1. Background
Cardiovascular diseases (CVDs) are considered the principal cause of early death in the world (1). Among CVDs, ischemic heart disease (IHD) is the most common one (2). IHD is a condition in which the myocardium receives inadequate oxygen as the result of an imbalance between myocardial oxygen supply and demand (3). Depending on the severity of stenosis in arteries and myocardial responses, angina pectoris (chest pain), sudden cardiac death, acute myocardial infarction (AMI), and chronic IHD are manifested (4). The global prevalence and mortality rate of IHD in 2017 was 126.5 million and 8.9 million individuals, respectively, which showed an increase of 74.5% and 52.3%, respectively, compared to 1990. Moreover, it was responsible for 15.3 million disability-adjusted life years (DALY) and 165 million years of life lost (YLL) in 2017 (5).
Although the mortality rates of CVDs have declined in the last decades in developed countries (2), the mortality rates and global burden caused by IHD have an upward trend in developing and newly developed countries, especially in the Eastern Mediterranean Region (EMR) (6), which has the highest prevalence of CVDs (7).
IHD was considered the first cause of mortality in Iran in 2019 (1). The age-standardized prevalence and mortality rate of IHD in Iran was 5143.08 per 100,000 people and 121.95 per 100,000 people in 2019, respectively (8). The impacts of IHD are not only limited to death and disability, but they also include critical health and economic outcomes (9). All countries are concerned mainly about the resulting costs of IHD. Among the different expenses of IHD, inpatient care accounted for more than half of the costs, followed by pharmaceutical treatment expenditure (10-14). In a study conducted by Schlatter et al. in Brazil, the average outpatient costs of IHD were 1521 USD, while its average inpatient costs were reported as 1976 USD in 2017 (15). In France, the direct medical costs of coronary artery disease (CAD) were estimated at 4183 million Euros, 50% of which came from inpatient care (16). A study by Darba et al. also revealed the inpatient costs of CAD at 1491.18 PPP $ (17), imposing costs equivalent to 0.5% of gross domestic product (GDP) in Iran in 2016 (17); these costs were estimated at 0.32% of GDP in Korea (18) and 3.37% of GDP in the United States (19).
Given the high burden of IHD and enormous financial costs on the health system and society, a few regional studies have investigated the costs of IHD in Iran. However, no comprehensive studies have been conducted on the inpatient costs of IHD and its determinants in Iran. The availability of correct information on the cost of illness can help make the right decisions on therapeutic and preventing plans. Furthermore, understanding the factors affecting the hospitalization costs can aid health policymakers to adopt control measures against the high costs of IHD.
2. Objectives
This study aimed to measure the hospitalization expenses of inpatients with IHD and analyze the influencing factors of these costs in Iran.
3. Methods
3.1. Study Design
This descriptive-analytical cross-sectional retrospective study was conducted in 31 provinces of Iran to evaluate the direct medical costs of inpatients with IHD from health system perspective. The bottom-up approach was used to calculate the costs. The micro-costs for each patient were extracted from the patients' hospital files. The hospitalization bills of all patients with IHD who were supported by Iran Health Insurance Organization were examined from August 23, 2019 to June 20, 2020. Only patients covered by Iran Health Insurance Organization were examined because it covers nearly half of the Iranian community and is known as the second largest insurance organization in Iran; it also provided the researcher a more complete and accurate data set. This organization has five insurance funds including civil servants, rural, Iranian, public health, and other sectors (20, 21).
Patients with IHD were identified by ICD-10 (the International Classification of Diseases Tenth Revision) codes of (I24.0, I24.1, I24.8, I24.9, I25.0, I25.1, I25.2, I25.3, I25.4, I25.5, I25.6, I25.8, and I25.9). Then, demographic information and hospitalization costs were gathered from the Health Information System of Iran Health Insurance Organization.
3.2. Sampling Method and Sample Size
This study was conducted using complete enumeration method. All the hospitalized IHD patients supported by Iran Health Organization funds were examined at the affiliated hospitals across Iran. The hospitalization files of 68726 patients with IHD were examined, of which 27369 files were excluded due to lacking the necessary criteria. Finally, 41357 files were included in the final analysis.
The excluded files were as follows:
(1) Fast track patients due to not being considered as inpatients
(2) Global records or per-case payment system (PPS) due to the low number (only four files)
(3) Patients with a LOS ≤ one day based on the experts’ opinions
(4) Patients with 0 or missing hospitalization costs
(5) Patients with missed data of LOS and the newly-established hospitals not accredited yet.
3.2.1. Fast Track Patients
The fast track consisted of three cubicles and a chair located near the emergency department but separate from the main department. The fast track system was designed for low acuity and ambulatory patients. So, the emphasis was on the rapid turnover, reducing waiting time, and LOS. These patients usually receive cares for less than six hours and are completely recovered and then discharged. Patients who need hospitalization or long-term care were transferred to other parts of emergency departments (22).
3.2.2. Global Records
The global payment system is the first example of a per-case payment system that covers about 60 common surgeries, for which payments are based on the average cost per case in Iran. We extracted the micro-costs for each patient from the patients' hospital files (23).
3.3. Variables and Their Measurement
The response variable was the sum of various expenses incurred during the hospitalization period, which consisted of visit and consultation, surgical services, drug, and consumable medical supplies, para-clinical services, laboratory tests, medical interventions, rehabilitation, nursing, and hoteling services, and other services. Also, the explanatory variables included demographic information (age, gender, and type of insurance fund), LOS, ICU admission (as a proxy of disease severity), accreditation grade, hospital ownership, and discharge status.
Hospital accreditation is the process of systematically evaluating and determining the credibility of a hospital conducted by an external organization using appropriate structural, procedural, and outcome standards (24). The accreditation degrees of hospitals are determined by their acquired scores. Accordingly, the hospitals are rated as top grade, grade 1, grade 2, grade 3, and non-standard.
The tariffs notified by Iran’s Ministry of Health and Medical Education are based on the accreditation grades of hospitals, such that hospitals with higher accreditation grades have higher charges (25).
Regarding hospital ownership, hospitals are classified as private, charity, social security, teaching governmental, and non-teaching governmental in Iran. The cost differences of hospitals depend on the tariffs approved by the government. These tariffs are divided into public and private groups. Private tariffs also include non-governmental public tariffs. Among these five classes, private hospitals use private tariffs, while teaching governmental and non-teaching governmental hospitals use public tariffs (26). Moreover, social security hospitals and charity hospitals benefit from a combination of public and private tariffs for their services (26).
3.4. Statistical Analysis
Percentage and frequency were employed to describe the characteristics of patients, whereas mean and standard deviation were utilized to describe hospitalization costs and relative variables. The following multiple linear regression model was adopted to analyze the factors affecting the hospitalization expenses (27, 28):
Y = α + B1X1 + B2X2 + ... BnXn + v
where α indicates a constant and v shows the random error. Furthermore, Xi refers to the ith factor affecting the hospitalization costs, and Bi is the regression factor of the ith independent variable proving the mean of variations in y when Xi increases or decreases by one unit under the assumption that other variables are constant.
Multiple regression analysis is a highly flexible system to examine the relationship between several independent variables and a single dependent variable. The independent variables may be quantitative or categorical (27, 28). Since the presumptions of the multiple linear regression model, ie, normality and consistency variance were not met, the logarithm of the response variable was determined based on ten to fulfill the model assumptions. When these assumptions were fulfilled, the multiple linear regression model was employed to estimate the coefficients of each variable. However, since the coefficients were obtained from logarithm based on ten, they were reversed to their first status. For this purpose, the inverse logarithm was used based on ten. All statistical tests were conducted at the significance level of P < 0.05 using the R 3.6.3 software. The costs were presented in both forms of Iranian Rials (IRR) and USD (2020) (1$ = 149000 IRR) (29)
4. Results
As provided in Table 1, 54.4% (n = 22483) of cases were male and 55.32% (n = 22882) were single. The mean age of hospitalized patients was 63.95 years (SD = 12.63), and the most prevalent age group was 61 - 70 years (31.6%, n = 13081). The minimum and maximum hospitalization days were 2 and 160 days, respectively, while the average LOS was 4.92 ± 5.41 days. The mean ICU LOS was 2.37 ± 3.93 days, and 63.5% (n = 26243) of patients had been admitted to the ICU. In term of accreditation grade, most hospitals received top grade and grade 1 (n = 39042, 94.4%). Regarding insurance coverage, most people were covered by rural insurance (n = 19253, 46.6%), and the lowest rate was related to Iranian health insurance (5.2%, n = 2130). Regarding the hospital ownership, 97.3% (n = 40252) of hospitals were teaching governmental hospitals, while 0.1% (n = 22) of them were social security hospitals. Moreover, 53.3% (n = 22053), 34.1% (n = 14113), 7.2% (n = 2988), 2.5% (n = 1014), 2% (n = 816), and 0.9% (n = 373) of patients were discharged with relative recovery, complete recovery, discharge against medical advice (DAMA), death, follow-up, and transfer to other medical centers, respectively. According to the findings of the multiple linear regression model in Table 1, hospitalization costs were significantly different in terms of age, gender, type of insurance, LOS, ICU stay, hospital accreditation degree, hospital ownership, and discharge status. The hospitalization costs of men were 24% higher than those of women. Patients aged 50 and below (23%), 51 - 60 (37%), 60 - 71 (38%), and 70 - 81 (27%) had significantly higher hospitalization costs than those aged above 80 years old.
| Variables | No. (%) | Coefficient | SE | Main Coefficient | P-Value |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 18874 (45.6) | 0.0952875 | 0.0032260 | 1.245 | < 0.001 |
| Female | 22483 (54.4) | Ref | |||
| Age | |||||
| ≤ 50 | 5677 (13.7) | 0.0906509 | 0.0066650 | 1.232 | < 0.001 |
| 51 - 60 | 10377 (25.1) | 0.1371036 | 0.0059389 | 1.37 | < 0.001 |
| 61 - 70 | 13081 (31.6) | 0.1392447 | 0.0057339 | 1.38 | < 0.001 |
| 71 - 80 | 7960 (19.2) | 0.1020007 | 0.0061347 | 1.27 | < 0.001 |
| > 80 | 4262 (10.3) | Ref | |||
| Accreditation grade | |||||
| Top grade and grade 1 | 39042 (94.4) | Ref | |||
| Grade 2 | 2236 (5.4) | -0.1763827 | 0.0469649 | 0.67 | < 0.001 |
| Grade 3 | 32 (0.1) | -0.4526562 | 0.0568424 | 0.35 | < 0.001 |
| Grade 4 | 47 (0.1) | -0.1411538 | 0.0070253 | 0.72 | < 0.001 |
| LOS | |||||
| ≥ 5 | 28160 (68.1) | 0.4654241 | 0.0035035 | 2.92 | < 0.001 |
| < 5 | 13197 (31.9) | Ref | |||
| ICU admission | |||||
| Yes | 26243 (63.5) | 0.2095755 | 0.0033662 | 1.62 | < 0.001 |
| No | 15114 (36.5) | Ref | |||
| Insurance fund | |||||
| Iranian | 2130 (5.2) | 0.090193 | 0.007845 | 1.21 | < 0.001 |
| Rural | 19253 (46.6) | -0.005515 | 0.004339 | 0.97 | < 0.01 |
| Other sectors | 5081 (12.3) | -0.014190 | 0.005776 | 0.95 | < 0.001 |
| Public health | 6686 (16.2) | 0.017837 | 0.005418 | 1.03 | < 0.01 |
| Civil servants | 8207 (19.8) | Ref | |||
| Hospital ownership | |||||
| Teaching governmental | 40252 (97.3) | Ref | |||
| Non-teaching governmental | 217 (0.5) | 0.0155020 | 0.0685513 | 1.03 | ns |
| Social security | 22 (0.1) | 0.0005965 | 0.0220488 | 1.001 | ns |
| Charity | 218 (0.5) | 0.1960379 | 0.0219046 | 1.57 | < 0.001 |
| Private | 648 (1.6) | 0.2820316 | 0.0130724 | 1.91 | < 0.001 |
| Discharge status | |||||
| Complete recovery | 14113 (34.1) | -0.2065434 | 0.0106285 | 0.63 | < 0.001 |
| Relative recovery | 22053 (53.3) | -0.2301226 | 0.0105107 | 0.59 | < 0.001 |
| Follow-up | 816 (2) | -0.2868844 | 0.0152341 | 0.51 | < 0.001 |
| Transfer to another center | 373 (0.9) | -0.3527438 | 0.0195632 | 0.44 | < 0.001 |
| Discharge against medical advice | 2988 (7.2) | -0.2046693 | 0.0118100 | 0.62 | < 0.001 |
| Death | 1014 (2.5) | Ref | |||
Regarding the accreditation grade, top-grade and first-grade hospitals had higher hospitalization costs. The Iranian insurance (21%) and public health insurance had significantly higher hospitalization costs than the civil servants insurance, whereas the hospitalization costs of patients with the insurance of other sectors (5%) and rural insurance (3%) were lower. The hospitalization costs of private hospitals (91%) and charity hospitals were higher than those of teaching governmental hospitals; however, no significant differences were reported between non-governmental public hospitals and non-teaching governmental hospitals in terms of hospitalization costs. The patients transferred to other centers (56%), in need of follow-up (49%), gained relative recovery (41%), and gained complete recovery (27%) had significantly lower hospitalization costs than the deceased patients.
R2 and Adjusted R, which have the same values in this study (0.437), mean that the variables in the model were able to predict 43% of the changes in the response variable. However, our main goal was not to make predictions, but to focus on R2 and Adjusted R.
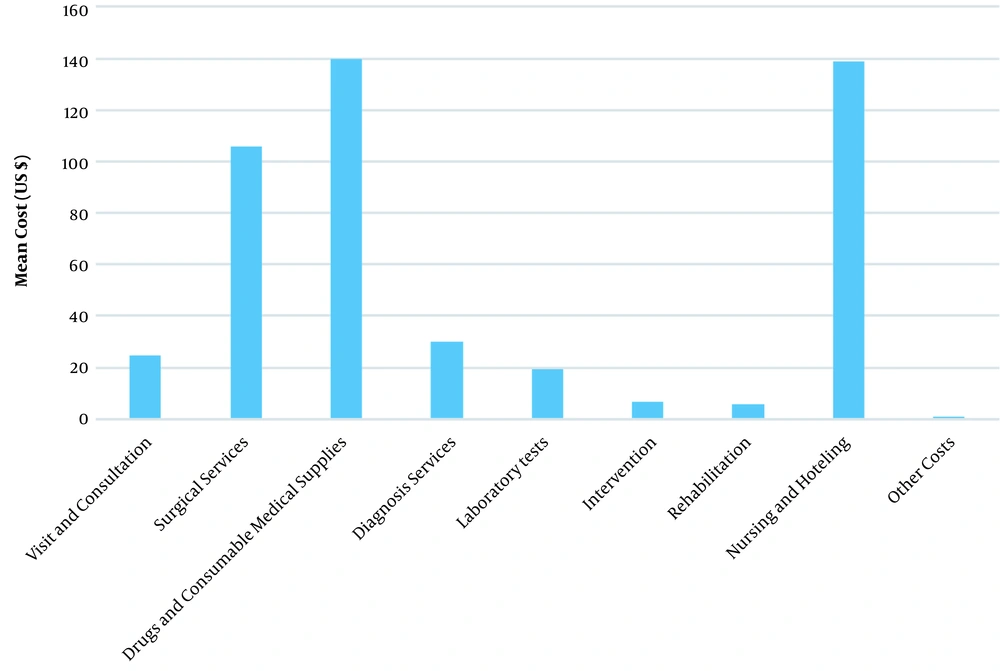
Table 2 illustrates the mean costs of hospitalization and its components in USD and IRR. The total hospitalization expenses and their average in 2020 were respectively 19.54 million USD and 472.51 USD. Among the components of hospitalization costs, the highest portions were attributed to drugs and consumable medical supplies (29.54%) and nursing service and hoteling (29.4%), followed by surgical services (22.53%), diagnosis services (6.4%), visit and consultation (5.22%), laboratory tests (4.08%), therapeutic interventions (1.46%), rehabilitation (1.2%), and other services (0.18%). The components of hospitalization costs have also been shown in Figure 1.
| Costs | Percent (%) | Minimum | Maximum | Mean (IRR) | Mean (US $) | SD |
|---|---|---|---|---|---|---|
| Hospitalization per patient | 100 | 17.7262 | 14,287.80 | 70404136.18 | 472.51 | 586.42 |
| Hospitalization per day | 100 | 8.9 | 1387.07 | 15442757.46 | 103.64 | 100.30 |
| Visit and consultation | 5.22 | 0 | 1,158.11 | 3675095.91 | 24.7 | 28.16 |
| Surgical services | 22.53 | 0 | 1,710.81 | 15862051.9 | 106 | 129.66 |
| Drugs and consumable medical supplies | 29.54 | 0 | 3,081.04 | 20790341.4 | 140 | 163.65 |
| Diagnosis services | 6.4 | 0 | 2,284.84 | 4505864.72 | 30.2 | 44 |
| Laboratory tests | 4.08 | 0 | 742.92 | 2872488.76 | 19.3 | 26.9 |
| Intervention | 1.46 | 0 | 1,024.8 | 1027900.4 | 6.9 | 33.78 |
| Rehabilitation | 1.2 | 0 | 1,173.17 | 844849.63 | 5.67 | 31.51 |
| Nursing and hoteling | 29.4 | 7.0173 | 7,422.94 | 20698816 | 139 | 174.62 |
| Others | 0.18 | 0 | 434.4 | 126727.44 | 0.85 | 7.37 |
5. Discussion
The main purpose of this study was to calculate the hospitalization expenditure of inpatients with IHD and analyze the related factors in Iran. The mean and standard deviation of hospitalization costs per patient and per hospitalization day was estimated at 586.42 ± 472.51 USD and 103.64 ± 100.29 USD, respectively, which were lower than the mean hospitalization costs of IHD patients in Hong Kong (3350 USD) (30) and Brazil (1976 USD) (15). Possible reasons for these differences might be due to the increased prices of medical equipment and services, modern medical technologies, differences in the healthcare models of the two countries, different samples and perspectives, inclusion criteria, calculation of costs, sanctions, and the dramatic fall of Iran’s currency. In Iran, governmental hospitals are subsidized by the state; thus, their tariffs are lower than the costs of services. Since the costs were based on the approved tariffs in this study, they were lower than the actual values. In some other studies conducted in the rural areas of China (31), urban areas of China (32), and Shanghai (33), the mean hospitalization costs of patients with chronic heart diseases was reported at 1012.47 USD, 6791.38 USD, and 2546.59 USD, respectively, which were also higher than those presented in our study. This might be due to the fact that these studies estimated the hospitalization costs of patients with chronic heart diseases, including myocardial infarction, angina pectoris, and IHD, but our research considered only patients with IHD. However, the mean hospitalization costs reported by the present study were higher than those suggested by Ribeiro et al. in public sectors in Brazil (34) and Darba et al. in Iran (17). Similar to a study conducted by Ding et al. (32), the highest shares of hospitalization costs were attributed to drugs and consumable medical supplies (140 USD, 29.54%) and nursing and hoteling services (139 USD, 29.4%). These high costs can be caused by the excessive use of cardiac stents and expensive cardiac drugs. Furthermore, the high costs of nursing and hoteling services can be explained by the fact that the majority of patients were in ICUs, where the expenses of human resources and bed-per-day are very high.
Our findings revealed a higher hospitalization cost among men than women, which was supported by previous studies (15, 31, 32, 35). Since men have more unhealthy life habits compared to women in Iran (eg, smoking and drinking alcoholic beverages), they have various underlying diseases and more severe CVDs (36). According to the findings, the age groups below 80 were significantly correlated with the increased hospitalization costs, which were much higher in patients aged 51 - 60 and 61 - 70 years old by 37% and 38%, respectively. Other studies also reported that younger patients had higher hospitalization costs than their older peers (31, 33, 37); this might be attributed to the fact that old patients selected relatively conservative treatments such as fewer cardiac stents, less aggressive therapies, and more drugs (32). There were also significant differences between the hospital costs in terms of their accreditation grades. The tariffs of hospitals were correlated with their accreditation grades (25, such that top-grade and grade 1 hospitals had higher costs than those of grade 2, grade 3, and grade 4.
The mean LOS for patients with IHD was reported as 4.92 days, which was close to the mean LOS for patients with CHD in China (4 days) (32) and United States (4.9 days) (38). However, some studies claimed longer mean LOS (31, 35). The LOS was significantly associated with the higher hospitalization costs, which was similar to some previous studies (31, 32, 39). Patients with excess hospitalization days had more critical illnesses, further comorbidity, and higher risk factors. Hence, they needed more resources and services over time and received aggressive measures that were positively related to higher costs (39). Consistent with some studies (35, 37), the present study revealed that ICU admission was significantly correlated with the increased hospitalization costs.
ICUs have the latest medical equipment and provide the highest level of medical and nursing care for critically ill patients. Therefore, the costs of hoteling and nursing services are high in ICUs.
Due to numerous serious differences between the structures of Iranian medical insurances and those of other countries, it was impossible to match the results with other countries. Based on the results, the highest mean of hospitalization costs was related to the Iranian and public health insurance funds, while the lowest average costs were seen in the funds of other sectors. Iranian health insurance and public health insurance funds cover the people without any medical insurance. These individuals usually apply for insurance notes only when they need to be hospitalized in the case of severe symptoms of diseases. They require lengthy stays and further diagnostic and therapeutic procedures that increase the average costs of these insurance funds compared to the other funds (40).
In this study, private and charity hospitals reported 91% and 57% increases in the mean hospitalization costs, respectively, compared to teaching governmental hospitals. A study conducted by Mehraban and Raghfar indicated that the catastrophic costs of healthcare services in private and charity hospitals were higher compared to other hospitals since the hoteling tariffs of private hospitals were 2.6 - 5 times higher than governmental tariffs (26). These findings were also confirmed by some previous studies (41, 42). As previously reported (34, 43), the mean hospitalization costs in the deceased patients were higher than the recovered ones. The deceased patients were unwell individuals with critical conditions who required a higher level of healthcare services, so in turn, had higher costs of treatment and drugs. In the present study, the patients transferred to other centers to receive healthcare services had the lowest hospitalization costs because the referring hospitals lacked expensive and specialized equipment and facilities for CVDs; therefore, they had lower hospitalization costs than the specialized centers.
A key strength of the present study is that its results can be used as input for health economics models and economic evaluations (such as cost-effectiveness). However, this study had some limitations. First, the statistical sample included only the patients supported by Iran health insurance funds, and it did not involve those supported by social security, armed forces, and private insurances. However, Iran Health Insurance Organization is the second largest insurance organization in Iran with 42 million clients, accounting for 65% of the entire population of Iran. Second, there were no data regarding household income, employment, education, number of hospitalizations, and comorbidity in the target group; these factors could have a significant effect on hospitalization costs, and the lack of them limited the multiple regression analyses. So, these problems should be solved in future studies. Third, we excluded the global records, which were different from the hospitalization records in terms of cost. It is suggested that future studies focus on the global records of ischemic heart patients and calculate their costs. Fourth, we did not consider overhead costs that may lead to low estimates of actual hospital costs, since overhead costs such as administration, laundry, cleaning, water, electricity, and those related to the LOS generally account for a large portion of total costs.
5.1. Conclusions
IHD is one of the most common, serious, and costly CVDs. Therefore, it is necessary to manage the treatment costs of this disease and evaluate its influencing factors. The cost information presented in this study can be used to calculate the economic burden of disease, cost-effectiveness of preventive and therapeutic interventions, and to identify strategies on hospital cost management related to this disease. Reducing the costs of IHD through prevention can help save the governmental budget; as a result, the state will be able to spend this portion of GDP improving other national conditions in other sectors. In addition, health policymakers can distribute resources more efficiently and optimally by knowing the costs of IHD.