1. Background
After the first case of COVID-19 was diagnosed in late December 2019, the highly contagious, deadly virus causing this disease rapidly spread worldwide. Almost three months later, the World Health Organization (WHO) declared the condition a pandemic (1). In such a pandemic, the knowledge and attitudes of the general population could be very crucial for disease control. Adequate awareness of a disease can always impact individuals' attitudes and practices, while negative attitudes and practices can increase the risk of morbidity and mortality (2-4). As every person may be a mobile source of infection, it is expected that improving the population's knowledge and taking the right actions to have a better attitude toward the disease would help prevent the further spread of the disease (5-9).
Since the beginning of COVID-19, numerous studies have examined the knowledge, attitude, and practice of COVID-19 patients in different parts of the world (10-13). The reviews and meta-analyses have indicated that knowledge, attitude, and practice components were almost acceptable (14-16). However, an Iranian study reported that a significant proportion of the general population showed a lack of knowledge, particularly about the outspread ways of COVID-19 and protective actions (17).
Research shows that people with chronic underlying diseases are at high risk of developing a severe form of the disease, and if they are affected by the virus, their mortality rate is much higher than those of others (6, 18-20). These people constitute an essential part of the emergency medical service (EMS) clients. However, in Iran, we recently recognized that when emergency medical technicians (EMTs) visited patients with chronic underlying diseases, many refused to be transferred to the hospital (21). It seems that most of them are worried about getting COVID-19 infection if they are transferred to the hospital, although in some cases, their underlying conditions worsen to the point that they need hospital care. On the other hand, several COVID-19 patients with chronic underlying diseases refuse to be transferred to the hospital, which seems to be rooted in their misconceptions about the disease and care in medical centers. However, to authorize our observations and better understand this group of EMS clients' level of knowledge and attitude, we needed a comprehensive study of this unique population.
2. Objectives
This study aimed to evaluate the knowledge and attitudes of patients suffering from a chronic underlying disease towards COVID-19, whether they were transferred to the hospital by Tehran EMS or not.
3. Methods
3.1. Study Design and Setting
This cross-sectional study was conducted from 21 May 2020 to 20 June 2020 in Tehran, Iran. The Tehran EMS center and Ethics Committee of the Iran University of Medical Sciences approved the study (IR.IUMS.REC.1399.227). Data gathering was conducted via telephone call interviews with eligible patients, and verbal informed consent was received before starting the conversation. We respected the participants' privacy, and all information was kept confidential. In all study processes, we committed to the principles of honesty and trustworthiness.
3.2. Study Population and Sampling
Using the registered data in the registry bank of the Tehran EMS center, eligible participants were selected from missions with possible diagnoses of cardiovascular disease, strokes, and altered mental status. They were divided into transferred and non-transferred groups based on the recorded data. Dissatisfaction with participating in the project and non-responsiveness were considered the exclusion criteria.
The percentage of acceptable knowledge and attitude (the correct answer to 60% of questions) about COVID-19 was 70% in the non-transferred group and 85% in the transferred group. Assuming a type-I error of 5% and a power of 80% to detect significant differences, the required sample size for each group was 174 people
3.3. Data Collection
A Farsi questionnaire was adopted from WHO course materials on emerging respiratory viruses, including COVID-19, and some other studies (22-24). The questionnaire comprised four parts. The first part included participants' demographic information, such as age, sex, occupational status, education level, and economic status. The second part consisted of 52 questions assessing the patients' knowledge about COVID-19. These questions were divided into five subcategories, including the most common symptoms of COVID-19 (14 questions), the main ways of disease transmission (14 questions), the primary protective ways (13 questions), the incubation period (one question), and high-risk groups (11 questions). A score of 0 was given to each incorrect answer and a score of 1 to each correct answer. The third part consisted of 12 questions to assess the patients' attitude towards COVID-19 based on a three-point Likert scale. The attitude score was 12 (true and logical/positive attitude) to -12 (wrong attitude). A neutral response (neither agree nor disagree) got a 0 score. These questions were divided into two domains: Nature of the disease (seven questions) and disease management by the pre-hospital and hospital system (five questions). The fourth part assessed patients' fear with five items: Having contact with infected people, eating out, going to the hospital, using the ambulance, and having contact with healthcare workers, which were answered based on a five-point Likert scale from very low to very much. According to these five questions, each participant's fear scores ranged from 5 to 25. The face and content validity of the questionnaire was assessed and approved by 15 experts (eight emergency medicine specialists, three researchers at Tehran EMS Center, three nurses, and one epidemiologist).
Select eligible individuals who agreed to enter the project were interviewed by telephone. Non-transferred participants were asked about the complications of the disease one week later.
We used the mean difference in knowledge scores for sample size calculation. Considering the mean difference of five points in knowledge between the two study groups (non-transferred and transferred) and a standard deviation of 15 for the knowledge score of each group, and assuming a type-I error of 5% and a power of 90% to detect significant differences, the required sample size for each group was 190 people. Considering responsiveness and cooperation of 80%, we determined 228 individuals as the sample size for each group, and then simple random sampling was done to select among the eligible cases.
3.4. Statistical Analysis
The data were analyzed using descriptive statistics, like frequency, percentage, mean, and standard deviation (SD), presented in tables and figures, as appropriate. The relationship with categorical variables was assessed by the chi-square or Fisher's exact test. The mean differences of numerical variables in the two study groups (non-transferred and transferred) were evaluated by the independent t-test. Also, we used the ANCOVA test for assessing the mean score of knowledge after adjusting for confounding factors like sex and education level. A p value lower than 0.05 was considered statistically significant. All statistical analyses were conducted via Stata v14.2.
4. Results
4.1. Baseline Findings
In the transferred patient group, we called 230 individuals, 201 of whom replied. In the non-transferred patient group, we called 230 individuals, 158 of whom answered. The mean age of the transferred group was lower than that of the non-transferred group (57.1 ± 16.1 vs. 62.0 ± 17.4 years; P = 0.006). Table 1 shows the basic and demographic information of the transferred and non-transferred patients. Based on the findings, the two study groups were statistically different concerning the mean age, sex ratio, occupational status, and education level (P < 0.05), but not in terms of economic status (P = 0.364).
| Variables | Transferred (N = 201) | Non-transferred (N = 158) | P-Value b |
|---|---|---|---|
| Sex | < 0.001 | ||
| Male | 111 (55.2) | 57 (36.1) | |
| Female | 90 (44.8) | 101 (63.9) | |
| Occupational status | < 0.001 | ||
| Employed | 82 (40.8) | 30 (19.0) | |
| Housewife/unemployed | 93 (46.3) | 89 (56.3) | |
| Retired | 26 (12.9) | 39 (24.7) | |
| Education level | < 0.001 | ||
| Under diploma | 72 (35.8) | 95 (60.1) | |
| Diploma | 63 (31.3) | 31 (19.6) | |
| Bachelor | 52 (25.9) | 25 (15.8) | |
| Master or above | 14 (7.0) | 7 (4.4) | |
| Economic status | 0.364 | ||
| Good or very good | 21 (10.4) | 20 (12.7) | |
| Moderate | 67 (33.3) | 42 (26.6) | |
| Bad or very bad | 113 (56.2) | 96 (60.8) |
a Values are expressed as No. (%).
b Based on the chi-square test
4.2. Consequences in the Non-transferred Group
The details of the consequences for non-transferred patients are reported in Table 2. Although most non-transferred patients (41.1%) felt better and did not report any consequences, 28.5% went to outpatient clinics and 23.4% to hospitals by themselves after EMS visits. The hospitalization, ICU, and CCU admission rates were 54.2%, 6.0%, and 17.9% in the transferred group, respectively, which were significantly higher than the rates in the non-transferred group (P < 0.001, P = 0.022, and P < 0.001, respectively). The results showed that non-transferred patients admitted to general wards had significantly higher mean days of hospitalization than the transferred patients (5.9 ± 3.8 vs. 2.5 ± 2.8 days; P < 0.001). There was not any significant difference in terms of mean days of hospitalization between those admitted to ICU versus those admitted in CCU (6.0 ± 5.0 vs. 4.7 ± 3.6 days; P = 0.462). There were three mortalities (of 161 responsive calls) in the non-transferred group and 13 mortalities (of 214 responsive calls) in the transferred group (1.9% vs. 6.1%; P = 0.04).
| Consequence | Values |
|---|---|
| No consequence (recovery) | 65 (41.1) |
| Recurrent symptoms | 2 (1.3) |
| Recalling the EMS | 1 (0.6) |
| Going to the clinic | 45 (28.5) |
| Calling a general physician or specialized medical consulting center | 8 (5.1) |
| Going to the hospital | 37 (23.4) |
| Hospitalization | 14 (8.9) |
| Hospitalization duration (d) | 5.9 ± 3.8 |
| ICU admission | 2 (1.3) |
| ICU admission duration (d) | 6.7 ± 6.7 |
| CCU admission | 3 (1.9) |
| CCU admission duration (days) | 5.0 ± 2.8 |
a Values are expressed as No. (%) or mean ± SD.
4.3. Reasons for Refusing to Transfer
The details of reasons for refusing to transfer are reported in Table 3. The most frequent reason was "a sense of well-being and no need for more follow-up" (36.1%). "Fear of hospital infection with COVID-19" stood in second place with 31.6% frequency.
| Mentioned Reasons | No. (%) |
|---|---|
| A sense of well-being and no need for more follow-up | 57 (36.1) |
| Fear of hospital infection | 50 (31.6) |
| Request to be transferred to a private hospital | 14 (8.9) |
| No need for transfer, according to the EMS personnel | 8 (5.1) |
| History of treatment in another hospital | 9 (5.7) |
| The suggested hospital was teaching or crowded, causing a waste of time | 7 (4.4) |
| Having problems with hospital costs | 6 (3.8) |
| The suggested hospital was inappropriate | 4 (2.5) |
| Request for the ambulance just for consulting and visiting at the home | 2 (1.3) |
| Having a negative experience in the suggested hospital | 2 (1.3) |
| Fear of ambulance infection | 2 (1.3) |
4.4. Knowledge
The mean knowledge score had no statistically significant difference between transferred and non-transferred patients (28.8 ± 5.7 vs. 28.2 ± 5.4; P = 0.320). Also, the mean score of knowledge was not statistically significant after adjusting for sex (P = 0.419) and education level (P < 0.001) based on ANCOVA (P = 0.637). Table 4 represents the details of obtained scores in the five subcategories. We found no statistically significant difference between the groups, except for knowledge regarding "high-risk groups" and "incubation period" that was higher in transferred patients than in non-transferred ones. The mean score of knowledge about the three common symptoms (dyspnea, cough, and fever) was significantly higher in the transferred group than in the non-transferred group (2.9±0.41 vs. 2.7±0.59, P = 0.003).
| Subcategories | Transferred | Non-transferred | P-Value* |
|---|---|---|---|
| Symptoms | 5.2 ± 2.3 | 5.5 ± 2.6 | 0.321 |
| Transmission | 8.2 ± 2.4 | 7.8 ± 2.3 | 0.135 |
| Prevention | 9.2 ± 1.8 | 9.3 ± 1.6 | 0.739 |
| Incubation period | 0.7 ± 0.5 | 0.7 ± 0.5 | 0.377 |
| High-risk groups | 5.4 ± 1.2 | 4.5 ± 1.6 | < 0.001 |
| Total score | 28.8 ± 5.7 | 28.2 ± 5.4 | 0.320 |
a Values are expressed as mean ± SD.
b based on the independent t-test
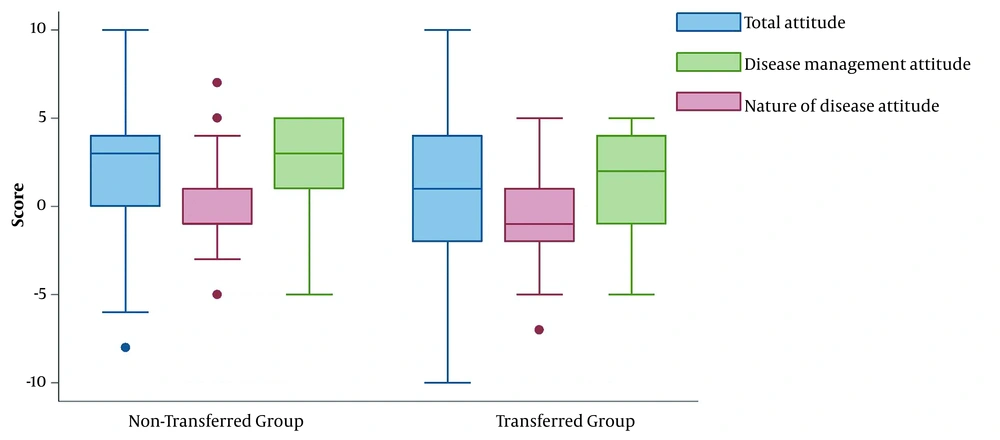
4.5. Attitude
The total attitude score for each person was -8 to +10 and -10 to +10 in the non-transferred and transferred groups, respectively. Figure 1 shows the distribution of the total attitude score in the two study groups. The mean attitude score was lower (true and more logical/positive attitude) in the transferred group than in the non-transferred group, and the difference was statistically significant (0.75 ± 3.7 vs. 2.2 ± 3.5; P = 0.001). This difference was related to the domain “disease management in the pre-hospital and hospital system.” Although attitude in both groups was positive, the mean attitude score for this domain was lower in the transferred group than in the non-transferred group (1.0 ± 3.3 vs. 2.4 ± 2.8; P < 0.001). The mean score of attitude toward the domain “nature of the disease” was negative in both groups, and the mean difference was not statistically significant (-0.24 ± 2.3 vs. -0.14 ± 2.3; P = 0.662).
4.6. Fear
The mean fear score was 16.0 (SD = 5.1) in the non-transferred group and 15.0 (SD = 5.6) in the transferred group. The mean fear score had no statistically significant difference between the two groups (P = 0.101). The transferred group had a lower score than the non-transferred one in some domains of fear. For example, 34.5% of transferred patients and 47.6% of non-transferred patients had very much fear of eating out, and this difference was statistically significant (P = 0.002). More details are presented in Table 5.
| Fear of… | Non-Transferred | Transferred | P-Value* | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Very Low | Low | Medium | Much | Very Much | Very Low | Low | Medium | Much | Very Much | ||
| Having contact with infected people | 20 (13.6) | 15 (10.2) | 29 (19.7) | 35 (23.8) | 48 (32.7) | 28 (14.0) | 26 (13.0) | 51 (25.5) | 28 (14.0) | 67 (33.5) | 0.174 |
| Eating out | 4 (2.7) | 9 (6.1) | 25 (17.0) | 39 (26.5) | 70 (47.6) | 18 (9.0) | 27 (13.5) | 46 (23.0) | 40 (20.0) | 69 (34.5) | 0.002 |
| Going to the hospital | 24 (16.3) | 27 (18.4) | 46 (31.3) | 21 (14.3) | 29 (19.7) | 35 (17.5) | 45 (22.5) | 47 (23.5) | 33 (16.5) | 40 (20.0) | 0.565 |
| Using the ambulance | 27 (18.4) | 37 (25.2) | 38 (25.9) | 19 (12.9) | 26 (17.7) | 45 (22.5) | 53 (26.5) | 43 (21.5) | 28 (14.0) | 31 (15.5) | 0.780 |
| Having contact with healthcare workers | 49 (33.6) | 31 (21.2) | 32 (21.9) | 18 (12.3) | 16 (11.0) | 74 (37.0) | 47 (23.5) | 38 (19.0) | 20 (10.0) | 21 (10.5) | 0.868 |
a Values are expressed as No. (%).
b Based on chi-square test
5. Discussion
In this study, we found that those refusing to transfer to the hospital against the EMTs' advice were mostly housewives/unemployed females, and had a lower education level and a higher mean age than those who were transferred. Although most non-transferred patients had no consequences, some were later admitted to the ICU or CCU, and even three cases died. Also, the hospitalization length was significantly higher in those who refused to transfer to the hospital by the EMS and later went to the hospital by themselves than in those transferred by the EMS. Most participants in both groups did not have sufficient knowledge of the disease, but the average attitude was positive. The mean fear score of the non-transferred group was also higher than that of the transferred group.
Previous studies have shown that the refusal to transfer increased during COVID-19 (25, 26). The voluntary refusal was accompanied by decreased EMS transports to Emergency Departments (EDs), which was disproportionately present among women and vulnerable groups. Although most non-transferred patients had no consequences, the hospitalization length was significantly higher in those who refused to transfer to the hospital by the EMS and later went to the hospital by themselves than in those transferred by the EMS, and importantly, some non-transferred patients died.
It is a great concern that severe patients with obvious signs of deterioration postpone referring to medical centers due to fear of COVID-19 transmission (27). The fear of disease transmission may result in behavioral changes like personal health decisions (28, 29). When it comes to the reasons for refusing to transfer, interestingly, a considerable number (almost 30%) mentioned "fear of hospital infection," and also some requested to be transferred to a private hospital. Although fear plays a significant role, many patients with fewer immediate complaints are less likely to refer to EDs, which leads to less ED collapse and other indirect effects of quarantine like social distancing. Nevertheless, it has been reported that patients with emergency conditions contributed to reduced ED utilization (30, 31), and they postponed referring to emergency care for this fear (32, 33). These findings convey that we need to improve hospitals' conditions to provide care for patients in pandemics like COVID-19 because we need our people's trust in the community health system. Otherwise, we cannot stand against major health issues like this pandemic.
The mean score of knowledge was not statistically significant between the two groups. It was found that patients had some misinformation, like the use of herbal medicines in protection against the disease. People have been exposed to many sources of information and misinformation about COVID-19 since the start of the disease (34-36). Therefore, to confront this epidemic, we should give people efficient and accurate health information and warn them about incorrect information, as maintaining society's safety is crucial.
This study also showed that the mean general attitude was positive. However, the attitudes of both transferred and non-transferred groups were negative/irrational toward the nature of the disease, and the two groups were not different in this regard. Concerning the pre-hospital/hospital management of the disease, although both groups had a positive attitude, the transferred group had a significantly lower positive attitude than the non-transfer group. One reason for this contradiction is that the transferred group was probably more ill, and they agreed to transfer despite their negative attitude toward disease management. Besides, considering that the study retrospectively examined the participants' knowledge and attitude and the hospitals were crowded during the pick of the epidemic, the transferred group received lower quality of services than before the pandemic, which may have led to their negative attitude towards disease management. On the other hand, the non-transferred group had a more positive attitude because they were unaware of the hospitals' overcrowding or other ongoing situations.
We also measured the fear of COVID-19 among the patients. The results showed that patients in the two groups had almost the same fear score, but in some aspects, such as fear of contact with health care workers, the non-transferred group had higher scores than the transferred group. This fear can be the reason for the refusal of these patients to transfer, so we should adopt proper strategies to guide people and assure them that they should trust health care workers because they need their help in this pandemic more than before. The same situation was seen in previous pandemics, and feared persons usually postponed seeking care (37). Also, designating referral hospitals for infected patients in pandemics and not involving all hospitals can help manage and control the disease and reduce people's fear of the possibility of being infected.
The best way to cut the transmission chain in pandemics is to stop person-to-person spreading. To reach this goal, we should find every defect in people's knowledge about the disease, especially those who are more vulnerable, and try to improve their understanding. Nowadays, the world is influenced by the internet, social media, and TV programs. Almost all people get information about anything from these ways, so the government and the health ministry should use these platforms to inform people about this pandemic. Also, we should consider the whole society in notice because those who are less educated or live in rural areas have different ways of getting information that may be inaccurate. In facing a pandemic like COVID-19, it is necessary to know about people's knowledge and attitude toward the disease, which can help prevent the spread of the disease. In any pandemic, we should detect vulnerable people like older adults and those with underlying illnesses and know about the challenges in their knowledge and attitude toward the disease. During pandemics, all systems, including the media, focus on disease management and control. Neglecting certain issues can indirectly increase the consequences of pandemics. One of the most critical issues in emergency patients is that they may be delayed in receiving vital care or refuse to be transferred to the hospital due to fear or lack of proper knowledge and attitude toward the conditions. Therefore, officials, the public health system, and the media have critical roles. Besides providing adequate information to control the disease, they should develop appropriate strategies to reduce people's negative and incorrect attitudes and fears, especially high-risk ones. Patients diagnosed with heart and brain problems are susceptible to delays in receiving treatment, which can cause mortality and morbidity. Several studies have shown that the rate of PPCI during pandemics is significantly lower than before, which can be due to the fear of contamination.
Following COVID-19, EMS should prepare for patients' changed behavior by focusing on high-risk groups and convincing them to be transferred to a medical center. Moreover, applying different EMS models can improve it by increasing the transfer of emergent patients and decreasing the transfer of non-emergent patients.
There are some limitations to our study. One of them is the small study population because we studied patients in one Iranian city. If we could conduct the study in some different cities with different study populations, the results would possibly change, and we could generalize the results to the whole country.
5.1. Conclusions
In this study, we found that most of the Tehran EMS clients who suffered from a chronic underlying disease, whether transferred or not transferred to the hospital, had not an acceptable knowledge of the disease. However, the average of their attitudes was positive. These findings highlight the need for specific actions by the government health system on this unique population for improving their knowledge and attitude toward COVID-19. These measures may help treat their underlying disease, if necessary, to receive in-hospital services while managing the risk of getting COVID-19 infection.