1. Introduction
Coronavirus disease 2019 (COVID-19) originated in Wuhan city, China, in December 2019 and spread rapidly around the world (1). In March 2020, the World Health Organization (WHO) declared COVID-19 a global pandemic, and the world emergency committee reported the need for early diagnosis, isolation, and prompt treatment (2). As of May 29, 2022, over 526 million confirmed cases and over 6 million deaths were reported to WHO in 188 countries and territories (3). The virus is transmitted by exposure to infectious respiratory fluids produced when an infected person coughs, sneezes, or talks. Instead of remaining in the air for a prolonged duration, these droplets usually drop onto the ground or surface (4). Individuals can get the infection by touching contaminated things or directly touching the mouth, nose, or eyes. The results showed that respiratory droplets containing coronavirus that fall onto the surface become a thin microscopic layer after the evaporation of water and can remain infectious for days on surfaces (5). The virus quantity reduces until it is insufficient for infection. Nevertheless, it might be observed for hours or days. The virus is very contagious in the first 3 - 4 days following the initiation of symptoms. However, the virus may spread prior to the appearance of symptoms, resulting in later disease (6). On January 23, 2020, Wuhan and other cities in Hubei imposed a lockdown for the whole month, and the government suspended travel in Wuhan and imposed other restrictions (7). Similar control measures have been taken in 15 cities in Hubei, China, since January 24, 2020 (8). Million people left Wuhan before the coronavirus lockdown began in various parts of the world and China (9). This led to the spread of the new coronavirus in many parts of the world. Better strategies for controlling the COVID-19 pandemic worldwide were to shoot down various activities in stages or all at once. China was the first country to start a partial closure. After China, COVID-19 became highly prevalent in Italy. As of March 9, 2020, the COVID-19 pandemic has moved to an almost nationwide holiday in Italy (10). It was followed by Iran, where the closure occurred on March 14, 2020 (11). At the closing of March 2020, most individuals worldwide were obliged to cease nearly all commercial, economic, and social activities. India began a shutdown after a long hiatus but underwent an identical phase (12). The first confirmed COVID-19 case in India was announced on January 30, 2020, in Kerala’s Thrissur region, where a student was coming back home from Wuhan University in China had a positive coronavirus test. Three Indians from Kerala tested positive for COVID-19 after returning to India from Wuhan on February 3, 2020. However, in March 2020, the number of daily new coronavirus cases increased dramatically, and in the third week, more than 550 cases had tested positive for COVID-19 which led to the nationwide lockdown on March 25, 2020 (13). This global shutdown had a key role in improving air quality; however, numerous investigations reported severe damage caused by the COVID-19 pandemic for cities with the worst air quality (14). According to epidemiological studies, ambient air pollution is directly related to mortality and various diseases, including cardiovascular and respiratory defects. In a study performed in Shiraz, cardiovascular and respiratory mortalities caused by air contaminants were predicted as 628 and 182 cases in 2016 and 370 and 82 cases in 2017, respectively. Sulfur dioxide (SO2) had the highest total mortality of 4.3% in 2016, but this percentage decreased in 2017 to 0.42% (15). The results of a study conducted by Bonyadi et al. (16) showed that the number of extra hospital admission due to asthma (HAAD) for less than 15 years and 15 - 64 years by air pollutants in Shiraz were estimated as 273 and 36 in 2016 and 243 and 30 cases in 2017, respectively. The results revealed that air pollutants caused respiratory problems in Shiraz city. Recent studies have shown that worse air quality also increases severe acute respiratory syndrome coronavirus 2 (SARS) mortality (17) and the incidence of influenza (18). In laboratory conditions, van Dormallen et al. (19) showed the long shelf life of SARS-CoV-2 in airborne particles, which could be an important source of COVID-19 transmission. The relationship between COVID-19 and climate change is very vague compared to air pollution. Evidence that may link climate to COVID-19 is the use of meteorological factors, such as temperature, relative humidity (RH), absolute humidity (AH), and wind speed (WS) (20). Several studies were published worldwide to determine the global effects of the COVID-19 lockdown on the environment. Rodo et al. (21) recently studied climate change and the COVID-19 epidemic. They stated that AH and temperature were associated with influenza outbreaks and facilitated epidemic progression. SARS-CoV-2 appears to have a higher survival rate and transmission rate than the influenza virus in tropical regions.
2. Objectives
This study reviewed the effects of air pollution, climate parameters, and lockdown on the number of cases and mortality related to COVID-19. Specifically, we attempted to assess the correlation between the COVID-19 lockdown and air pollutants emissions (NO, SO2, CO, O3, PM2.5, and PM10).
3. Methods
The present review was performed to determine the effects of weather and air pollution on the number of cases and deaths related to COVID-19 during the lockdown. Through searching existing online university databases, such as PubMed, Science Direct, and Google Scholar, articles were collected with no limitations on publication dates. Afterwards, this review focused on outdoor air pollution (including PM2.5, PM10, NO2, SO2, and O3) and weather conditions affecting SARS-CoV-2/COVID-19. MeSH and keywords, such as "PM" and "SARS-CoV-2/COVID-19", "air pollution" and "SARS-CoV-2/COVID-19", "O3", and "SARS-CoV-2/COVID-19", "NO2" and "SARS-CoV-2/COVID-19", "SO2" and "SARS-CoV-2/COVID-19", "CO" and "SARS-CoV-2/COVID-19", "humidity" and "SARS-CoV-2/COVID-19", "temperature" and " SARS-CoV-2/COVID-19", "rainwater" and "SARS-CoV-2/COVID-19", "wind speed" and "SARS-CoV-2"/COVID-19", "lockdown" and "SARS-CoV-2/COVID-19", "lockdown" and "air pollution", "SARS-CoV-2/COVID-19" and "climate" OR "weather" were used. An initial keyword search retrieved 886 studies on January 24, 2021. After limiting the language to "English" and the document type to "article", 465 papers remained for analysis. Subsequently, 367 more publications were excluded after being completely read and evaluated as they did not provide enough information or the results were not sufficiently in line with our review. A total of 98 studies were obtained for inclusion in the present review after a full-text review.
4. Results
The study findings are presented in five sections: COVID-19 in ambient air, the effect of pollutants on the number of COVID-19 cases and mortality, the effect of different climate parameters on the number of COVID-19 cases and mortality, the effect of COVID-19 lockdown on the atmospheric pollutants, and indirect impacts of COVID-19 on the environment.
4.1. COVID-19 in Ambient Air
4.1.1. Aerosol Particles Produced by Coughing and Sneezing in SARS-CoV-2 (COVID-19)
It was observed that coronavirus caused three significant concerns in terms of survival and transmission as an air pollutant. When the virus becomes suspended in smaller droplets, known as aerosols, it can stay suspended for three hours in the air, but it would drift down much sooner under most conditions. Other factors, such as the size of the respiratory droplets and the activities that cause the virus to spread in the environment, were not considered when it was announced that keeping a distance of 1 m from others could prevent the spread of coronavirus (22). Therefore, a group of researchers reviewed the published studies in this field and evaluated the extent of coronavirus spread under different conditions. They concluded that the COVID-19 virus could be transmitted with respiratory droplets up to 8 m away in just a few seconds after sneezing, coughing, and talking. Many environmental factors transmit SARS-CoV-2 in the air (23). The infectious dose required for COVID-19 infection is unknown. Surgical masks and eye protection are needed at a distance of 2 m from the patient because of the possibility of droplet exposure and are recommended when exposed to a single cough or sneeze from a virus carrier nearby. Sneezing and coughing create clouds of liquid aerosol particles in the air, mainly in the range of 1 - 100 micrometers (24, 25). Particles of diverse sizes have significantly different dynamic properties. Relatively large droplets precipitate within 1 m due to the attraction of gravity. Many studies have shown that particle size can significantly affect dynamic properties. Due to the gravitational attraction force, relatively large droplets precipitate within 1 m. Smaller particles can travel long distances (26). Zayas et al. found high concentrations of submicron particles in cough aerosols (27). In some articles, the total concentration of aerosol particles (integrated into all sizes) is 10-3 - 2.10-3 cm3 (22). The particle size range was 1 - 10 μm, and 50% of particles had a diameter of less than 5 μm. However, when ejected from an infected person, some droplets may or may not be directly associated with coughing but with the background aerosol. The COVID-19 infection risk due to droplet concentrations for speech and coughing was estimated to be in the ranges of 2.4 - 5.2 and 0.004 - 0.223 cm3, respectively (28). According to the literature, numerous inconsistencies were reported in the particle number and size distribution of different respiratory behaviors, including speaking, singing, coughing, and sneezing. Most data demonstrate that cough droplets generated by infected humans span an extensive range of sizes from smaller than 1 μm to more than 100 μm. Particles larger than 1 μm and smaller than 10 μm in diameter are part of the PM10 characteristic. For example, they seem to suspend (minutes to hours) or travel more than 6 feet in the air. The larger particles are potentially more infectious than the small particles (on average 1000 times greater). Therefore, viral load is higher in bigger particles than in smaller ones (19).
4.1.2. Could Air Pollution Efficiently Carry and Transmit SARS-COV-2
The available data also indicated that PM and gaseous pollutants operate as carriers or transport vectors in COVID-19 through several routes. COVID-19 mortality might increase through air pollution rise via its function in related diseases (29). Recent experimental studies support the hypothesis that the immune response is decreased through exposure to air pollution for a short time at higher levels. Animal and human investigations demonstrated that the increase in mucosal permeability and oxidative stress, decreased antioxidants and antimicrobial surfactant proteins, and the destruction of macrophage phagocytosis results from exposure to air pollutants in the laboratory. Nevertheless, it is required to investigate further the relationship between air pollutants and SARS-CoV-2 in ambient air, especially their effects on human health (30). Given the link between air pollution and COVID-19, for the reduction of air pollution, it is required to concentrate on the primary sources of emissions, including the utilization of fossil fuels in road traffic and heat generation. Experimental studies have shown that the virus is bound to be an air pollutant. However, it is not yet confirmed whether coronavirus can survive on the surface of suspended particles. The preliminary findings of this study indicated a high probability for viruses to create clusters with PM in atmospheric stability and high concentrations of particulate matter (31). Another study by the University of Bologna, the oldest university in the world, and the University of Trieste collected PM10 from Bergamo, northern Italy, with the highest number of registered COVID-19 cases. A high concentration of PM is also a characteristic of this region. The evidence obtained until April 12, 2020, demonstrated that approximately 30% of COVID-19-positive cases were Lombardy residents in Italy. The mentioned investigation studied 34 PM10 samples collected by air sampling from an industrial area in Bergamo for three weeks, from February 21 to March 13. This study indicated that several SARS-CoV-2 samples were positive (32). Various parameters, such as air pollutants, relative humidity, temperature, wind speed, and rainwater, affect the transmission of SARS-CoV-2 (33).
4.2. Effect of Pollutants on the Number of COVID-19 Cases and Mortality
Various studies worldwide were also found to understand the effect of various air pollution parameters on COVID-19 mortality and morbidity (Table 1).
| Parameter and Country | Change in Pollution Parameter | Impact |
|---|---|---|
| PM | ||
| United States (14) | 1 μg/m3 increase in PM2.5 | 8% increase in COVID-19 death rate |
| United States (806 counties) (34) | 10 μg/m3 increase in PM2.5 | Number of daily confirmed cases increases by 9.41% for PM2.5 and by 2.42% (95% CI: 1.56%-3.28%) for O3 |
| Italy (107 Italian territorial areas) (35) | Increase of 1 μg/m3 PM2.5 | 9% increase in the average COVID-19 mortality rate |
| Varese, northern Italy (36) | PM2.5 | 5.1% increase in the rate of COVID-19 |
| Italy (71 provinces) (37) | Chronic exposure to atmospheric PM2.5 and PM10 | Desirable for severe acute respiratory syndrome coronavirus two infection spread |
| Middle East countries (38) | Increased concentrations of PM2.5 and PM10 indoors | Facilitates the transmission of the COVID-19 virus by droplets and aerosols in an indoor environment |
| Italy (north) (39) | Daily limit value PM10 | Significant increase in the number of cases |
| United States (California) (40) | PM10 | Significant correlation with the COVID-19 epidemic |
| NO2 | ||
| 66 Regions in Germany, Spain, Italy, and France (41) | Highest NO2 concentration with downward air | Out of 4443 mortalities, 3487 (78%) were in northern Italy and central Spain |
| China (120 cities) (33) | 10 μg/m3 increase in NO2 | 6.94% increase in the daily number of confirmed patients |
| United States (California) (40) | NO2 | Significant correlation with the COVID-19 epidemic |
| SO2 | ||
| China (120 cities) (33) | 10 μg/m3 increase in SO2 | 7.79% reduction in the daily number of confirmed cases |
| Romania (Bucharest) (42) | SO2 | Directly correlated with the daily COVID-19 incidence and mortality |
| United States (California) (40) | SO2 | Significant correlation with the COVID-19 epidemic |
| CO | ||
| China (120 cities) (33) | 10 μg/m3 increase in CO | 15.11% increase in the daily number of confirmed patients |
| Romania (Bucharest) (42) | CO | Directly correlated with the daily COVID-19 incidence and mortality |
| United States (California) (40) | CO | Significant correlation with the COVID-19 epidemic |
| O3 | ||
| China (120 cities) (33) | 10 μg/m3 increase in O3 | 4.76% increase in the daily number of confirmed patients |
| United States (806 counties) (34) | 10 μg/m3 increase in O3 | The number of daily confirmed cases increases by 2.42% (95% CI: 1.56% - 3.28%) for O3 |
4.2.1. Particulate Matter (PM)
As demonstrated in laboratory studies, there is a possibility of interaction and alteration of viral activity for PM and viruses on account of their composition. Moreover, PM has been identified as a carrier of microorganisms, such as SARS-CoV-2 (43). Regarding the effect of PM and the prevalence of viruses, some COVID-19 studies in several countries have recently identified whether the different regions of the world were associated with higher and faster increases in COVID-19 transmission with a higher level of air pollution. The coronavirus has infected many individuals in three parts of the world. The origin of COVID-19 was in Wuhan, China. Very high levels of air pollutants have been shown in Italy, the USA, and Iran (14, 37, 44). Recent investigations have focused on the regions mentioned above to determine a significant correlation between air pollution variables and COVID-19 contagions. Based on the evidence from the USA for determining air pollution exposure and COVID-19 death rate, there was an association between an increase of only 1 μg/m3 in PM2.5 and 95% CI with an 8% rise in the COVID-19 mortality rate. For this study, the number of COVID-19 deaths for more than 3,000 cities in the United States (representing 98% of the population) up to April 22, 2020, was collected from the Johns Hopkins University, Center for Systems Science and Engineering Coronavirus Resource Center (14). In Italian regions, during the last four years, Fattorini and Regoli (37) concluded that air pollutants (e.g., PM2.5, PM10, nitrogen dioxide, and ozone) have a higher distribution than regulatory boundaries. Another study demonstrated that the association between air pollution and COVID-19 was also noticed in rural regions, indicating that air pollution, considered separately from an urban setting with all its features (e.g., density or congestion), has a direct role in COVID-19. In rural areas, ammonia released from urea and other fertilizers reacts rapidly with nitrogen dioxide (NO2) and SO2 to form a particulate matter (PM2.5) (Table 1).
4.2.2. Gases Pollutant
Air pollutants, such as NO2, ozone, SO2, carbon monoxide (CO), and methane (CH4), can be measured by satellite instruments (45). These instruments calculate the solar spectrum from ultraviolet to near-infrared. Advanced recovery algorithms are applied to convert the measured radiation to column pollutant concentrations (e.g., a troposphere column density of NO2. The Aura satellite was launched by the National Aeronautics and Space Administration on July 15, 2004, and equipped with the ozone monitoring instrument to monitor global air pollution in numerous regions of the world (14). Recently, a large study conducted in the United States showed a significant association between prolonged exposure to NO2 and COVID-19 mortality (27). In addition, another research in the UK demonstrated that COVID-19 mortality and morbidity had positive associations with SO2 and NO2 levels recorded in 2018 - 2019 and had a negative correlation with O3 (46). Another investigation on the effects of SO2, CO, NO2, and O3 on COVID-19 mortality demonstrated that a 10 μg/m3 increase in NO2 and O3 was associated with 6.94% (95% CI: 2.38 - 11.51) and 4.76% (95% CI: 1.99 - 7.52) rise in the daily number of COVID-19 confirmed patients, respectively. There was also an association between a 1 μg/m3 increase in CO and a 15.11% (95% CI: 0.44 - 29.77) rise in the daily number of COVID-19-confirmed patients. Moreover, a negative correlation was observed between SO2 levels and COVID-19 morbidity and mortality. As a result, a 7.79% decrease (95% CI: -14.57 to -1.01) in the confirmed cases of COVID-19 was related to an augmentation of 10 μg/m3 in the SO2 concentration (33).
4.3. Effect of Different Climate Parameters on the Number of COVID-19 Cases and Mortality
This section investigates the influential parameters of climate change on the airborne transmission of SARS-CoV-2. Table 2 summarizes the effect of different climate parameters on the number of COVID-19 cases and mortality.
| Parameter and Country | Relationships and Results |
|---|---|
| 1. Temperature | |
| China (10 affected provinces) (47) | An asymmetric relationship between temperature and COVID-19, with several slightly positive, slightly negative, and some mixed trends |
| Bangladesh (48) | 1°C increase in temperature associated with a 36.1% (P < 0.01) increase in the rate of COVID-19 infection |
| Spain (49) | No proven evidence for a relationship between temperature and cumulative items within a temperature range of 3.19°C - 29.26°C |
| India (50) | A significant positive association between COVID-19 cases in Rajasthan (25°C - 25°C) and Kashmir (10°C - 32°C) was found. However, there is no significant association between temperature and COVID-19 in Maharashtra (29°C - 38°C) |
| Brazil (51) | With each 1°C increase in temperature, there was a reduction in the number of daily COVID-19 patients by 4.9% in temperatures below 25.8°C (range: 27.4°C - 16.8°C) |
| China (52) | Temperature significantly affected COVID-19 incidence within the range of 22°C - 26°C. There was an increase in temperature with a decrease in infection rate (RR = 0.96; 95% CI: 0.93 - 0.99) |
| Italy (53) | An increase in the average daily temperature by 1°F led to a reduction in the number of cases by about 6.4 cases/day |
| Iran (44) | No significant relationship between temperature and COVID-19 |
| Indonesia (Jakarta) (54) | The number of COVID-19 cases was associated with the temperature |
| China (55) | Lower and higher temperatures might be positively associated with reducing the risk of COVID-19 spread |
| 2. Humidity | |
| Australia (56) | There was a significant negative association between relative humidity and COVID-19 patients (P = 0.0304); accordingly, there was an association between every 1% reduction in morning humidity and an increase of 6.11% in cases |
| China (all provincial capitals) (57) | An association between an increase of 1 g/m3 in absolute humidity and a decrease in the number of daily confirmed patients |
| Malaysia (Kuala Lumpur) (58) | The data analyzed by Spearman's correlation test showed a positive correlation between COVID-19 cases and relative humidity (r = 0.106, P = 0.001) |
| Global (166 countries except China) (urban) (59) | A negative association between relative humidity and daily cases. Each 1% increase in relative humidity resulted in 0.85% (95% CI: 0.51 - 1.19%) decrease in daily new cases |
| Turkey (60) | An increase in relative humidity leads to a decrease in the number of daily cases |
| 3. Rainfall | |
| United States (61) | A negative correlation between rainfall and COVID-19 transmission |
| Italy (53) | An increase in COVID-19 transmission due to rainfall. An increase of 56.01 in COVID-19 cases/day was reported on account of each average rainfall per inch/day |
| Bangladesh (48) | Rainfall (P < 0.01) was significantly associated with the COVID-19 pandemic |
| Indonesia (Jakarta) (54) | Rainfall was not significantly associated with COVID-19 |
| 4. Wind speed | |
| United States (61) | Wind speed had a significant role in the virus spread |
| Bangladesh (48) | A significant association between wind speed and COVID-19 (P < 0.03) |
| Malaysia (58) | No significant correlation between wind speed and the number of COVID-19-confirmed patients (r = -0.059; P > 0.01) |
| South America (62) | Wind speed had no significant relationship with daily cases |
| Turkey (60) | High wind speed was significantly correlated with an increase in the COVID-19 cases |
| 5. Solar radiation | |
| China (63) | Solar radiation does not reduce the transmission of COVID-19; however, although ultraviolet light from the sun can kill the flu virus |
| Malaysia (58) | No significant relationship between solar radiation and COVID-19 cases |
4.3.1. Temperature
The optimum environmental temperature associated with the SARS outbreak in Hong Kong, Guangzhou, Beijing, and Taiyuan was 16°C - 28°C. In addition, Bi et al. (64) showed an inverse correlation between temperature and SARS transmission in Hong Kong and Beijing in 2003. A laboratory study using alternative viruses to investigate the effect of temperature on coronavirus survival on environmental surfaces showed the rapid inactivation of viruses at 20°C instead of 4°C (65). Another laboratory study revealed that the virus was more stable on smooth surfaces for about 5 days at 22°C - 25°C and relative humidity of 40% - 50% (66). Furthermore, van Doremalen et al. (67) noticed the lower stability of Middle East respiratory syndrome coronavirus at high temperatures/humidity. Overall, most investigations demonstrated an optimum temperature for the coronavirus. Moreover, high environmental temperatures can harm virus viability. A study in New York, the United States, reported a significant association between ambient temperature (average and minimum) and confirmed COVID-19 cases (68).
4.3.2. Humidity
Based on a study by Chan et al. (66) at a temperature of 22°C - 25°C and relative humidity of 40% - 50%, the dried SARS-CoV-2 can survive up to five days on a smooth surface. However, SARS-CoV-2 survival decreased with higher humidity and temperature. Therefore, the evidence has demonstrated the better stability of SARS-CoV at low a temperature and low relative humidity. Moreover, the evidence shows rapid moisture evaporation in the exhaled bioaerosols at low relative humidity, forming droplet nuclei that remain in the air for extended periods, increasing the likelihood of transmitting the pathogenic virus (69). Relative humidity can affect the evaporation and dispersion of exhaled breathing droplets. Droplet nuclei formation can substantially increase the viruses, possibly remaining infectious in aerosols for hours. Many studies have shown that humidity has a primary role in COVID-19 spread. Research conducted in New York found no significant relationship between COVID-19 cases and the average humidity (68).
4.3.3. Rainfall
Few studies show an association between COVID-19 and rainfall. A significant negative correlation between rainfall and COVID-19 spread was reported based on the evidence in the USA (68). On the other hand, some studies have shown 56 cases/day increase for each inch of average rainfall per day (53). The evidence shows no relationship between rainfall and the number of COVID-19 patients in Iran (44).
4.3.4. Wind Speed
Wind has also been shown as another critical factor in COVID-19 transmission. Virus spread is hard to control in windy weather. The COVID-19 virus can be transmitted dependent on the wind intensity and direction. There is evidence that it can be transmitted to large areas with high population density, and virus spread increases in cases where the wind speed is high. In places where the wind blows at a speed of 30 km/h or more, there is a higher risk of SARS-CoV-2 transmission in the case of a high-density population. In this case, traffic restrictions must be considered depending on the wind speed. The virus spreads so much on windy days. As a result, traffic raises the risk of SARS-CoV-2 transmission (70). A study in the United States found that wind speed played a small role in spreading the COVID-19 virus (68). A study in Iran revealed that low wind speed has a statistically significant association with the number of COVID-19 cases (44).
4.3.5. Solar Radiation
There are limited investigations on the association between COVID-19 and solar radiation. A study conducted during the SARS epidemic in Iran showed that solar radiation is a threat to the survival of the virus. Areas that received more solar radiation showed a higher infection exposure rate (44).
4.3.6. Aerosol Optical Depth (AOD)
Aerosol optical depth (AOD) was used to monitor and measure the charge of suspended particles in the atmosphere during the lockdown. Southeast Asian countries have shown an increase in AOD values (about 0.5 - 0.7) (71). On the other hand, a significant reduction in AOD (∼40%) in western and northern India during COVID-19 was observed. The average AOD rose slightly in Iran from March 21 to April 21, 2020 (72). A significant decrease in AOD (20% - 60%) was reported in the Hindu gantry basin (7).
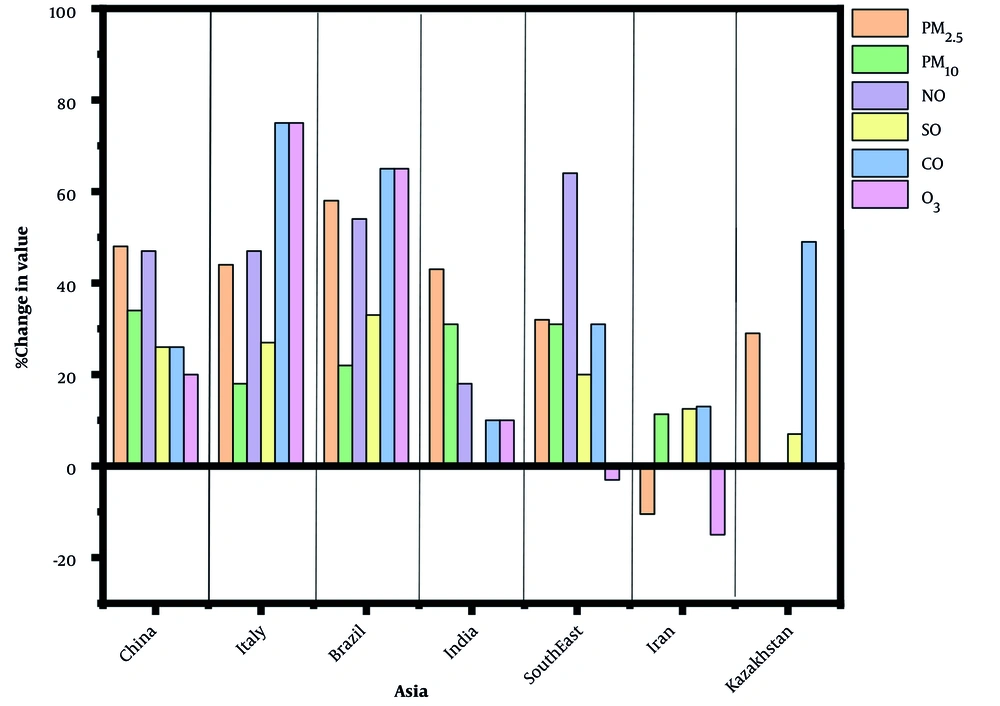
4.4. Effect of COVID-19 Lockdown on Air Quality
The severe contagious COVID-19 led to lockdowns across the world. The COVID-19 lockdown and travel restrictions dramatically reduced the emission of key air pollutants, primarily carbon, throughout the world. It has been an unprecedented situation in the emission of air pollutants during the COVID-19 pandemic in the world compared to previous decades (73). Some of the salient impacts of the COVID-19 lockdown on air quality are shown in Figure 1. Note that the effects of lockdown on NO2, which has an atmospheric lifespan of about one day, are locally detectable, while the impacts of lockdown on O3, with a lifespan of several weeks, are under the influence of transport associated with specific climate patterns (74). Restrictions imposed during the COVID-19 pandemic in 30 major Turkish cities, where most of the Turkish population lives, significantly improved the air quality. Assuming that some actions taken during the epidemic period become permanent over time (such as increasing home-based businesses, reducing air travel thanks to online meetings, making extensive use of distance learning, changing consumption habits, and reducing waste), it is expected that the epidemic period will be a turning point in increasing global air quality (75).
4.5. Association Between COVID-19 and Air Pollution
The evidence showed an indirect (negative/positive) effect of pollutants on COVID-19 primarily associated with inhibitory actions on individuals and implemented by various authorities around the world (Table 3).
| Country | Covered Area | Air Pollution | Rate of Change and Impact |
|---|---|---|---|
| United States (14) | 3000 places | PM2.5 | An 8% increase in COVID-19 mortality rate results from an increase of 1 mg/m3 in PM2.5 |
| United States (40) | California | PM2.5, PM10, SO2, NO2, Pb, VOC, CO | PM2.5, PM10, SO2, NO2, and CO had significant associations with COVID-19 |
| East Asia (76) | BTH, Wuhan, Seoul, and Tokyo | NO2, HCHO, SO2, CO, AOD | The highest decreases in pollutants emission were reported in Wuhan, with reductions of about 83%, 11%, 71%, 4%, and 62% in the column densities of NO2, HCHO, SO2, CO, and AOD, respectively. NO2, CO, and formaldehyde concentrations in metropolitan regions, namely Seoul and Tokyo, reduced in comparison to those of the last year; however, the concentration of SO2 rose in the aforementioned two regions on account of the transportation effect of polluted windbreaks. |
| China (33) | 120 cities | PM2.5, PM10, NO2, O3 | An increase of 10 μg/m3 in all the listed pollutants resulted in a rise of 2.24%, 1.76%, 6.94%, and 4.76% in the daily number of confirmed COVID-19 patients, respectively. |
| China (77) | 49 cities | PM2.5, PM10 | Exposure to PM10 and PM2.5 increased the COVID-19 death rate by 0.24% and 0.26%, respectively. |
| China (78) | 219 cities | Air quality index (AQI) | Air pollution positively affects COVID-19 transmission and infection. |
| China (79) | 33 regions | Air quality index (AQI) | A direct association was observed between AQI and COVID-19-confirmed patients. |
| Pakistan (80) | Islamabad, Karachi, Peshawar, and Lahore | PM2.5 | PM2.5 and some weather factors were positively associated with the incidence of COVID-19 in Pakistan |
| Italy (37) | 71 provinces | NO2, O3, PM2.5, PM10 | Significant associations were observed between COVID-19 cases and chronic exposure to PM2.5 and PM10. |
| Italy (81) | Milan | PM2.5, PM10 | New cases of COVID-19 were positively associated with PM2.5 and PM10. |
| Italy (82) | The northern provinces of Italy | NO2, PM10 | There was no significant increase in the number of cases with the permissible concentration of PM10 levels, while high levels of NO2 were associated with the release of COVID-19 |
| Bangladesh (83) | Dhaka | PM2.5, PM10, NO2, SO2, CO, O3 | Overall, 26%, 20.4%, 17.5%, 9.7%, and 8.8% decline in PM2.5, NO2, SO2, O3, and CO concentrations |
| Korea (84) | The seven largest cities and nine provinces | PM2.5, PM10, O3, NO2, SO2, CO | A significant correlation was observed between the incidence of COVID-19 and NO2, SO2, and CO in South Korea. |
| England (85) | All over the country | NO2, O3, PM2.5, PM10 | Air quality was significantly associated with COVID-19 infection and mortality. |
| Netherlands (86) | 355 Municipality | PM2.5, PM10 | An increase of 1 µg/m3 in PM2.5 concentration led to 9.4 higher COVID-19 cases, 3.0 higher hospital admissions, and 2.3 higher mortality. |
| France (87) | Paris, Lyon, Marseille | PM2.5, PM10 | The evidence shows that certain factors increase the probability of a disease outbreak. |
| Malaysia (58) | Kuala Lumpur | PM2.5, PM10, SO2, NO2, CO, O3 | Spearman’s correlation showed that COVID-19 cases had a significant positive relationship with the contaminants (PM10, SO2, NO2, CO, PM2.5, and O3) |
| New York (88) | New York State | O3 | Short-term exposure to ozone possibly affects COVID-19 transmission and disease onset; however, disease aggravation and mortality are dependent on other factors. |
| Mexico (89) | Mexico City | PM2.5 | There was a significant positive correlation between PM2.5 exposure and the probability of death from 19 COVID |
| United States (90) | Southern California | PM2.5, NO2, and O3 | Long-term exposures to ambient air pollutants (PM2.5, NO2, and O3) may contribute to the higher risk of COVID-19 infection. |
5. Discussion
Generally, the COVID-19 pandemic positively affects the environment/climate globally (91). The daily reduction in global CO2 emissions was estimated at 17% (92). In China, a reduction in the utilization of coal (50%) and oil (20% - 30%) resulted in a 25% decrease in CO2, equal to 6% of greenhouse gas emissions (93). The PM2.5 emission decreased by 35%, 29%, and 19% in Wuhan, Hubei (Wuhan excluded), and China (Hubei excluded), respectively (94). Reductions in CO (49%) and NO2 (35%) concentrations were observed in Almaty, Kazakhstan (95). During the lockdown, NO2 concentration declined by 62% and 50% in Madrid and Barcelona (Spain), respectively (96). In the United States, the concentration of NO2 decreased by about 25% during the COVID-19 pandemic compared to 2017 - 2019 (40). A statistically significant reduction was found in the concentration of CO and NO2 in Rio de Janeiro (97). In Morocco, on 2 March 2020, the concentrations of PM10 (75%), SO2 (49%), and NO2 (96%) decreased (98). Several countries/cities, namely China (33), India (99), and the United States (40), have reported reduced NO2 levels over the COVID-19 pandemic. It has been observed that control measures during the COVID-19 pandemic have reduced NO2 emissions, and thus, air quality improved. A decline in CO levels during the COVID-19 pandemic was observed in several countries/cities, including southern and central India (99). In Amman, an overall reduction was observed in NO2 in 2020 by around 27% and 48% compared to 2019 and 2021, respectively. In addition, a slight decrease in CO (around 1%) was recorded in 2020 and 2021 compared to the same period in 2019 (100). Several researchers have recently reported that a slight increase in O3 was observed in some cities compared to NO2 during the lockdown. These results can be attributed to a compound combination of reactions involving volatile organic compounds (VOCs) and nitrogen oxides (NOx). Vehicles also lead to high concentrations of NOx emissions. These conditions are associated with low VOC/NOx ratios. In this case, reducing NOx concentration may result in O3 formation through mechanisms of photochemical reactions. In contrast, in rural regions with a rather high VOC/NOx ratio, O3 production is associated with the distribution of NOx emissions (71). Significant changes in other important pollutants (e.g., SO2, CO, O3, and VOCs) were reported in various countries during the lockdown. According to one of the first studies in China, the concentrations of SO2, CO, and VOC decreased by 16% - 26%, 21% - 26%, and 27% - 57%, respectively. A minor increase in the O3 layer by 20.5% was observed simultaneously with the COVID-19 pandemic (101). It was reported that SO2 and CO concentrations reduced by 33% - 38% and 36% - 65%, respectively, while an increase in O3 level by 30% was observed in Sao Paulo (102). Another study in China showed that air pollution levels decreased significantly during the epidemic. Human factors had no significant effect on O3 concentration. However, they significantly affected PM, SO2, NO2, and CO (103). The impact of movement control order during the COVID-19 pandemic due to the increase of ambient PM2.5 and PM10 concentrations was reported by Mohd Nadzir et al. (104) in Kota Damansara, Malaysia (2020). They reported rises in the ambient concentrations of PM2.5 and PM10 by 60% and 9.7%, respectively. In another study conducted in Milan, Italy, PM2.5 and PM10 decreased by 26% - 48% and 13.1%-18.9% resulting from the initial outbreak of COVID-19 and its associated lockdown. In addition, black carbon (BC) concentration had a significant decline of 71% - 57% (105). A study conducted in São Paulo, Brazil, observed substantial reductions in the mean concentration of PM2.5 and PM10 up to 20% and 30%, depending on the site (102). A study by Chauhan and Singh showed that PM2.5 levels in the world's largest cities reduced by 11%-58% (106). Other studies have shown a reduction in PM2.5 concentrations in Asian (e.g., India and China) and European (e.g., Spain, France, and Italy) countries (107). In another study conducted in 22 cities in India, 43% and 31% showed a decrease in PM2.5 and PM10, respectively (99). An investigation was carried out in 120 cities in China to assess the direct relationship between exposure to high concentrations of particulate matter (i.e., PM2.5 and PM10) and an augmentation in the death rate due to COVID-19. The results of the study, as mentioned earlier, demonstrated that a 10 μg/m3 increase in PM2.5 and PM10 results in an increase of 2.24% (95% CI: 1.02 - 3.46) and 1.76% (95% CI: 0.89 - 2.63) in the daily number of confirmed patients, respectively (33). Global studies have shown that weather parameters (e.g., temperature, relative humidity, wind speed, visibility, and solar radiation) significantly affect COVID-19 cases and fatalities. In Malaysia (Kuala Lumpur) (58), a significant inverse association was shown between ambient temperature and COVID-19 cases. Based on the evidence in Turkey, as the temperature decreases each day, the number of COVID-19 cases per day rises (60). According to research in China, temperature could be considered an environmental trigger for the COVID-19 outbreak in China. The incidence of COVID-19 could decrease with low and high temperatures (57). In Iran, a study showed that humidity has a negative relationship with the rate of virus spread; however, in two humid regions of Iran, the rate of virus spread was high (44). In Australia (56), a significant negative association was reported between relative humidity and COVID-19 patients. There was an association between each 1% reduction in morning humidity and an increase of 6.11% in cases. Based on the evidence in Turkey, the highest correlation was observed between the average wind speed in 14 days and the number of patients. The number of COVID-19 cases augmented with the increase in wind speed. The results showed the most logical time interval as 14 days, indicating that the wind speed in 14 days should be regarded as the correct correlation of case transmission (60). In many studies, there was a significant association between wind speed and COVID (48, 61), but in some other investigations, no correlation was revealed (58, 62). A study was performed on the impact of lockdowns on air pollution and found that CO, SO2, and benzene concentrations reduced due to lockdown by 55% - 55%, 20% - 27%, and 48% - 68%, respectively. Unlike other pollutants, the ozone concentration increased by about 50% (105). One of the first studies conducted (January to March 2020) in China on the impacts of the COVID-19 lockdown on air pollution showed that the concentration of PM2.5 and PM10 declined by 48% - 48% and 34% - 39%, respectively (101). A study on PM10 in rock mines in eastern India observed a 73% - 78% reduction in PM10 concentration before and after the lockdown (108). In Italy, CO and O3 decreased to 75%. This slight air quality improvement is primarily caused by reduced human activities, as COVID-19 lockdowns have reduced ~50% of human activities, measured by traffic volume (37). In many countries, significant changes were observed in reducing the emission of CO, O3, and PM2.5 during the lockdown (78, 95, 101, 102). Adverse climate conditions (e.g., lower wind speed, higher air humidity, higher air pressure, and lower air temperature) can help reduce air pollution, thereby having a significant effect (98). Previous studies have shown that patients affected by SARS are about 84% more likely to die if they live in a highly infected area over time (17). Most of the available data showed that COVID-19 infections and mortality rates were higher in highly infected areas than elsewhere. On the other hand, due to lockdown strategies, air pollution has decreased in some parts of India and China (109, 110). Therefore, maintaining air quality is an important and effective approach to preventing the transmission of COVID-19. A decline in economic activities over the pandemic would assist in reducing global warming and air and sea pollution. Another positive impact is protecting the environment through the EU's recovery plan, the “next-generation EU”, at a minimum of 25% of EU expenditure will play a part in climate action during 2021-2027 (111).
5.1. Conclusions
It has been shown that SARS-CoV-2 is highly contagious if infected individuals cough, sneeze, and talk. The virus can survive for a considerable period and travel long distances without losing its ability to survive and spread, thus, posing a significant threat to human health. There is no evidence of the transmission of viruses in the air for minutes to hours or survival on the surface of suspended particles. However, the marker genes of SARS-CoV-2 in particulate matter samples were positive. According to the literature, COVID-19 daily new cases and mortality had positive associations with particulate matter and the criteria of air pollutants. In meteorology, there are negative correlations between several parameters, such as temperature and humidity (e.g., solar radiation is regarded as a threat to coronavirus). The lowest number of cases was observed at higher temperatures and humidity. Our study demonstrated that rainfall is not associated with COVID-19 new daily cases. Wind speed was directly related to the number of confirmed COVID-19 cases in a worldwide investigation. Solar radiation is a threat to coronavirus. We concluded that the lockdown had significant effects on air quality. A significant reduction was observed in the concentrations of PM10, PM2.5, BC, NOx, SO2, CO, and other gaseous pollutants in every monitored area. Overall, in environmental perspective-based COVID-19 studies, efforts should be accelerated regarding effective policies for reducing human emissions, bringing about air pollution and climate change. Therefore, using clean and renewable energy sources will increase public health and environmental quality by improving global air quality.