Fields] OR ("high"[All Fields] AND "blood"[All Fields] AND "pressure"[All Fields]) OR "high blood pressure"[All Fields]))
3.2. Scopus
(TITLE-ABS-KEY (COVID-19) OR TITLE-ABS-KEY (COVID -2019) OR TITLE-ABS-KEY (severe AND acute AND respiratory AND syndrome AND coronavirus 2) OR TITLE-ABS-KEY (2019-ncov) OR TITLE-ABS-KEY (sars-cov-2) OR TITLE-ABS-KEY (coronavirus) OR TITLE-ABS-KEY (coronaviruses) OR TITLE-ABS-KEY (munita AND coronavirus AND hku13) OR TITLE-ABS-KEY (coronavirus AND hku15) AND TITLE-ABS-KEY (high AND blood AND pressure) OR TITLE-ABS-KEY (high AND blood AND pressures))
3.3. Embase
(COVID-19'/exp OR 'coronavirus infection'/exp OR 'coronavirus infection' OR 'coronavirus infections') AND ('hypertension'/exp OR 'htn (hypertension)' OR arterial hypertension' OR 'acute hypertension' OR 'cardiovascular hypertension' 'blood pressure, high' OR 'controlled hypertension' OR 'endocrine hypertension' OR 'high blood pressure' OR 'high renin hypertension' OR 'hypertension' OR 'hypertensive effect' OR 'hypertensive disease' OR 'hypertensive response' OR 'neurogenic hypertension' OR 'preexistent hypertension' OR 'refractory hypertension' OR 'salt hypertension' OR 'salt high blood pressure' OR 'secondary hypertension' OR 'systemic hypertension').
Articles were selected using MeSH, EMTREE, and others in each electronic database. The search was limited to the English language. This study only included the cross-sectional studies that reported the patients with COVID-19, while the case studies, clinical trials, or letters to the editor were excluded. In addition, the primary outcome of the assessed studies was to measure the prevalence of hypertension, and they were evaluated qualitatively.
4. Selection and Screening of Articles
An EndNote library (Variety 8) was created to collect papers, remove duplicates, and analyze headings and summaries. Two researchers reviewed the titles and abstracts of papers, and the differences were resolved through discussion and referring to a third party if needed. The selected references were nominated for full-text review if they contained the favourite facts in the headings or summary reviews. Two authors separately reviewed the full text. Data were extracted from eligible studies and were entered into Microsoft Excel version 2016. In the reviewed articles, a person with a positive polymerase chain reaction test was considered to have COVID-19, and blood pressure above normal (120/80) was regarded as elevated blood pressure.
4.1. Quality Assessment
The Newcastle-Ottawa Scale (NOS) was applied to assess the quality of investigations. This system assigns each question a score of 0 - 1, and the maximum score a study can obtain is nine. Studies with the sum scores ≤ 5, 6 - 7, and 8 - 9 were considered low-, medium-, and high-quality, respectively (16).
5. Data Extraction
In order to obtain the facts, a checklist was initially developed using the opinions of experts on the facts of papers, including author name, year of publication, hypertension prevalence, sample size, country of publication, and population study.
5.1. Bias Risk
Two authors conducted the qualitative assessment of articles according to the NOS that evaluates the quality of observational studies. This checklist is a tool that takes into account three main areas with six different items for each study, including the selection of study groups, comparing groups, and proving the exposure or expected outcome of the study. Checkmarks are placed next to each observed item. The highest possible score is nine, and if there was a disagreement over the score of a published article, the assessors agreed to an arbitrator's decision.
5.2. Analysis
The model of DerSimonian-Laird random-effects was applied to assess the overall prevalence of hypertension (95% CI) using the Metaprop command in Stata 14. The Q and I2 tests Cochrane were utilized to evaluate the variance and heterogeneity of investigations. A funnel plot, Egger test, and graphs were used to evaluate the publication bias. All two-way statistical tests were considered with α = 0.05.
6. Results
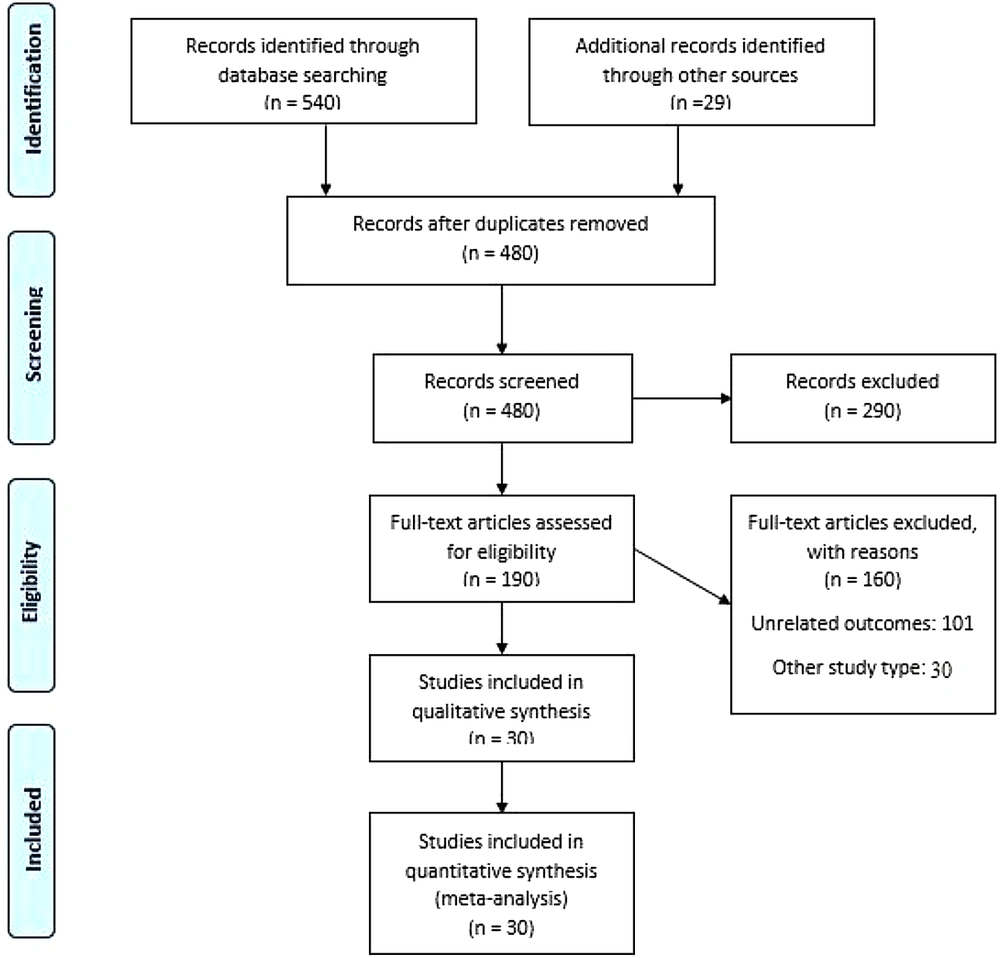
The query yielded a total of 569 articles, and after the removal of duplicates, 480 papers remained for screening based on title and abstract. Titles and abstracts were screened considering the inclusion and exclusion criteria, and finally, 190 articles remained for full-text screening. Following the full-text screening, 160 papers were deleted due to irrelevancy to the main goal, failure to determine hypertension prevalence as the primary study outcome, different statistical populations, and the lack of access to full-text. As a result, finally, 30 studies were selected for meta-analysis (Figure 1).
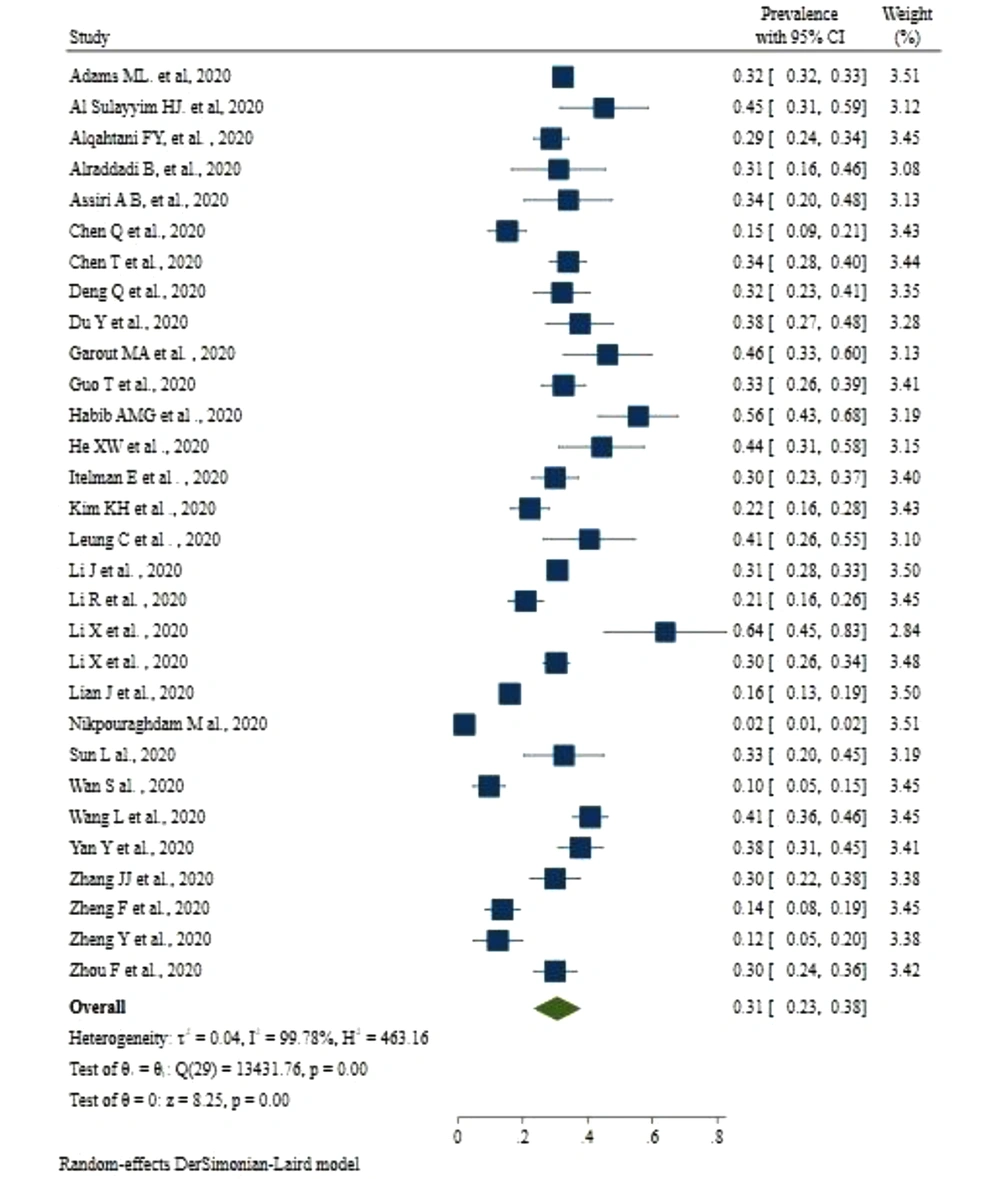
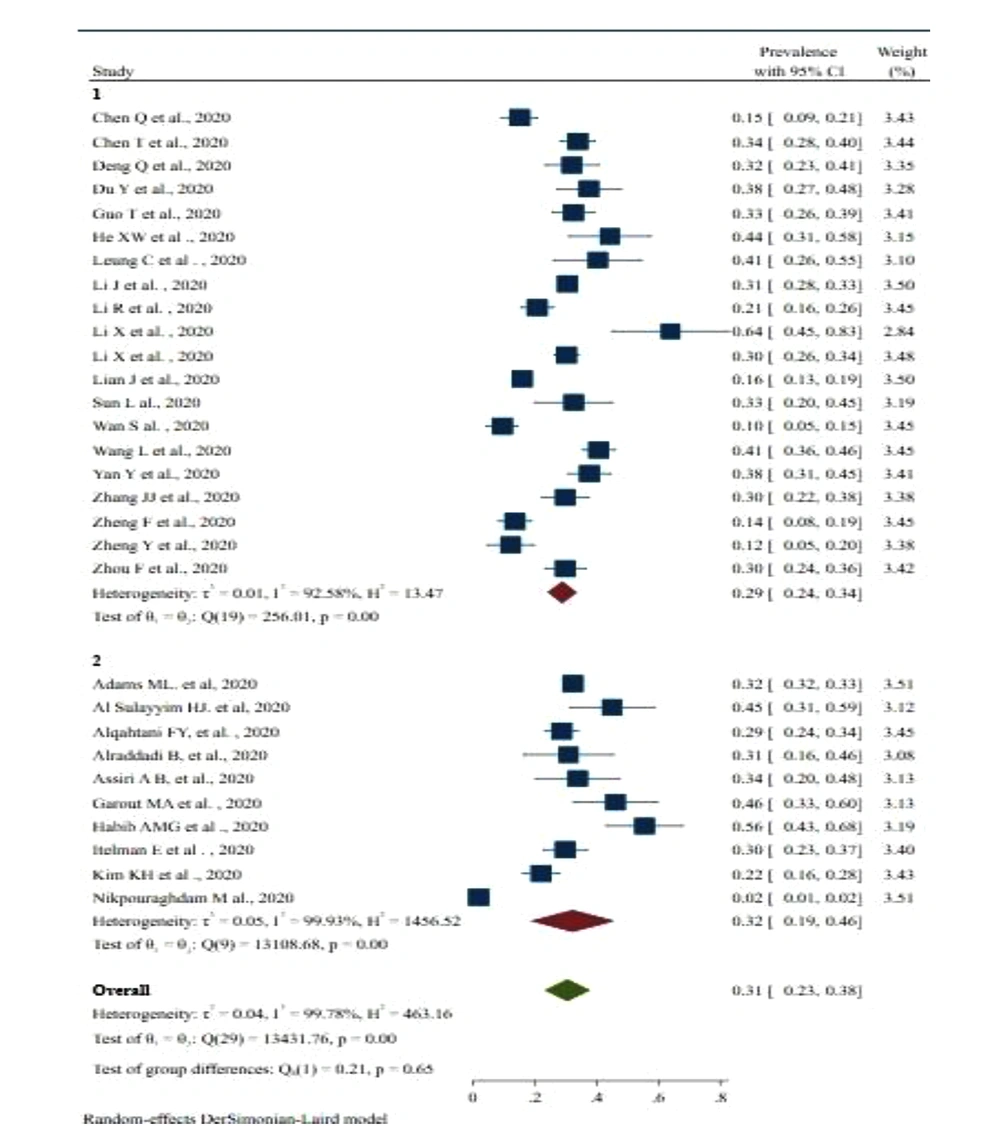
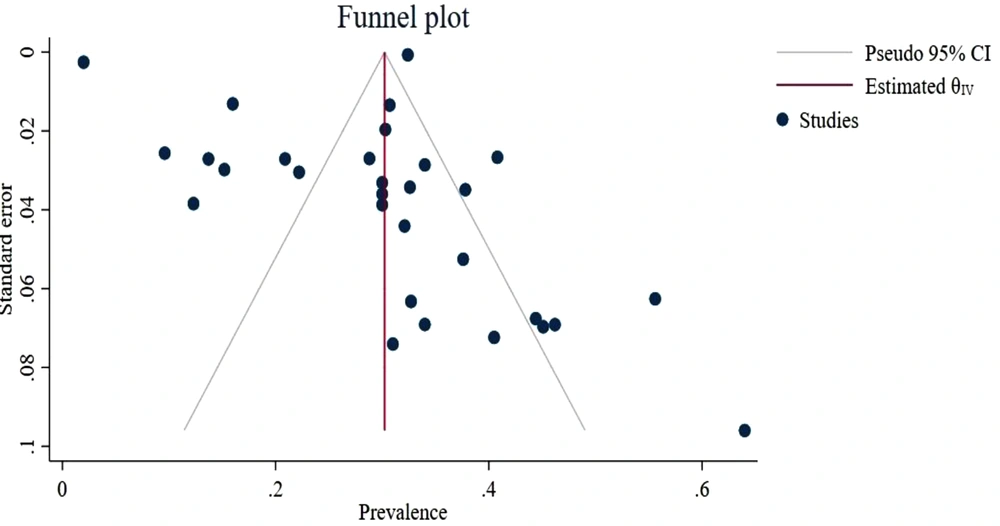
All the selected studies were statistical population was patients hospitalized with COVID-19. The prevalence had a range of 2 - 64% in different studies, and the highest prevalence was reported by Li et al. in China, while the lowest was in the study performed by Nikporghadam in Iran (17, 18). Among the investigations selected for meta-analysis, Iran and Israel conducted one study each, the United States and Korea together carried out one research (18-21), Saudi Arabia had five studies (22-26), and the rest belonged to China (17, 27-46) (Table 1). The final and cumulative prevalence of hypertension in patients with COVID-19 hospitalized worldwide in this study was found as 31%, with a confidence interval of 23 - 38%. The heterogeneity rate in this pooled prevalence was as high as 99.78%, attributed to variations in sample size, working method, and measurement technique in different studies included in this meta-analysis (Figure 2). Trim and Fill indicated publication bias in studies included in the meta-analysis. Egger test results were also significant (B = 3.94, SE = 1.74, P = 0.021). The findings are also presented as a funnel plot graph (Figure 3). The subgroup analysis results based on different countries demonstrated that hypertension prevalence in patients with COVID-19 in China was 29%, with a CI of 24 - 34%. In countries other than China, hypertension prevalence was 32%, with a CI of 19 - 46% (Figure 4).
| Author, Countries | Study Population (Study Type) | Sample Size by Gender | Age (y) | Prevalence of Hypertension | ||
|---|---|---|---|---|---|---|
| Male | Female | Total | ||||
| Li et al. (17) China | Patients with COVID-19 (A retrospective study) | 10 | 15 | 25 | 55 - 100 | 64 |
| Nikpouraghdam et al. (18) Iran | Patients with COVID-19 (A retrospective study) | 1955 | 1009 | 2964 | All ages | 1.99 |
| Itelman et al. (19) Israel | Patients with COVID-19 (A retrospective study) | 105 | 57 | 162 | 20 - 72 | 30 |
| Adams et al. (20) United States | Patients with 2019-nCoV pneumonia (A population-based cross-sectional study) | 191,193 | 241,695 | 444,649 | > 18 | 32.4 |
| Kim et al. (21) Korea | Middle East respiratory syndrome coronavirus infection (A retrospective study) | 111 | 75 | 186 | All ages | 22.2 |
| Alqahtani et al. (22) Saudi Arabia | Patients with Middle East respiratory syndrome coronavirus (A retrospective study) | 167 | 114 | 281 | All ages | 28.8 |
| Alraddadi et al. (23) Saudi Arabia | Patients with Middle East respiratory syndrome coronavirus (A cross-sectional study) | 21 | 18 | 39 | 1 - 79 | 31 |
| Assiri et al. (24) Saudi Arabia | Patients with COVID-19 (A descriptive study) | 36 | 11 | 47 | All ages | 34 |
| Garout et al. (25) Saudi Arabia | Patients with Middle East respiratory syndrome coronavirus infection (A retrospective study) | 40 | 12 | 52 | 15 - 85 | 46.2 |
| Habib et al. (26) Saudi Arabia | patients with Middle East respiratory syndrome coronavirus infection (A retrospective study) | 47 | 15 | 63 | All ages | 55.6 |
| Zhang et al. (27) China | Patients with COVID-19 (A retrospective study) | 71 | 69 | 140 | All ages | 30 |
| Zhou et al. (28) China | Patients with COVID-19 (A retrospective study) | 119 | 72 | 191 | 21 - 76 | 30 |
| Chen et al. (29) China | Patients with COVID-19 (A retrospective study) | 171 | 103 | 274 | All ages | 34 |
| Li et al. (30) China | Patients with COVID-19 (A retrospective study) | 279 | 269 | 548 | 18 - 95 | 30.3 |
| Chen et al. (31) China | Patients with COVID-19 (A retrospective study) | 79 | 66 | 145 | All ages | 15.2 |
| Deng et al. (32) China | Patients with COVID-19 (A retrospective study) | 57 | 55 | 112 | 49 - 70.8 | 32.1 |
| Du et al. (33) China | Patients with COVID-19 (A retrospective study) | 62 | 23 | 85 | All ages | 37.6 |
| Guo et al. (34) China | Patients with COVID-19 (A retrospective study) | 91 | 96 | 187 | All ages | 32.6 |
| He et al. (35) China | Patients with COVID-19 (A retrospective study) | 34 | 20 | 54 | All ages | 44.4 |
| Lian et al. (36) China | Patients with COVID-19 (A retrospective study) | 407 | 381 | 778 | All ages | 15.98 |
| Wang et al. (37) China | Patients with COVID-19 (A cross-sectional study) | 166 | 173 | 339 | All ages | 40.8 |
| Leung (38) China | Patients with COVID-19 (A cross-sectional study) | 46 | 0 | 46 | All ages | 40.5 |
| Li et al. (39) China | Patients with COVID-19 (A retrospective study) | 545 | 633 | 1178 | All ages | 30.7 |
| Li et al. (40) China | Patients with COVID-19 (A retrospective study) | 120 | 105 | 225 | 36 - 64 | 20.89 |
| Sun et al. (41) China | Patients with COVID-19 (A retrospective study) | 31 | 24 | 55 | All ages | 32.7 |
| Wan et al. (42) China | Patients with COVID-19 (A case series study) | 72 | 63 | 132 | All ages | 9.6 |
| Zheng et al. (43) China | Patients with COVID-19 (A retrospective study) | 80 | 81 | 161 | All ages | 13.7 |
| Zheng et al. (44) China | Patients with COVID-19 (A retrospective study) | 40 | 33 | 73 | 21-76 | 12.3 |
| Yan et al. (45) China | Patients with COVID-19 (A cross-sectional study) | 114 | 79 | 193 | All ages | 37.8 |
| Chen et al. (46) Taiwan/China | Patients with acute respiratory distress syndrome (A cross-sectional study) | 32 | 35 | 67 | 23-86 | 19.4 |
7. Discussion
After Middle East respiratory Syndrome and Severe Acute Respiratory Syndrome, COVID-19 is the third virus that caused an epidemic in the 21st century, posing a major challenge to all countries (27). The mode of transmission, diagnosis, and long incubation period (3 - 14 days) are among the main problems of this new virus. Furthermore, worldwide coronavirus transmission is affected by various factors and is difficult to identify. The outbreaks among family members and widespread transmission reported by healthcare workers further complicate the situation (47, 48).
Human society is not immune to COVID-19 because it is a newly identified infection. Moreover, no health measure has been developed to reduce the rapid spread of this new virus. This uncertainty complicates the situation for those with vulnerable conditions, including immunodeficiency, comorbidities, and the elderly. Despite the novelty of the subject, there are numerous studies on the history, mode of transmission, the urgency of response, potential pathological features, and prevention strategies for this disease (49). Nevertheless, there is a paucity of studies on the prevalence of underlying and associated diseases, such as hypertension. Therefore, the present meta-analysis and systematic study aimed to determine the prevalence of hypertension in COVID-19 patients worldwide.
The results of the current study revealed that the pooled prevalence in patients hospitalized with COVID-19 worldwide was 31% (95% CI: 23 - 38%). The range of changes in hypertension prevalence in different investigations included in the meta-analysis varied from 2 - 64%. In addition, the results of subgroup analysis based on different countries pointed out that hypertension prevalence in patients with COVID-19 in China and other countries was 29% (95% CI: 24 - 34%) and 32% (95% CI: 19 - 46%), respectively.
Due to the dearth of meta-analysis studies in this subject, the results of the current research were compared with some studies in this field Zhang et al. investigated the clinical features of 82 COVID-19-related deaths in China. The results of the latter study indicated that the majority of death cases (65.9%) were male. Furthermore, more than half of the dead patients (80.5%) aged 60 years or older, and the median age was 72.5 years. Fever, shortness of breath, and cough were the most common clinical symptoms in 78%, 64.6%, and 63.4% of cases, respectively. Radiologically, all patients had bilateral lung involvement. Moreover, 76.8% of cases had comorbidities, including hypertension, heart disease, diabetes, stroke, and cancers reported in 56.1%, 20.7%, 18.3%, 12.2%, and 7.3% of the individuals, respectively (50).
In another retrospective cohort study, Zhou et al. assessed the risk factors and clinical course for adult mortality of hospitalized COVID-19 patients in Wuhan, China. Out of 191 patients enrolled in the mentioned study, 137 cases were discharged, and 54 patients died at the hospital. It was reported that 91 (48%) patients had comorbidities, the most prevalent of which was hypertension reported in 58 (30%) patients, followed by diabetes and coronary heart disease in 36 (19%) and 15 (8%) patients, respectively (28). A meta-analysis and systematic review by Emami et al. investigated the prevalence of underlying diseases in patients admitted with COVID-19 (51).
Finally, ten studies with a population of 76,993 were included, indicating the collective prevalence of hypertension, cardiovascular diseases, smoking history, and diabetes as 16.37% (95% CI: 10.15%, 23.65%), 12.11% (95% CI: 4.40%, 22.75%), 7.63%, (95% CI: 3.83%, 12.43%), and 7.87% (95% CI: 6.57%, 9.28%), respectively (51). We observed that hypertension, cardiovascular diseases, diabetes, smoking, chronic obstructive pulmonary disease, malignancy, and chronic kidney disease were the most prevalent diseases among patients hospitalized with COVID-19. In conclusion, the results of this research and other preliminary studies in this field emphasize the high prevalence of hypertension in patients with COVID-19.
Some factors affect the increased mortality rate among hypertensive patients with COVID-19:
(1) One possibility is that these patients do not seek doctors for follow-up; therefore, their disease process gets out of control.
(2) During the pandemic, overcrowding in emergency departments delays the admission of patients with underlying diseases, which augments the mortality rate of these patients.
(3) Avoiding patients from receiving effective treatments against COVID-19 leads to the disease's progression.
7.1. Strengths and Weaknesses
Regarding the strengths of the present study, it should be noted that to the best of our knowledge, this research is one of the first systematic and meta-analytic studies on the pooled prevalence of hypertension in patients with COVID-19 worldwide. Another remarkable strength is the large number of selected articles in this meta-analysis, which reduces the possibility of selection bias in our findings. Cumulative estimates based on countries were also explained to determine the important sources of heterogeneity.
The current study also had limitations that need to be addressed. Firstly, degrees of selection bias may be present in this systematic review since the initial search may not potentially provide complete coverage of all available literature. Secondly, most of the studies included in the meta-analysis were related to China and may be underestimated because the data provided by China is under doubt.
7.2. Conclusions
According to the results of the present study, hypertension is one of the most common underlying diseases in patients with COVID-19. Therefore, the health needs of these patients should be addressed through implementing preventive and educational measures. A considerable number of patients with COVID-19 also have hypertension. Consequently, researchers should find ways to identify and treat COVID-19 in these patients to reduce their mortality rate. The following suggestions will help prevent and reduce mortality in hypertensive patients with COVID-19:
(1) Studies to evaluate the treatment process for patients with hypertension who have recovered from COVID-19
(2) Raising public health awareness and training of those with underlying diseases, such as hypertension, during the COVID-19 pandemic.
(3) Increasing the number of self-care programs, including preparing health education protocols and pamphlets
(4) Online treatment of underlying conditions, such as hypertension, in order to reduce the spread of the virus.