1. Background
The financial burden of non-communicable diseases is high in most countries around the world, and more and more families seem to fall into poverty due to chronic diseases (1). The out-of-pocket payment (OOP) of healthcare services can limit the household budget and expose the household members to several financial problems. Each year, millions of people face financial difficulty meeting their living expenses due to high healthcare expenditures, and vulnerable populations are forced to spend their income on health services (2). The costs of diagnosis and treatment of diseases can increase the rate of poor households, especially in rural areas; accordingly, human rights organizations, including the World Health Organization (WHO), have emphasized the need for universal health coverage. This goal cannot be achieved unless access to healthcare services is available for all people, without the incidence of catastrophic expenditures (3, 4).
Catastrophic health expenditures (CHEs) and the fair financial contribution index (FFCI), as major indices for evaluating the performance of healthcare systems, represent the level of financial support for people facing health expenditures (5). These indices are considered unfair when the household payments for health services significantly exceed the household budget (6). CHEs occur when OOPs exceed 10% of the total annual income or 40% of the household payment capacity. The FFCI indicates the level of inequality in OOPs for health, with scores ranging from 0 (perfect inequality) to 1 (perfect equality). According to some studies, about two-thirds of chronically ill patients and 42% of chronically ill households face CHEs due to insufficient financial support (7, 8).
Cancer, as a chronic non-communicable disease, can increase the risk of CHEs (9). This disease is caused by uncontrolled cell proliferation, which may extend to other body organs (10). More than 100 types of cancer have been identified so far, which are treated using various methods, including surgery, chemotherapy, and radiotherapy, depending on the type of disease. According to the global report of the International Cancer Agency in 2020, the number of new cases and deaths caused by cancer was estimated at 19.3 and 10 million people, respectively (11, 12), suggesting a significant increase compared to previous global cancer studies (13, 14).
In 2010, nearly 808 million people around the world faced CHEs. Due to a rapid increase in the number of new cancer cases over the past decade, the financial burden of this disease has increased. Research suggests that any type of expenditure imposed directly on households reduces their tendency to use health services. Therefore, the compulsory prepayment system (insurance), funded by tax credits or compulsory insurance premiums, is the most effective and fair approach to finance the treatment expenditures of cancer patients (15, 16).
In a cross-sectional study, Rezapour et al. examined the effects of direct OOPs on 2,200 households in Tehran, Iran, using two approaches of CHE and impoverishing health expenditure. According to their results, although the need for healthcare services was strongly felt in poor households, inequality in access to these services was evident, and healthcare utilization was higher in affluent groups and households. Their findings showed that the educational level of the household head, household size, and frequency of inpatient care service utilization had positive relationships with the possibility of facing catastrophic expenditures, while the presence of a preschool child in the household reduced the likelihood of these expenditures. However, health insurance did not show a significant relationship with the rate of exposure to catastrophic expenditures (17).
Additionally, in a descriptive analytical study by Kavosi et al., CHEs and coping strategies were investigated in the households of cancer patients in Namazi Hospital of Shiraz, Iran. Their results showed that 67% of families of cancer patients experienced CHEs. There was a significant relationship between CHEs and type of insurance, history of outpatient services, type of cancer treatment, and household members refusing to receive health services (18). Moreover, Piroozi et al. investigated the determinants and inequality of CHEs in diabetes mellitus treatment in Iran. The results of their study showed that 57.5% of the patients were exposed to CHEs. The socioeconomic status, sex, and marital status were the main determinants of CHE inequality among patients with type 2 diabetes mellitus (19).
Kasahun et al. investigated the rate of exposure to catastrophic expenditures among cancer patients in Ethiopia’s capital and found that 74.4% of cancer patient households faced catastrophic expenditures. Based on the results of their study on the type of treatment, chemotherapy imposed more catastrophic expenditures than radiotherapy. Moreover, households with lower income were more exposed to the catastrophic expenditures of cancer. With advancing age and increasing frequency of chemotherapy, exposure to the catastrophic expenditures of cancer has also increased (20). Moreover, the incidence and mortality rates of cancer have increased in Iran in recent years (21). Therefore, the current study was carried out, as little research has been conducted on cancer-related CHEs in Iran.
2. Objectives
The present study aimed to investigate the equality of financing for cancer treatment, to estimate CHEs, and to determine the influential factors for presenting policymaking solutions to reduce CHEs for the households of cancer patients, referred to Shahid Rahimi Hospital in Khorramabad, as the main public center for cancer patients in Lorestan Province, Iran.
3. Methods
3.1. Study Setting
This study was conducted in Khorramabad, located in western Iran, with 18 public hospitals and five private medical centers. Shahid Rahimi Educational and Medical Center, as a referral hospital for cancer patients, was selected as the research environment. There are wards in this center designated to cancer diagnosis and treatment.
3.2. Study Design
This hospital-based, cross-sectional study was conducted to investigate the catastrophic expenditures and fairness of financing for cancer treatment.
3.3. Study Population
The statistical population of this study included all households of cancer patients, referred to the radiotherapy and chemotherapy wards of Shahid Rahimi Hospital in June 2017.
3.4. Inclusion Criteria
The inclusion criteria were cancer patients, referred to the radiotherapy or chemotherapy wards of the hospital (or both) in Lorestan Province, Iran.
3.5. Exclusion Criteria
The exclusion criteria were other acute cancer patients, who usually received treatment in other provinces of Iran.
3.6. Sample Size
According to a previous study, 67.9% of cancer patient households faced CHEs [18]. With almost 2,500 registered cancer patients in Lorestan Province, a sample size of 220 was measured at P = 0.679 (q = 1-p = 0.321, error = 0.05) and an accuracy level of e = 0.06 (z = 1.96), based on the following formula:
By visiting the hospital wards, the researchers collected the data through interview, using a simple random sampling method. A face-to-face household interview conducted for each household randomly and each interview lasted about 30 minutes.
3.7. Study Variables
In this study, the dependent variable was household CHE, and the independent variables were characteristics, including the educational level of the household head, sex, age, and other variables, such as type of cancer, insurance type, supplementary insurance coverage, treatment type, utilization of inpatient services, residency and household size.
3.8. Data Collection
In the present study, a WHO questionnaire, called the Global Health Survey, was used to collect data. This questionnaire was developed in 2003 to measure the performance of health systems, based on the three objectives of the health system. This questionnaire was translated into Persian in a previous study (18). The results showed that the translated version had adequate reliability and validity. Generally, it consists of three main parts, including the demographic information, household questionnaire, and individual questionnaire. In the present study, the identification information and household questionnaires were used. The time allowed for recalling information related to the total household expenditures, consumption expenditures, and outpatient treatment expenditures was one month (one year for hospitalized cases). Regarding the socioeconomic status, information was collected on the total expenditure of each household (22, 23).
3.9. Data Analysis
Based on the WHO approach, to determine the CHEs and fair financing of cancer treatment, the income and total household expenditures spent on food and non-food items (e.g., housing, education, transportation, and other expenditures) were determined. In this study, a two-stage method was applied for data analysis. The first step was understanding the household CHEs, and the second step was determining the fairness of financial contributions for cancer treatment expenditures. To estimate the CHEs, food expenditure and household size were converted using the following formula (β = 0.56):
To determine the poverty line (PL), first, the percentage of food expenditure to total expenditure was calculated for each household by dividing the food expenditures to the equivalent household size calculated in the previous step to determine the PL. The average food expenditure of households within the 45th and 55th percentiles was considered as PL. The subsistence expenditures (SEs) were also calculated for each household using the following formula:
The criterion for determining the household status regarding PL is to compare the calculated SEs with the total household expenditures. If the total household expenditures are lower than the SEs, the household is below PL (poor). In the next step, capacity to pay (CTP) was measured using the following formula:
where
In this study, to measure the financial protection of households, the WHO approach was applied. The following formula was used for estimating the fairness of financing for cancer treatment:
Where wh is the household weight
This article is part of a research project (grant No: 95-04-163-29776; ethics code: IR.IUMS.REC1395.95-04-163-29776). The research team would like to thank the financial support of the research deputy, affiliated to Iran University of Medical Sciences, Tehran, Iran.
4. Results
A total of 220 households were included in the study, about 70% of whom were exposed to CHEs. The FFCI was estimated at 0.857 for the study population. The rate of exposure to CHEs was calculated for different educational groups, income levels, age groups, and other independent variables; the results are presented in Table 1.
| Characteristics | Exposure to CHEs | P-Value | |
|---|---|---|---|
| Yes | No | ||
| Sex of the household head | 0.0495 | ||
| Male | 67 (81.63) | 38 (19.36) | |
| Female | 87 (65.75) | 28 (35.24) | |
| Educational level of the household head | 0.0387 | ||
| Illiterate | 36 (67.27) | 74 (32.73) | |
| Primary school | 15 (70) | 35 (30) | |
| Secondary school | 7 (70.83) | 17 (27.16) | |
| Diploma | 5 (82.76) | 24 (17.24) | |
| Academic | 3 (57.14) | 4 (42.86) | |
| Income quintile | < 0.001 | ||
| Quintile 1 | 33 (0.75) | 11 (25) | |
| Quintile 2 | 23 (52.27) | 21 (47.73) | |
| Quintile 3 | 23 (52.27) | 21 (47.73) | |
| Quintile 4 | 32 (72.73) | 12 (27.27) | |
| Quintile 5 | 43 (97.73) | 1 (2.27) | |
| Age of the household head (y) | 0.029 | ||
| < 30 | 41 (85.42) | 7 (14.58) | |
| 30 - 60 | 57 (67.06) | 28 (32.94) | |
| > 60 | 56 (64.37) | 31 (35.63) | |
| Supplementary insurance | 0.493 | ||
| Covered | 8 (54.61) | 5 (46.38) | |
| Not covered | 146 (53.70) | 61 (47.29) | |
| Insurance type | 0.033 | ||
| Relief Foundation | 28 (56) | 22 (44) | |
| Social Security | 64 (01.79) | 17 (99.20) | |
| Health Service | 25 (76.75) | 8 (24.24) | |
| Residence | 0.575 | ||
| Rural areas | 37 (07.66) | 19 (93.33) | |
| Khorramabad | 81 (5.67) | 39 (5.32) | |
| Other cities | 73 (73) | 27 (27) | |
| Treatment type | 0.57 | ||
| Chemotherapy | 108 (79.68) | 49 (21.31) | |
| Radiotherapy | 16 (66.66) | 8 (33.33) | |
| Both | 30 (92.76) | 9 (08.23) | |
| Utilization of inpatient services | 0.0421 | ||
| Yes | 77 (78.77) | 22 (22.22) | |
| No | 77 (64.63) | 44 (36.36) | |
| Type of cancer | 0.12 | ||
| Breast cancer | 30 (17.73) | 11 (83.26) | |
| Gastrointestinal cancer | 53 (23.60) | 35 (77.39) | |
| Liver cancer | 8 (73.72) | 3 (27.27) | |
| Lung cancer | 14 (78.77) | 4 (22.22) | |
| Others | 49 (03.79) | 13 (97.20) | |
| Household size | < 0.001 | ||
| 1 - 3 | 68 (77.95) | 3 (23.4) | |
| 4 - 6 | 77 (6.61) | 48 (4.38) | |
| > 6 | 9 (5.37) | 15 (5.62) | |
aValues are expressed as No. (%).
As shown in Table 1, the rate of exposure to catastrophic expenditures was lower in households whose head had academic education compared to other educational groups. Also, the rate of exposure to CHEs was higher in younger age groups (head of the household), and the difference was statistically significant. Considering the exposure of each household quintile or income level, the percentage of exposure to CHEs was higher in high-income groups compared to low-income groups. Moreover, the results showed that younger household heads were more exposed to CHEs compared to other age groups.
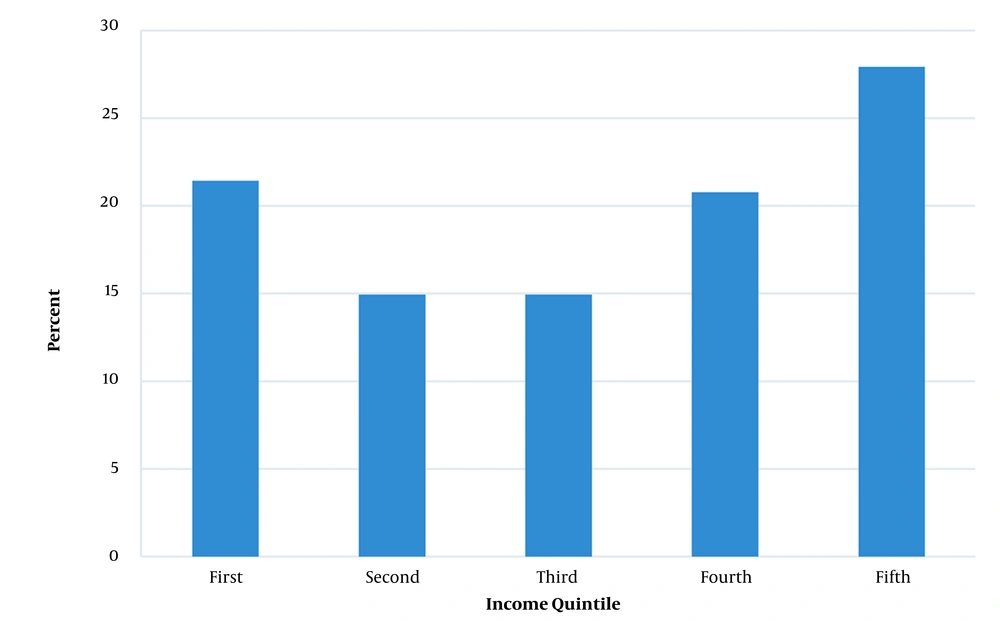
In Figure 1, the distribution of households exposed to CHEs at different income levels (quintiles) is presented. The first quintile is the poorest household, while the fifth quintile is the wealthiest. The highest percentage of households exposed to CHEs was observed in the richest group (the fifth quintile); in other words, 27.92% of households with CHEs belonged to this group.
As shown in Table 1, women-headed households were more likely to face CHEs, and this relationship was statistically significant. Besides, households with supplemental insurance coverage were less exposed to CHEs compared to other households, although this relationship was statistically insignificant. Households living in Khorramabad faced relatively lower catastrophic expenditures compared to households living in other cities; however, the difference was not statistically significant.
The household size had a significant reducing effect on the household CHEs; in other words, by increasing the household size, the likelihood of catastrophic expenditures decreased. The relationship between the incidence of CHEs for households of cancer patients and the type of cancer showed that the financial burden of cancer treatment was high in households with breast and lung cancer patients. Besides, exposure to these expenditures was higher in households with patients receiving chemotherapy and radiotherapy simultaneously as compared to households with patients receiving radiotherapy or chemotherapy separately. In terms of the type of insurance, households covered by social security and medical service companies were more exposed to CHEs compared to households covered by the Relief Foundation and rural insurance companies. Also, inpatient service utilization increased the likelihood of exposure to CHEs.
5. Discussion
In many countries, especially less developed and developing ones, the rate of exposure to CHEs is high for cancer treatment (27). Studies show that CHE is proportionally high in Iran (28). In this study, the number of households facing CHEs and the FFCI were measured as two key indices. The results regarding the financial burden of cancer imposed on patients and their households showed that about 70% of cancer patient households in Lorestan Province were exposed to CHEs, and the FFCI of healthcare financing for the studied households was estimated at 0.857. Nonetheless, the values of these indices vary in previous studies (24, 26).
The incidence of CHEs in the current study was proportionally higher than other similar studies in Iran. In this regard, the results of a study by Kavosi et al. in Shiraz, Iran, indicated that 67.9% of households of cancer patients were exposed to CHEs (18). Moreover, Kasahun et al. found that the incidence of CHE for cancer patient households was about 75% (20). According to general health policies, the FFCI, as a national indicator, must be 0.9 at minimum (26); however, this requirement was not met in our study; in other words, inequity in financing for cancer treatment was significant in the study population. In a similar study, Rezapour et al. (17) reported a lower FFCI (0.68) in Iran. Another study from Kermanshah Province, Iran, measured this index to be 0.57 (29). Consistent with the current study, Murray reported the value of this index to range from 0.74 in Brazil to 0.941 in Slovakia (30). In recent years, although the healthcare system has improved healthcare services, it has not been successful in reaching the goal discussed in upstream documents related to health in iran
Generally, high-cost cancer treatment services can impose a heavy financial burden on households and push them into poverty (31). Therefore, improved protection of patients and their families against financial difficulties is essential, especially for incurable diseases, such as cancer. Regarding the determinants of CHEs for cancer treatment, the current study showed that supplementary health insurance had an insignificant protective effect on CHEs and that the risk of catastrophic expenditures was lower in households with supplementary insurance (61.54%) compared to households without this type of insurance (70.53%). Moreover, Lee and Yoon indicated that the probability of facing CHEs among households without this insurance was higher than those covered by this insurance plan (32). Overall, the success of such plans in preventing CHEs depends on their sufficient coverage or effective definition of cancer care.
The current study revealed that the type of insurance is a significant determinant of exposure to CHEs. Accordingly, the incidence of CHEs was higher in households covered by social security and medical service insurance compared to those covered by the Relief Foundation insurance. Since people with the Relief Committee insurance are normally in the low-income group, they ignore receiving healthcare services due to their low payment capacity. In this regard, a previous study reported inconsistent results with the current study, and the CHEs were found to be higher in people covered by the Relief Foundation insurance because of their lower CTP (18).
Moreover, there was a significant association between the incidence of household CHEs and the type of cancer treatment. The results showed that the rate of exposure to CHEs was higher in households with breast cancer and lung cancer. Patients who received radiotherapy were less likely to be exposed to CHEs compared to patients receiving chemotherapy and radiotherapy simultaneously. In the study by Kavosi et al., it was found that 74.1% of patients undergoing chemotherapy were exposed to CHEs, while the rate of exposure to CHEs was 54.5% in patients undergoing radiotherapy. In line with other studies on household CHEs for cancer treatment (18, 33), a significant relationship was found between catastrophic expenditures and the sex of the household head.
The present study indicated that the rate of exposure to catastrophic expenditures was lower among households whose head had academic education compared to other educational levels; this study confirmed the results of previous studies (34, 35). According to our findings, younger household heads were more exposed to CHEs compared to other age groups. This finding is in line with the results of previous studies (35, 36), as younger household heads often have a lower economic status, which is a good explanation for our findings.
The current study also revealed the positive effect of inpatient service utilization on the exposure of households to CHEs, as inpatient service utilization can increase the use of services provided for patients and consequently, increase the expenditure of medical services. Kavosi et al. (23) and Cruz Rivero et al. (36) also found that increased inpatient service utilization was associated with the frequency of hospitalization and the risk of CHEs. The household size is another factor, which had a negative significant relationship with the possibility of CHEs in the study population; in other words, CHEs decrease by increasing the household size.
The negative impact of increasing the household size on the likelihood of exposure to catastrophic expenditures may be due to the lower expectations of larger households to utilize health services and more attention to health by small-sized households. Finally, the CHEs increase in higher income households, because they allocate a larger share of their CTP to health expenditures. However, poorer households with lower income and payment capacity ignore receiving health services and prefer meeting other needs to health needs; a similar study in China confirmed our finding (37).
This study, similar to other studies, had some limitations. Due to differences in the socioeconomic status, the results of the present study may be only generalizable to other regions of the country. Besides, this study was conducted through interviews and had limitations, such as cost reporting bias and recall bias. Another limitation of the current study was restriction of the FFCI to distinguish between the progressive and regressive trends of the financing system; to resolve this issue, other indices are needed.
5.1. Conclusions
The present results showed that the CHEs were high for cancer treatment. Despite the efforts made so far, the Iranian health system has failed in preventing the catastrophic expenditures of cancer treatment and has not been successful in protecting households from the financial burden. Also, the recent health system transformation plan and health financing system reforms in Iran have not had significant effects on improving this index for these households. Therefore, a large number of households with cancer patients face financial difficulties due to health expenditures. Accordingly, more financial support and effective insurance plans need to be provided for these households, and the health system should not only improve supportive policies by expanding the insurance coverage, but also introduce cancer benefit packages to reduce cancer treatment expenditures.