1. Background
Blood transfusion is one of the most important health issues in the modern world. Despite extensive advances in various fields of medicine, scientists have not yet been able to find a viable alternative to human blood, so the only source of blood is the already donated blood (1). World Health Organization states that about 87.5% of developing countries supply less than half of the blood requirements for their populations (2). On the other hand, the demand for blood bags in hospitals depends on the number of daily admission of patients with accident-related injuries, which cannot be well forecasted; therefore, in most cases, forecasting the daily demand of hospitals might not exactly correspond to their real demand (3). Various studies mentioned excessive blood ordering as a major cause of blood wastage (4-6). The importance of demand forecasting in the blood supply chain process and the criteria for measuring blood utilization in health care settings have been investigated in many studies (7, 8). Different management models and targeted interventions, such as using trained personnel for blood product transportation (8) and managing as well as reducing excessive orders of blood (9, 10), have been proposed and established in different countries. In Iran, based on comprehensive research during 2005 - 2015, the two main causes of blood product wastage were stated as date expiry and returned/reserved units of operating rooms and wards (1). On the other hand, 34.7% and 93% of the red blood cells (RBCs) wastage have been reported in surgery units in different medical centers of Iran (11, 12). Lack of standard guidelines for proper blood ordering and consumption is stated as a major problem leading to blood wastage in Southern Iran, as well (13). Enormous costs of preparing blood products, as well as relative costs of wasting blood, have received considerable attention from researchers worldwide (14, 15). Taken together, implementing efficient interventions for promoting blood product consumption is considered as one of the major health issues, especially in developing countries that are facing limitations in blood supply.
2. Objectives
Therefore, this study was designed to suggest an effective blood consumption management model based on determining the most influential initiatives using stakeholders’ opinions in the operating rooms of the largest tertiary referral hospital in Southern Iran.
3. Methods
In this cross-sectional study, 185 participants, consisting of 10 anesthesiologists, 33 surgeons, 75 anesthesiology technicians, and 67 surgical technicians, were enrolled during September and November 2019 in the Nemazee Hospital, the largest tertiary referral center in Southern Iran. Inclusion criteria were all anesthesiologists, surgeons, anesthesiology technicians, and surgical technicians working in the operating rooms during the study period who were willing to cooperate with us. Based on Mundfrom et al.’s study (16), the suggested minimums for the sample size are 3 to 20 times the number of variables. Therefore, our sample size is enough for confirmatory factor analysis (8 samples per item). The study protocol was approved by the Ethical Committee of the Islamic Azad University (ethics code: IR.IAU.SRB.REC.1398.078, approval code = 15899).
In the first step, a comprehensive literature search was done to determine the effective factors and initiatives previously reported for improvement of blood consumption management and decreasing blood wastage (Table 1).
| Author | Year | Country | Type of study | Problems/Aims | Factors/Interventions |
|---|---|---|---|---|---|
| Heitmiller et al. (8) | 2016 | USA | Interventional | Product obsolescence due to inaccurate detection of temperature index along the route | Increase access to blood transfusion tanks, use of objective tools such as labels and posters on tanks, and train transport officials |
| Venugopal et al. (17) | 2017 | India | Interventional | Evaluate the use of process improvement tools | The uniqueness of the staff and operator of the donor reception and guidance department to fill out the pre-donation form. Only one donor enters the pre-test room and medical examination room at a time to protect donor privacy and designating a separate waiting area for donors |
| Jovanovic et al. (18) | 2013 | Serbia | Interventional | Optimal use of blood products and minimizing the cost of blood loss | Implementation of the new Progress information system at the Blood Transfusion Institute |
| Improta et al. (19) | 2015 | Italy | Interventional | Reduce blood loss in the hospital and health care center | Multiple interventions and corrective actions to improve the efficiency of the care process |
| Toledo et al. (20) | 2013 | Colombia | Interventional | Enforcement of FIFO law | Clear expectations, improved teamwork, and a multidisciplinary clinical course |
| Soleymani et al. (21) | 2016 | Iran | Interventional | Non-consumption and return of blood packages from the wards or negligence of blood bank personnel to check the date of consumption of blood packages | Use of elusive blood care system based on tracer system |
| Alavi-Moghaddam et al. (22) | 2014 | Iran | Interventional | Ordering and consumption more than the need for blood | Type and screen protocol |
| Najafi et al. (23) | 2017 | Iran | Observational analytical | Excessive blood supply and unnecessary transfusions | Considering the "demand and supply uncertainty" factor that exists in the real world. Considering factors such as the certainty of the blood bank’s knowledge of the actual age of the blood received, Using Cross Matching electronic system based on blood bank information system to ensure the compatibility of donor and patient blood, Cross-match blood reservation for more than one patient, Determining the quality of blood as the age of the transferred blood. |
| Brue (24) | 2015 | USA | Interventional | Improper blood storage and transportation | Training programs, print, and digital messages, and ways to improve transportation and identify components |
| Whitney et al. (25) | 2015 | USA | Interventional | Enforcement of FIFO law | 1) Delivery of RBCs through pneumatic tube system, 2) No storage of RBCs in operating room refrigerators, 3) Lack of feedback on events leading to the loss of RBCs in surgeries, 4) Training of anesthesia and nursing staff in the area of liver transplantation |
| Kanani et al. (26) | 2017 | India | Interventional | Unnecessary orders, improper storage, and transportation of blood | 1) Use of advanced software in blood banks and general rooms of hospitalized patients, 2) Continuous medical training to technical personnel to empower them, 3) Understanding the quality indicators of processing and preparation of blood components and monitoring the rational use of blood |
| Javadzadeh Shahshahani et al. (27) | 2016 | Iran | Interventional | Expiry date due to non-return of blood to the blood bank, non-compliance with standards in the blood preparation process | Reducing RBCs to 7 days in the hospital, managing blood loss using standard operating procedures, regular staff training programs including standard methods of blood collection, processing, transportation and storage based on standard operating procedures Iranian Blood Transfusion Organization (IBTO), distribution and transfer of blood units between hospitals and regulatory centers for blood loss |
| Anani et al. (28) | 2018 | Iran | Interventional | Implement payment tariffs for blood products | Implement payment tariffs for blood products |
3.1. Search Strategy
Quantitative studies, including descriptive, observational, interventional, meta-analysis, and systematic review, as well as qualitative studies in the field of blood bag consumption management, were reviewed. Factors affecting the management of blood bag consumption were effectively examined to identify and investigate the patterns of blood bag consumption management. Databases and electronic articles, international and national, were searched through academic and non-academic digital networks. Restrictions on access to some of the databases made the search period longer and more limited. We searched international databases of PubMed, ProQuest, Ovid, Scopus, Web of Science, and CINAHL, as well as national databases (SID, Magiran, Iran doc, and Iranmedex) using various combinations of keywords related to the subject of “a proposed managerial model for improvement of blood consumption in the operating rooms in Southern Iran”, was searched. The criterion in this section was the availability of information and programs, and the keywords of “hospital management”, “blood bags”, “blood consumption”, “blood management”, “blood wastage” and “operating room” were used.
Data on the following items were collected: year of study, country of study, study method, study tools, and study results. Afterward, the indicators related to blood bag consumption management in developed and developing countries and factors affecting blood bag consumption management based on the five management dimensions were collected, and a preliminary model was formed.
In the second step, an expert panel was formed to develop an appropriate localized questionnaire. The invited experts were stakeholders of the transfusion practice in the hospital, including anesthesiologists, surgeons, and blood bank experts. Using the searched items and new suggestions, which were obtained using the brainstorming methods in 10 sessions, a total of 19 factors were identified as the potential influencing factors on the blood consumption management in our situation and presented as a researcher-made questionnaire with 23 items scored on a Likert scale. The effectiveness of each item on blood consumption management was considered as very low, low, moderate, high, and very high, which were ranked based on the viewpoints of the participants.
In the third step, the validity and reliability of the questionnaire were evaluated. To confirm the content validity ratio (CVR) and content validity index (CVI) (29), the questionnaire was evaluated by 10 experts in the fields of surgery, anesthesiology, epidemiology, PhD in the blood bank, and Ph.D. in hospital management to express their views on the quality of the items and help us to construct an appropriate questionnaire (29). Based on the Lawshe table, the minimum acceptable CVR (according to the number of evaluators) (29, 30), and the acceptable amount of CVI, all suggested factors obtained the required score to be included in the questionnaire (the acceptable value was 0.62 for CVR and 0.79 for CVI). Also, the reliability of the questionnaire was determined by internal consistency, with a Cronbach’s alpha of 88.9% obtained from a randomly selected sample (n = 50) from our studied population.
In the final step, the questionnaire was distributed to the participants to determine their opinions regarding the degree of effectiveness and prioritize areas of focus on blood consumption management. For better evaluation, related items of the questionnaire were classified into 5 dimensions of planning, organization process, resource allocation, leadership, and control.
3.2. Statistical Analysis
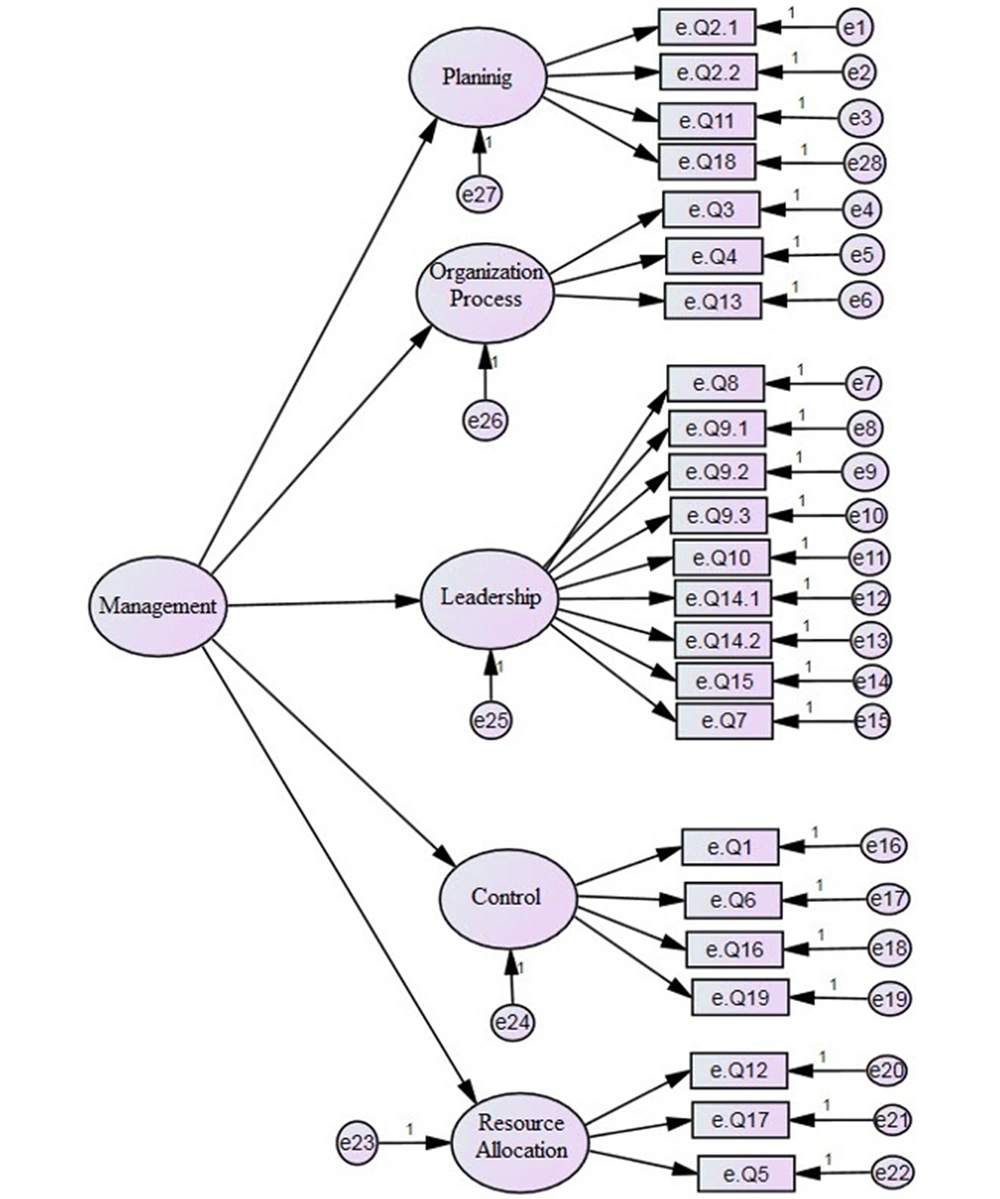
Data analysis was administered using AMOS version 21. A general model for the improvement of blood bag management was designed and evaluated by confirmatory factor analysis (CFA). In the confirmatory factor analysis, the researcher designs and tests the path model and the relationships between the obvious and the latent variables obtained based on previous information (14). Then, we described the fit index of the model, including Root Mean Square Error of Approximation (RMSEA < 0.05), Comparative Fit index (CFI > 0.90), Tucker-Lewis index (TLI > 0.90), and χ2/df (< 2). Statistical significance was considered when P-value < 0.05.
4. Results
Data of 185 participants (60 (32.5%) females and 125 (67.5%) males), with a mean age of 40.63 ± 12.31 years were analyzed. The CFA model is depicted in Figure 1. Five dimensions influencing blood consumption management in descending order were as follows: Resource allocation, control, and leadership, planning, and organization process.
Factor loading values of each factor are shown in Table 2. The standardized coefficients and a significant number of items are demonstrated in Table 3. Model fit indices had acceptable values, indicating the appropriateness of the proposed model (P = 0.032) (Table 4).
| Item | Resource Allocation | Control | Leadership | Planning | Organization Process | |
|---|---|---|---|---|---|---|
| Q1 | Monitor the use of blood products by blood supply agencies and hospitals on an annual basis | 0.682 | ||||
| Q2.1 | Report and publish information related to blood transfusion products and indicators on an annual basis through private websites and annual reports | 0.563 | ||||
| Q2.2 | Report and publish information related to blood transfusion products and indicators annually through special blood transfusion quarterly | 0.581 | ||||
| Q3 | Designing a systematic and user-friendly electronic software for ordering blood products in hospital | 0.619 | ||||
| Q4 | Designing and creating a site based on the central intranet and interstitial intranet, to connect different wards of the hospital | 0.603 | ||||
| Q5 | Evaluate and update the level of response to blood needs and demand by examining the factors affecting blood demand through hospital advisory committees | 0.648 | ||||
| Q6 | Detection of unsuccessful blood requests via monitoring the canceled transfusion injections and canceled surgeries | 0.713 | ||||
| Q7 | Use of national and international blood management guidelines, such as World Health Organization (WHO) and International Society of Blood Transfusion (ISBT) guidelines | 0.629 | ||||
| Q8 | Develop and implement blood transfusion guidelines to manage blood consumption according to the conditions in each ward or hospital, including the implementation of the MSBOS program (maximum amount of blood ordered) | 0.593 | ||||
| Q9.1 | Development of training programs to manage blood consumption through e-learning | 0.544 | ||||
| Q9.2 | Development of educational programs to manage blood consumption through meetings and lectures, retraining, and workshops | 0.643 | ||||
| Q9.3 | Development of educational programs to manage blood consumption through books, booklets, and publications | 0.580 | ||||
| Q10 | Carrying out blood transfusion operations between adjacent hospitals in the city so that the requested blood can be used by other hospitals if not used. | 0.572 | ||||
| Q11 | Recording complete details of the physician who ordered the blood bag with the seal and signature and commitment to the orders | 0.675 | ||||
| Q12 | Using trained personnel oriented to inventory management principles and blood bag handling, storage, and transportation rules | 0.714 | ||||
| Q13 | Design and creation of a user-friendly electronic system (computer) system to order blood products | 0.722 | ||||
| Q14.1 | Correction of anemia in patients before surgery through clinics and hospitals | 0.641 | ||||
| Q14.2 | Correction of the anemia of patients before surgery through special blood transfusion machines that are located in different parts of the city | 0.509 | ||||
| Q15 | Prioritizing consumption of older blood bags rather than the newer ones (FIFO: First In/First Out by Blood Banks) | 0.679 | ||||
| Q16 | Recording and reporting reasons for date expiry of blood products (e.g., excessive orders of blood bags) | 0.752 | ||||
| Q17 | Using of in-hospital safe blood transportation equipment | 0.746 | ||||
| Q18 | Electronic registration of blood products | 0.642 | ||||
| Q19 | Control and tracking of electronic information of blood bags | 0.691 |
| Item | Coefficient | T-Value | |
|---|---|---|---|
| Q1 | Monitor the use of blood products by blood supply agencies and hospitals on an annual basis | 0.57 | 11.30 |
| Q2.1 | Report and publish information related to blood transfusion products and indicators on an annual basis through private websites and annual reports | 0.49 | 23.05 |
| Q2.2 | Report and publish information related to blood transfusion products and indicators annually through special blood transfusion quarterly | 0.45 | 11.97 |
| Q3 | Designing a systematic and user-friendly electronic software for ordering blood products in hospital | 0.62 | 22.97 |
| Q4 | Designing and creating a site based on the central intranet and interstitial intranet, to connect different wards of the hospital | 0.46 | 13.52 |
| Q5 | Evaluate and update the level of response to blood needs and demand by examining the factors affecting blood demand through hospital advisory committees | 0.69 | 12.24 |
| Q6 | Detection of unsuccessful blood requests via monitoring the canceled transfusion injections and canceled surgeries | 0.71 | 14.82 |
| Q7 | Use of national and international blood management guidelines, such as World Health Organization (WHO) and International Society of Blood Transfusion (ISBT) guidelines | 0.58 | 35.32 |
| Q8 | Develop and implement blood transfusion guidelines to manage blood consumption according to the conditions in each ward or hospital, including the implementation of the MSBOS program (maximum amount of blood ordered) | 0.51 | 23.43 |
| Q9.1 | Development of training programs to manage blood consumption through e-learning | 0.46 | 10.48 |
| Q9.2 | Development of educational programs to manage blood consumption through meetings and lectures, retraining, and workshops | 0.49 | 15.67 |
| Q9.3 | Development of educational programs to manage blood consumption through books, booklets, and publications | 0.47 | 11.07 |
| Q10 | Carrying out blood transfusion operations between adjacent hospitals in the city, so that the requested blood can be used by other hospitals if not used. | 0.54 | 13.58 |
| Q11 | Recording complete details of the physician who ordered the blood bag with the seal and signature and commitment to the orders | 0.57 | 34.73 |
| Q12 | Using trained personnel oriented to inventory management principles and blood bag handling, storage, and transportation rules | 0.87 | 15.62 |
| Q13 | Design and creation of a user-friendly electronic system (computer) system to order blood products | 0.58 | 35.32 |
| Q14.1 | Correction of anemia in patients before surgery through clinics and hospitals | 0.49 | 17.36 |
| Q14.2 | Correction of the anemia of patients before surgery through special blood transfusion machines that are located in different parts of the city | 0.42 | 16.94 |
| Q15 | Prioritizing consumption of older blood bags rather than the newer ones (FIFO: first in/first out by blood banks) | 0.63 | 13.33 |
| Q16 | Recording and reporting reasons for date expiry of blood products (e.g., excessive orders of blood bags) | 0.82 | 16.29 |
| Q17 | Using in-hospital safe blood transportation equipment | 0.84 | 10.70 |
| Q18 | Electronic registration of blood products | 0.51 | 17.59 |
| Q19 | Control and tracking of electronic information of blood bags | 0.61 | 13.15 |
| Index | TLI | CFI | RMSEA | χ2/df | P-Value |
|---|---|---|---|---|---|
| Value | 0.905 | 0.913 | 0.050 | 1.252 | 0.032 |
zAbbreviations: CFI, comparative fit index; RMSEA, root mean square error of approximation; TLI, Tucker-Lewis index.
Table 5 demonstrates the most impressive interventions for improving blood consumption management in operating rooms based on the calculated coefficients in the suggested model. Interventions with less impact on blood consumption management in each dimension were as follow:
| Dimension | Items | Coefficient |
|---|---|---|
| Resource allocation | Q12: Using trained personnel oriented to inventory management principles and blood bag handling, storage, and transportation rules | 0.87 |
| Q17: Using in-hospital safe blood transportation equipment | 0.84 | |
| Control | Q16: Recording and reporting reasons for date expiry of blood products (e.g., excessive orders of blood bags) | 0.82 |
| Q6: Detecting unsuccessful blood requests via monitoring the canceled transfusion injections and canceled surgeries | 0.71 | |
| Leadership | Q15: Prioritizing consumption of older blood bags rather than the newer ones (FIFO: First In/First Out by Blood Banks) | 0.63 |
| Q7: Using national and international blood management guidelines, such as World Health Organization (WHO) and International Society of Blood Transfusion (ISBT) guidelines | 0.58 | |
| Planning | Q11: Recording complete details of the physician who ordered the blood bag with the seal and signature and commitment to the orders | 0.57 |
| Organization Process | Q3: Designing a systematic and user-friendly electronic software for ordering blood products in hospital | 0.62 |
Resource Allocation: Q5: Considering full-time specific blood bank experts in the operating rooms for supervising blood consumption process (0.69).
Control: Q19: Monitoring and tracing electronic data of blood bag consumption (0.61); Q1: Annual supervision of blood products use by blood supply institutions and hospitals (0.57).
Leadership: Q8: Preparing and implementing problem-based guidelines for blood consumption in each ward such as Maximum Surgical Blood Ordering Schedule (MSBOS) (0.51);
Q9 1-3: Developing an educational program on blood consumption management via electronic program (0.46), sessions, lectures, and workshops (0.49), or pamphlets and books (0.47);
Q10: The possibility of transportation of the unused blood bags between hospitals in one city (0.54);
Q14 1-2: Correcting anemia before operation in outpatient clinics and hospitals (0.49) or specific stations of blood transfusion organization in each city (0.42).
Planning: Q18: Convincing the hospital management to establish a coherent electronic system for recording blood data (0.51);
Q2 1-2: Annual reporting of blood utilization indices via the website (0.49) or quarterly blood product bulletin (0.45).
Organization process: Q13: Careful review of electronic medical records of surgical patients before surgery by the responsible physician (0.58),
Q4: Designing an Intranet website to better transfer blood consumption data between hospital wards (0.46).
5. Discussion
In the present study, factors and initiatives affecting the management of blood consumption in operating rooms were studied in a large tertiary referral hospital in southern Iran. The most impressive and practical interventions were determined based on the viewpoints of the surgeons, anesthesiologists, and technicians of the operating rooms and proposed as an effective model.
In the suggested model, resource allocation was determined as the most impressive managerial dimension, which its most effective factor was using trained and oriented personnel to inventory management principles and blood bag handling, storage, and transportation rules, followed by providing in-hospital safe and standard blood transportation equipment. Therefore, providing the required efficient and appropriate transportation equipment, such as monitoring temperature devices and specific protective boxes for different types of blood products, as well as suitable allocation of skilled personnel, not only can substantially reduce blood wastage but also improve blood bag consumption management in the hospital. In the same vein, Javadzadeh Shahshahani et al. (31) and Heitmiller et al. (8) showed that the use of trained personnel for transporting blood bags reduced the wastage of blood bags. Also, inappropriate transportation equipment has been recognized as one of the important factors causing RBC wastage in previously reported articles (8, 9). Moreover, Bots et al. (32) showed that straightforward interventions, particularly improving transport conditions, had a clear impact on the level of RBC wastage.
The second most influential dimension was "control". In this facet, the most impressive subject was evaluating and reporting reasons for the expiry date of blood products, such as excessive orders of blood bags in operating rooms. In accordance with our results, excessive order of blood was suggested as one of the major causes of blood wastage in several studies (9, 27, 33). Another important problem in our center that leads to a high amount of blood wastage is a high frequency of canceled transfusion injections, mainly due to canceled surgeries. It seems that implementing a designed control program can be highly efficient in this regard. Generally, managing the inventory by careful assessment of blood product supply and demand is one of the crucial issues in blood consumption management (34).
Concerning leadership, prioritizing consumption of older blood bags, rather than newer ones (FIFO: first in/first out), by blood banks was the most important factor influencing the management of blood usage in operating rooms. Our finding was similar to those of Stanger et al.’s (35) study, which showed that FIFO was one of the most important disciplines in reducing wastage. Likewise, Soleymani et al. (21) detected a 75% reduction rate in the loss of blood bags after implementing the FIFO law. The use of national and international blood management guidelines was recognized as another important factor improving blood consumption management, which should be taken into account with more caution.
In the planning dimension, creating responsibility for those ordering blood bags by signing and recording the details seems to be effective in increasing attention towards the appropriate ordering of blood products and decreasing the rate of wastage. In the last dimension, designing a systematic and user-friendly electronic software for registration of all data related to blood products was identified as the most important factor that can decrease blood wastage at the hospital. It seems that in developing countries, including Iran, this important issue has been neglected due to the shortage of financial resources; however, establishing a systematic electronic system for data registry translates into improved monitoring and tracking of inventories, resulting in better management and will be highly cost-effective in the field of blood consumption.
From less important influencing factors, implementation of problem-based guidelines for blood consumption in each ward, such as MSBOS, and establishment of a regular educational program with different teaching methods for related staff should be taken into consideration as well.
Our study was limited due to using data from a single center; however, as mentioned above this center was the largest referral tertiary center in Southern Iran.
5.1. Conclusions
While blood wastage is inevitable, situation analysis and determination of the most influential initiatives by related stakeholders in this field can effectively aid in the promotion of blood transfusion practice. Improvement in resource allocation was determined as the most influential dimension by focusing on using trained blood bank staff oriented to inventory management, handling, and transportation rules, as well as providing standard blood transportation equipment. Implementing a stepwise evidence-based blood consumption program based on the most prioritized suggested initiatives in the proposed model can be highly cost-effective in this respect.