1. Background
Coronavirus disease 2019 (COVID-19) is an acute respiratory disease introduced as a public health emergency and an international concern by the World Health Organization (WHO) due to its rapid spread. The COVID-19 pandemic was declared in March 2020 (1, 2). According to the WHO, until February 28, 2022, more than 434,154,739 confirmed cases were approved, and 5,944,342 deaths were attributed to this disease worldwide (3). In Iran, a total of 7,040,467 confirmed cases and 136,631 deaths due to COVID-19 were reported (4). This disease has posed major challenges to individuals' physical and mental health due to its rapid spread (5). Healthcare workers (HCWs) who are at the forefront of combating COVID-19 are exposed to an increased risk of infection due to long and uncomfortable work shifts and increased workload to save patients' lives (6). A study from China indicated that in the first stage of the COVID-19 pandemic, infected nurses accounted for 29% of all hospitalized cases with COVID-19 (7). In Iran, at least 40 HCWs died due to COVID-19, and hundreds of them have been hospitalized after the onset of symptoms (5). Evidently, the safety of the HCWs is not only crucial for protecting them against the virus but is also effective in preventing the transmission of the virus (8). Overall, understanding and adopting behaviors, such as using appropriate personal protective equipment, by HCWs is important in COVID-19 prevention (9).
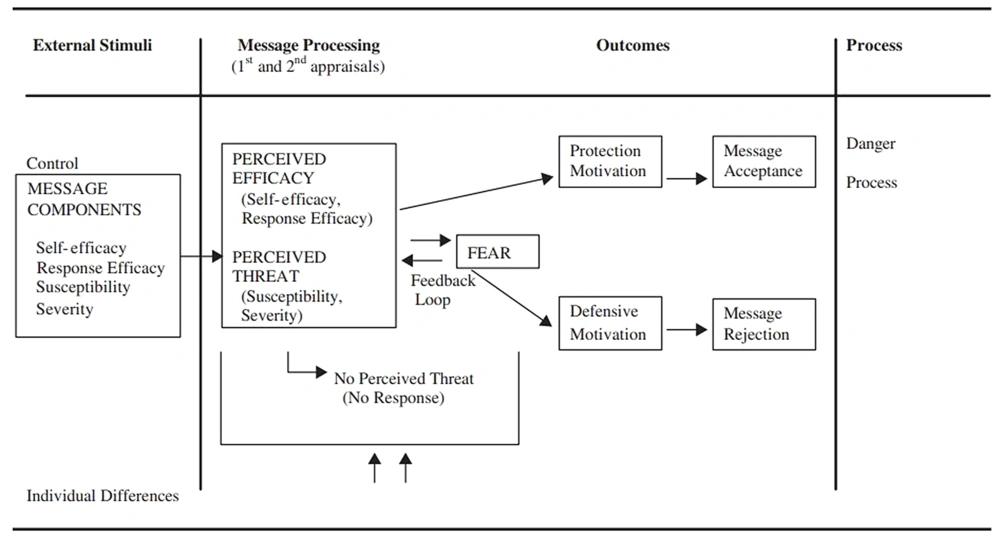
Protective behaviors refer to behaviors that reduce exposure to risk factors, as well as effective actions for the rapid detection and control of the disease, decelerating the spread of disease, receiving timely and appropriate treatment, and minimizing complications (10). The WHO has identified education as one of the most important components of preventive programs. Experts also believe that one of the reasons for the failure of educational programs is the lack of attention to analytical studies and their inability to consider psychosocial models as an intellectual framework for educational planning (9). One of the important theories of health education, which has been applied in various studies to predict protective behaviors, is the extended parallel process model (EPPM) (11). Based on the EPPM, when facing a risk factor or threat, individuals follow one of two pathways based on their perceived self-efficacy and risk analysis: (1) danger control that enables the individual to take preventive actions against risks or exposing factors and (2) fear control that causes the individual to apply a passive mechanism while facing risk and avoid preventive behaviors (12). Performing threat appraisal, followed by assessing perceived self-efficacy and perceived response efficacy, will increase the probability of change in attitude, intention, and behavior (13). The relationships between the constructs of the model are presented in Figure 1 (14).
People's lifestyle in a community concerning emerging diseases requires awareness and a thorough understanding of the disease, adaptation to the disease, increased risk perception, and increased motivation to perform protective behaviors (15). Therefore, to encourage the HCWs to follow COVID-19 health recommendations, it is crucial to understand how they perceive the COVID-19 pandemic, how they assess the risks, and how such assessments may lead them to change their protective behaviors.
2. Objectives
This study was conducted considering the importance of identifying the determinants of COVID-19 preventive behaviors in the HCWs (due to their high vulnerability) in designing and implementing preventive programs. It aimed to predict the protective behaviors of Iranian HCWs toward COVID-19 based on the EPPM.
3. Methods
3.1. Study Design and Population
The current study with a cross-sectional design was conducted online among a convenience sample of 418 Iranian HCWs, including nurses, physicians, HCWs, laboratory technicians, radiologists, and administrative workers, from May 4 to July 22, 2020. The inclusion criteria were the HCWs of all centers affiliated with the Iranian healthcare system, willingness to participate in the study, and access to the Internet for answering the questions of the electronic questionnaire. The exclusion criteria were lack of cooperation in completing questionnaires and incomplete questionnaires.
Data were collected using an electronic questionnaire published on the Porsline website. A general announcement was posted on social media through Telegram, Instagram, and WhatsApp to invite people to participate in the study. Besides, messages were sent to several authorities, including some managers of hospitals and healthcare centers who had access to the HCWs, to share the questionnaire link. The required sample size was 422 individuals, based on the sample size equation (d = 0.05, P = 0.5, and Z = 0.95), with an estimated attrition rate of 10%.
3.2. Theoretical Framework and Measures
The data collection tool in this study was a researcher-made questionnaire, including demographic characteristics with eight questions (e.g., age, sex, marital status, education level, and job experience) and questions related to all constructs of the EPPM (Table 1).
| Constructs | Scoring (Range) | Item Example |
|---|---|---|
| Perceived susceptibility: Individual's perception of his/her vulnerability to COVID-19 | Agree = 3; No idea = 2; Disagree = 1 (1-3) | I am worried that I will be infected with COVID-19. |
| Perceived severity: Individual's perception of the severity of COVID-19 risk | Agree = 3; No idea = 2; Disagree = 1 (1-3) | COVID-19 is a fatal and threatening disease. |
| Perceived self-efficacy: Assurance of the individual about his/her ability to perform COVID-19 protective behaviors | Agree = 3; No idea = 2; Disagree = 1 (1-3) | I can perform COVID-19 protective behaviors every day, such as wearing masks, gloves, or special clothes. |
| Perceived response efficacy: Individual's opinion about the preventive effects of protective behaviors for COVID-19 | Agree = 3; No idea = 2; Disagree = 1 (1-3) | I perform daily protective behaviors, such as wearing masks, gloves, or special clothes. |
| Behavioral intention: A person's perceived likelihood or "subjective probability" that he/she will engage in a given behavior | Agree = 3; No idea = 2; Disagree = 1 (1-3) | I intend to perform protective behaviors until the end of the COVID-19 pandemic, such as wearing masks, gloves, or special clothes. |
| Behavior: Protective behaviors associated with COVID-19 | Never = 1; Rarely = 2; Sometimes = 3; Often = 4; Always = 5 (1-5) | I currently do protective behaviors regularly during my work shift, such as wearing masks, gloves, and special clothes. |
3.3. Validity and Reliability
The content validity of the questionnaire was evaluated by measuring the content validity ratio (CVR) and content validity index (CVI) based on the opinions of 10 experts (experts in health education, health promotion, and communicable diseases). Regarding the total mean score, the CVI was 0.81 (perceived sensitivity, 0.80; perceived severity, 0.80; perceived self-efficacy, 0.84; perceived response efficiency, 0.79; behavioral intention, 0.82; and behavior, 0.81), and the total mean CVR was 0.79 (perceived sensitivity, 0.75; perceived severity, 0.78; perceived self-efficacy, 0.87; perceived response efficiency, 0.76; behavioral intention, 0.81; and behavior, 0.77). Also, the reliability of the questionnaire was evaluated based on internal consistency (Cronbach's alpha coefficient) in a sample of 30 HCWs. The total reliability coefficient for the subscales was 0.70.
3.4. Data Analysis and Crisis Point Determination
Data were analyzed in SPSS version 16 using statistical tests (descriptive tests, independent t-test for mean comparisons, ANOVA test, Pearson's correlation test for mean comparisons in the subgroups, and multiple regression analysis for predicting intention and behavior).
To determine the critical point in the EPPM model, the subtraction of the perceived threat construct (combination of perceived susceptibility and perceived severity) with the perceived efficacy construct (combination of perceived self-efficacy and perceived response-efficacy) was used.
3.5. Ethical Considerations
At the beginning of the questionnaire, the participants were asked their willingness to answer the questions. Completing the questionnaire was voluntary, and informed consent was obtained from the participants after the assessment.
4. Results
A total of 418 respondents were included in the final analysis. The results showed that most participants (40.4%) were 30-40 years old, 72% were married, and the majority were female (70.6%). Also, 49.5% of the participants had a bachelor's degree, and 53.6% of the HCWs had job experience of more than 10 years (Table 2). The relationships between the EPPM constructs and demographic variables are computed and presented in Table 2.
| Variables | No. (%) | Susceptibility | Severity | Self-efficacy | Response-efficacy | Intention | Behavior |
|---|---|---|---|---|---|---|---|
| Age | |||||||
| 20 - 29 | 87 (20.8) | 2.59 ± 0.70 | 2.25 ± 0.89 | 2.52 ± 0.77 | 2.27 ± 0.81 | 2.77 ± 0.49 | 4.03 ± 1.06 |
| 30 - 39 | 169 (40.4) | 2.63 ± 0.67 | 2.31 ± 0.85 | 2.47 ± 0.79 | 2.44 ± 0.76 | 2.79 ± 0.48 | 4.07 ± 1.13 |
| 40 or more | 142 (34.0) | 2.63 ± 0.62 | 2.26 ± 0.86 | 2.66 ± 0.67 | 2.46 ± 0.79 | 2.80 ± 0.50 | 4.16 ± 0.99 |
| P-value | 0.907 | 0.801 | 0.078 | 0.174 | 0.840 | 0.595 | |
| Number of children | |||||||
| No | 154 (36.8) | 2.67 ± 0.64 | 2.26 ± 0.87 | 2.56 ± 0.74 | 2.29 ± 0.80 | 2.83 ± 0.43 | 4.16 ± 1.00 |
| One | 100 (23.9) | 2.64 ± 0.65 | 2.26 ± 0.87 | 2.47 ± 0.79 | 2.45 ± 0.74 | 2.73 ± 0.52 | 4.01 ± 1.05 |
| Two or more | 150 (35.9) | 2.60 ± 0.66 | 2.30 ± 0.86 | 2.60 ± 0.71 | 2.50 ± 0.78 | 2.82 ± 0.47 | 4.04 ± 1.12 |
| P-value | 0.660 | 0.920 | 0.363 | 0.069 | 0.197 | 0.439 | |
| Education status | |||||||
| Associate's degree | 72 (17.2) | 2.56 ± 0.66 | 2.18 ± 0.86 | 2.56 ± 0.72 | 2.38 ± 0.77 | 2.80 ± 0.52 | 4.15 ± 1.07 |
| Bachelor's degree | 207 (49.5) | 2.67 ± 0.62 | 2.23 ± 0.89 | 2.51 ± 0.77 | 2.38 ± 0.82 | 2.77 ± 0.50 | 4.02 ± 1.06 |
| Master's degree or higher | 132 (31.6) | 2.57 ± 0.71 | 2.41 ± 0.82 | 2.64 ± 0.70 | 2.45 ± 0.74 | 2.81 ± 0.47 | 4.18 ± 1.06 |
| P-value | 0.291 | 0.093 | 0.282 | 0.722 | 0.753 | 0.341 | |
| Economic status | |||||||
| Poor | 42 (10.0) | 2.61 ± 0.69 | 2.61 ± 0.69 | 2.30 ± 0.89 | 2.23 ± 0.84 | 2.78 ± 0.47 | 3.71 ± 1.13 |
| Not good, not bad | 278 (66.5) | 2.63 ± 0.64 | 2.30 ± 0.86 | 2.57 ± 0.72 | 2.38 ± 0.78 | 2.79 ± 0.50 | 4.15 ± 1.04 |
| Good | 98 (23.4) | 2.62 ± 0.68 | 2.07 ± 0.89 | 2.65 ± 0.70 | 2.53 ± 0.74 | 2.80 ± 0.46 | 4.11 ± 1.07 |
| P-value | 0.975 | 0.002* | 0.041* | 0.105 | 0.962 | 0.044* | |
| Occupational status | |||||||
| Nurse | 133 (31.8) | 2.63 ± 0.67 | 2.36 ± 0.83 | 2.51 ± 0.79 | 2.30 ± 0.83 | 2.80 ± 0.46 | 4.24 ± 0.93 |
| Health worker | 171 (40.9) | 2.66 ± 0.63 | 2.22 ± 0.86 | 2.54 ± 0.75 | 2.50 ± 0.73 | 2.78 ± 0.50 | 3.96 ± 1.12 |
| Physician | 29 (6.9) | 2.58 ± 0.73 | 2.24 ± 0.95 | 2.55 ± 0.73 | 2.10 ± 0.85 | 2.79 ± 0.49 | 4.17 ± 1.10 |
| Laboratory technician and radiologist | 32 (7.7) | 2.71 ± 0.58 | 2.18 ± 0.93 | 2.71 ± 0.63 | 2.37 ± 0.83 | 2.96 ± 0.17 | 4.31 ± 0.78 |
| Administrative staff | 52 (12.4) | 2.51 ± 0.67 | 2.34 ± 0.86 | 2.65 ± 0.65 | 2.51 ± 0.69 | 2.69 ± 0.64 | 4.00 ± 1.26 |
| P-value | 0.633 | 0.611 | 0.580 | 0.039* | 0.178 | 0.140 | |
| Work experience | |||||||
| 1 - 5 years | 106 (25.4) | 2.61 ± 0.69 | 2.21 ± 0.92 | 2.47 ± 0.81 | 2.28 ± 0.78 | 2.80 ± 0.46 | 3.98 ± 1.04 |
| 6 - 10 years | 80 (19.1) | 2.67 ± 0.66 | 2.36 ± 0.76 | 2.51 ± 0.74 | 2.40 ± 0.78 | 2.73 ± 0.56 | 4.10 ± 1.12 |
| 10 or more | 224 (53.6) | 2.64 ± 0.63 | 2.28 ± 0.87 | 2.62 ± 0.70 | 2.45 ± 0.78 | 2.82 ± 0.45 | 4.14 ± 1.04 |
| P-value | 0.747 | 0.526 | 0.173 | 0.164 | 0.412 | 0.413 | |
| Gender | |||||||
| Male | 123 (29.4) | 2.58 ± 0.71 | 2.34 ± 0.84 | 2.44 ± 0.081 | 2.34 ± 0.81 | 2.76 ± 0.51 | 3.93 ± 1.08 |
| Female | 295 (70.6) | 2.65 ± 0.63 | 2.26 ± 0.87 | 2.61 ± 0.70 | 2.43 ± 0.77 | 2.80 ± 0.48 | 4.16 ± 1.05 |
| P-value | 0.277 | 0.382 | 0.037* | 0.286 | 0.434 | 0.043* | |
| Marital status | |||||||
| Single | 117 (28.0) | 2.64 ± 0.65 | 2.25 ± 0.87 | 2.58 ± 0.75 | 2.43 ± 0.79 | 2.79 ± 0.49 | 4.08 ± 1.06 |
| Married | 301 (72.0) | 2.59 ± 0.68 | 2.35 ± 0.84 | 2.58 ± 0.72 | 2.33 ± 0.77 | 2.79 ± 0.50 | 4.13 ± 1.06 |
| P-value | 0.530 | 0.269 | 0.772 | 0.232 | 0.988 | 0.665 |
a Values are expressed as mean ± SD unless otherwise indicated.
According to the findings, there was a significant association between financial status and the EPPM constructs of perceived severity (P = 0.002), perceived self-efficacy (P = 0.041), and behavior (P = 0.044), between occupation and perceived response efficacy (P = 0.039), and between sex and perceived self-efficacy (P = 0.037) and behavior (P = 0.043). No significant association was observed between other demographic variables and the constructs of EPPM. Pearson's correlation test was used to assess the association between the constructs of EPPM. There was a significant association between the constructs of perceived susceptibility and perceived severity (r = 0.286, P = 0.000), perceived self-efficacy and perceived response efficacy (r = 0.237, P = 0.000), perceived self-efficacy and intention (r = 0.225, P = 0.000), intention and perceived response efficacy (r = 0.147, P = 0.003), and protective behaviors for COVID-19 and perceived self-efficacy constructs (r = 0.373, P = 0.000), perceived response efficacy (r = 0.120, P = 0.014), and intention (r = 0.462, P = 0.000). All of these associations were positive (Table 3).
| Susceptibility | Severity | Self-efficacy | Response-efficacy | Intention | Behavior | |
|---|---|---|---|---|---|---|
| Susceptibility | ||||||
| Pearson correlation | ||||||
| P-value | ||||||
| Severity | ||||||
| Pearson correlation | 0.281** | |||||
| P-value | 0.000 | |||||
| Self-efficacy | ||||||
| Pearson correlation | -0.020 | -0.019 | ||||
| P-value | 0.686 | 0.694 | ||||
| Response efficacy | ||||||
| Pearson correlation | 0.031 | 0.034 | 0.237** | |||
| P-value | 0.533 | 0.492 | 0.000 | |||
| Intention | ||||||
| Pearson correlation | 0.083 | 0.025 | 0.225** | 0.147** | ||
| P-value | 0.090 | 0.610 | 0.000 | 0.003 | ||
| Behavior | ||||||
| Pearson correlation | 0.080 | 0.023 | 0.373** | 0.120* | 0.462** | |
| P-value | 0.102 | 0.632 | 0.000 | 0.014 | 0.000 |
a ** P-value = 0.01, * P-value = 0.05
In the first phase of the multiple regression analysis, to predict intention using the EPPM constructs, among the constructs of perceived susceptibility, perceived severity, perceived self-efficacy, and perceived response efficacy in the model, two constructs of perceived self-efficacy (P = 0.000) and perceived response efficacy (P = 0.043) were predictors of intention; these variables explained 6% of the total variance in intention. Also, with a one standard deviation increase in the perceived self-efficacy score and perceived response efficacy, the intention score increased by 0.20 and 0.10, respectively (Table 4).
| Dependent Variables | Predictor Variables | B | SE | Beta | T | P | R | R2 | ADJ.R2 |
|---|---|---|---|---|---|---|---|---|---|
| Intention | Constant | 2.300 | 0.101 | - | 22.880 | 0.000 | 0.245 | 0.060 | 0.055 |
| Self-efficacy | 0.134 | 0.033 | 0.201 | 4.108 | 0.000 | ||||
| Response efficacy | 0.063 | 0.031 | 0.100 | 2.032 | 0.043 | ||||
| Behavior | Constant | 0.666 | 0.271 | - | 2.456 | 0.014 | 0.538 | 0.289 | 0.286 |
| Intention | 0.856 | 0.091 | 0.398 | 9.370 | 0.000 | ||||
| Self-efficacy | 0.405 | 0.61 | 0.283 | 6.572 | 0.000 |
In the second phase of the multiple regression analysis, to predict protective behaviors based on the constructs of EPPM, it was found that among the constructs of perceived susceptibility, perceived severity, perceived self-efficacy, and intention in the model, two variables of perceived self-efficacy (P = 0.000) and intention (P = 0.000) were predictors of protective behaviors; these variables explained 28% of the total behavioral variance. Therefore, with one standard deviation increase in the scores of intention and perceived self-efficacy, the behavior score increased by 39.0 and 28.0, respectively (Table 4).
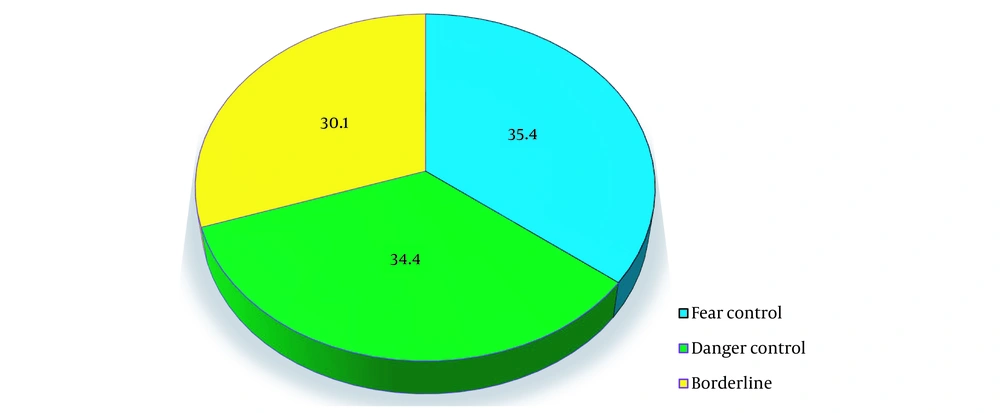
Moreover, the results of descriptive analysis for determining the critical point in the EPPM showed that 148 (35.4%) HCWs with a critical point < 1, who were in the process of fear control, were probably not performing protective behaviors; 144 (34.4%) HCWs with a critical point >1, who were in the danger control process, were probably performing protective behaviors; and 126 (30.1%) HCWs with a critical point of zero were indifferent to protective behaviors of COVID-19 and were considered borderline (Figure 2).
5. Discussion
This study aimed to determine the protective behaviors for COVID-19 among Iranian HCWs, based on a psychological theoretical framework of EPPM. In the current study, only 47.8% of the HCWs regularly performed protective behaviors against COVID-19 (e.g., wearing a mask, gloves, and special clothes), while the rest were undesirable. Therefore, according to the recommendations of the WHO, regular use of masks and gloves is essential in all therapeutic procedures during the COVID-19 pandemic (16). According to the present findings, in the first stage of the COVID-19 pandemic, infected nurses comprised 29% of all patients (7). In other studies, protective behaviors against diseases and injuries related to the work environment were undesirable among workers (e.g., nurses and physicians) and students in health and treatment sections (17, 18); these findings are consistent with the results of the current study. However, some studies reported inconsistent results with the present study findings. In this regard, a study by Rajoura et al. showed that 82.6% of physicians and 85% of Indian nurses wore masks during the epidemic of H1N1 influenza in their work environment (19).
Moreover, a study by Shirahmadi et al. revealed that more than 70% of the participants performed the recommended behaviors against COVID-19 (20). Consolo et al. reported inconsistent results with the current findings (21). The cause of the discrepancy between the present study and other studies or reasons for undesirable protective behaviors in the current study may be the lack of people's awareness, non-adherence to long-term use of protective tools, interference of protective behaviors with other tasks, waste of time, high level of fatigue, limited understanding of the importance of adherence to health and protective principles, and limitations in access to protective facilities and equipment in Iran. Subsequently, to promote the level of awareness, attitude, and performance of the HCWs, interventions seem necessary, such as regular monitoring of the HCWs' adherence to protective principles and appropriate and effective training for this vulnerable group; also, authorities and managers need to pay particular attention to meet the requirements.
According to the results of the present study, to determine the critical point based on the EPPM, almost 35.4% of the HCWs were in the fear control process (defensive avoidance, oppositeness, and disagreement), 30.1% were indifferent to protective behaviors for preventing COVID-19, and only 34.4% of the HCWs faced COVID-19 in the danger control process (changes in attitude, intention, and behavior). In other words, the HCWs did not show desirable coping appraisal and preventive behaviors. In contrast, perceived susceptibility, perceived severity, and overall perceived threat were almost adequate. Generally, the critical point is a key concept in EPPM. It refers to when an individual, despite a high perceived threat, realizes that he/she does not have the ability to prevent the occurrence of a significant threat, such as COVID-19, due to reasons, such as the assumed inefficacy of the recommended approach, costly or time-consuming ways of combating the risk or problem, or low perceived self-efficacy; therefore, the process of fear control overcomes the process of danger control (13). The current study results align with the findings of studies based on the EPPM on health topics, behaviors, and hazards (15, 20, 22). In a study by Rimal and Real assessing the EPPM constructs, it was found that individuals with high perceived risk and high perceived efficacy showed more self-protective behaviors than those who were inactive, indifferent, or avoidant (23). The HCWs are expected to experience the highest threat and efficacy and are involved in the process of danger control. Also, according to the results, the feelings of fear and threat associated with the mental pressure of COVID-19 have become excessive among the HCWs in Iran, similar to almost all countries worldwide. Therefore, it is essential to design more precise programs to promote workers' self-efficacy for performing protective behaviors and emphasize the efficacy of recommended practices and approaches. Also, alarming messages can be posted about the risks of COVID-19 in retraining programs for workers to promote their protective behaviors; this final recommendation is based on the comments of White et al., claiming that messages with strong fear appeal and high efficacy cause more behavioral changes, while messages with strong fear appeal and low efficacy create more defensive responses (13). Based on the multiple regression analysis results in this study, perceived self-efficacy was a predictor of self-protective behaviors. The predictive potential of perceived self-efficacy suggests that promoting workers' confidence in the importance of self-protective behaviors can be effective in COVID-19 prevention under all circumstances. In other studies, perceived self-efficacy was also an important predictive factor for behavior (16, 24, 25). Overall, reducing the HCWs' work shifts, resolving their physical and mental fatigue, incorporating a new auxiliary workforce in the health system, teaching relaxation techniques, and using motivating approaches can be effective strategies for promoting individuals' self-efficacy.
In addition to the perceived self-efficacy in this study, the construct of intent also predicted protective behavior in employees. Self-efficacy and response efficiency also predicted the intention to perform protective behavior in employees. This means that to have a greater risk perception of COVID-19, self-efficacy and higher perceived intent are likely to be required, and these perceptions will have a positive effect on the perception of COVID-19 and, thus, the protective behavior of employees. Therefore, if employees feel that they can protect themselves against the disease by themselves and think these measures are effective in preventing COVID-19, the intention and motivation to perform protective behaviors will increase. In fact, it is the intention of a conscious plan or decision to act and try to perform a behavior. These results are consistent with the findings of other studies (9, 26, 27).
Besides, interventions must concentrate on training to improve the individuals' perceptions regarding the efficacy of protective behaviors and provide better technical and protective facilities and equipment in hospitals and medical centers.
5.1. Strengths and Limitations
The strength of this study was the use of an online sampling method through the Porsline website to collect data; this facilitated the well-timed collection of a broad spectrum of HCWs in Iran. Other data collection methods were uncertain and difficult for researchers or patients in the acute phase of COVID-19. On the other hand, a limitation of this study was the self-report assessment of behavior; unavoidably, such studies can produce bias and false information.
5.2. Conclusions
Only one-third of the HCWs contributed to the process of COVID-19 danger control. The HCWs' motivation for protection against COVID-19 depended on their perception of self-efficacy and their perceived efficacy of COVID-19 preventive behaviors. The present results can be used to design and implement training programs to improve the protective behaviors of the HCWs.