1. Background
Patient safety means protecting the patient from any injury during health care (1). Brennan et al. has indicated that adverse events occurred in 3.7% of the hospitalizations, among which 27.6% were due to negligence (2). A patients fall is considered as the most prevailing patient-safety problem in hospitals. However, the rate of falls varies depending on the type of hospital (3). Several reports have indicated that 2% - 15% of patients have experienced a fall during their hospital stay, 15% resulted in serious injuries (4, 5), which not only entails prolonged hospital stays and higher costs, however, it may also result in sustained injuries and even death (6). It is estimated that fall related injuries could be attributed to approximately $15000 and by 2020, the total number of related injury is estimated to reach $58.27 billion among Americans on an annual basis (7).
However, falling is one of the most frequent events in the hospital and is defined as an accidental and unexpected shift in the body posture, which may result in injuries (8); yet, statistics have shown that 78% of in-hospital falls are avoidable (9). Different intrinsic and extrinsic factors have been identified to be contributing to falls in hospital such as the patient’s clinical condition, medication, as well as extrinsic factors such as lack of proper maintenance and design of medical equipment, failures in communication, education, and team working (10).
Several mechanisms have been incorporated to reduce patient falls. Faults have been traditionally interpreted as a failure on the part of individual providers. However, nowadays, the responsibility of medical faults has shifted towards the system. Thus, it is necessary for the hospitals to assess the adverse incidents leading to unexpected injuries to patients and developing preventive action plans (11). This study investigated the contributing factors of fall incidents to determine the share attributed to each factor for developing preventive strategies.
2. Methods
The present study was conducted in a multi-phases qualitative method, in a 600-bed hospital in Tehran, during a 9-month period within 2015. The process of analyzing the root causes was conducted in compliance with the modified protocol of National Patient Safety Agency (NPSA) (12). Data collection process for each case of fall incident was implemented as below:
2.1. Incident Identification
Data on the fall was collected through voluntary error-reporting system. In addition, daily round of raters and interviewing all discharged patients during their stays in hospital was performed in parallel over the course of study.
2.2. Data Collection
Following identification of all individuals involved in the fall incident, the necessary information was extracted by interviewing the personnel and fallers (an interview guide is shown in the additional file). Data including age, sex, Morse fall scale, place and time of fall, the patient’s activity during fall, medications, and environmental factors were collected. The patients’ clinical condition after the fall and the type and severity of injury were rated by physicians in five levels ranging from no injury to death (13). In order to identify high-risk patients, all patients were assessed by two supplementary scales, namely Stratify and Handritch, in addition to Morse scale.
2.3. Developing a Summary of the Fall Incident
At this phase, the timeline of the incident was prepared using findings of last sections. Multiple sessions were held in the cases of sentinel events resulting in death or serious injury caused by inpatient fall.
2.4. Recognizing Challenges
Identifying problems related to falls were performed after data gathering. These problems consist of all errors that take place during a patients’ fall such as failure to monitor, observation. The question ‘why’ was asked repeatedly until the root of the cause of fall was identified. Factors that may have contributed to this rooted cause were also noted. This phase was conducted by two researchers, well-versed with error analysis. The root causes were determined separately by two raters. In case of consensus between two raters, the share of that attributed factor in the fall incidents was accepted. However, in case of divergent scores by two raters, a third rater was consulted.
2.5. Preparing a Fall Incident Report
In this phase, a report of the fall incident was prepared in which the root causes were identified and recorded.
2.6. Operational Plan Development
Nominal group technique (NGT) was used in this phase. The group consisted of 12 hospital experts who were selected based on their expertise and experience including physicians (Neurologist, Orthopaedic, Cardiologist, Anaesthesiologist, General Medicine), nurses, hospital directors, and a number of scientific advisors in the field of patient safety.
At first panel, the root causes of fall incidents, analyzed in previous stages, were provided. Then, the members were asked to draft their suggested strategies without any limitation. Thence, all suggestions were considered, and similar ones were merged together. Finally, a list comprised of 29 strategies was concluded to be discussed in the next meeting.
In the second round, the list was disposed to the expert team members, and they were asked to rate the priority order of interventions according to the importance and feasibility of implementation in form of the Likert scale. After the initial rating, the principal investigator entered all of the raw data into the software program, and numeral difference was controlled by the assistant researcher. The results of analysis were made available and presented to the members at the subsequent meeting, in which the cases with the consensus less than 70% were discussed in details by the members. In the third round, the members were asked to rerate the interventions to remove interventions with consensus less than 70%. Those interventions with a consensus of greater than 70% were considered on the agenda of implementation, which would be run in form of a clinical trial.
2.7. Data Analysis
Data on root causes was collected and analyzed by SPSS 15 Software. Statistical methods were used in this study including descriptive tests in NGT phase, Pearson test, and ANOVA to investigate the relationship between attributed factors and other variables.
3. Results
3.1. Characteristics of Fallers
The average age of patients was 53.7 years (SD = 18.44, range = 17 - 89), and the average length of stay was calculated 12.44 days (SD = 11.74, range = 1 - 63).
A total of 55% of falling incidents occurred among women, and 17% of fallers had a history of previous falls in the past preceding 3 months. The majority of fallers were reported to suffer from cardiovascular diseases and cancer (Table 1).
| Diagnosis | No. (%) |
|---|---|
| Cardiovascular | 24 (22) |
| Cancer | 16 (15) |
| Urologic | 13 (12) |
| Neurodegenerative | 11 (10) |
| Cerebrovascular | 9 (8) |
| Respiratory | 5 (5) |
| Gastrointestinal | 5 (5) |
| Osteoarticular | 4 (4) |
| Gynecology | 3 (3) |
| Others disease | 24 (22) |
Main Diagnosis Fallers at Hospital
3.2. Fall Reports
Among the fall incidents, 80% (90 cases) have resulted in minor to major injuries, of which 57% (63 cases) were patients diagnosed as high risk by Morse risk assessment scale (Table 3). In this study, patients were assessed by two supplementary tools (Handrixh and Stratify tools) in addition to Mores tool, so that 70% of patients were identified as high risk (Table 2).
Gap and Correlation Between Fall Reporting by Nurses and Assessors
A total of 67% of falls occurred when the patient was alone. Out of total falls, 60% of the actual fall incidents were reported by nurses, of which 86% resulted in minor to major injuries. Based on Pearson test, a significant relationship was found between the severity of injury and the fall incident reports by nurses (Table 3).
Activity restriction had been prescribed by a physician in almost 16% of fallers. The analysis of ANOVA test revealed no significant association between the level of activity prescribed by the physician and scores of the Mores tool (F = 0.75, DF = 109, P value = 0.4).
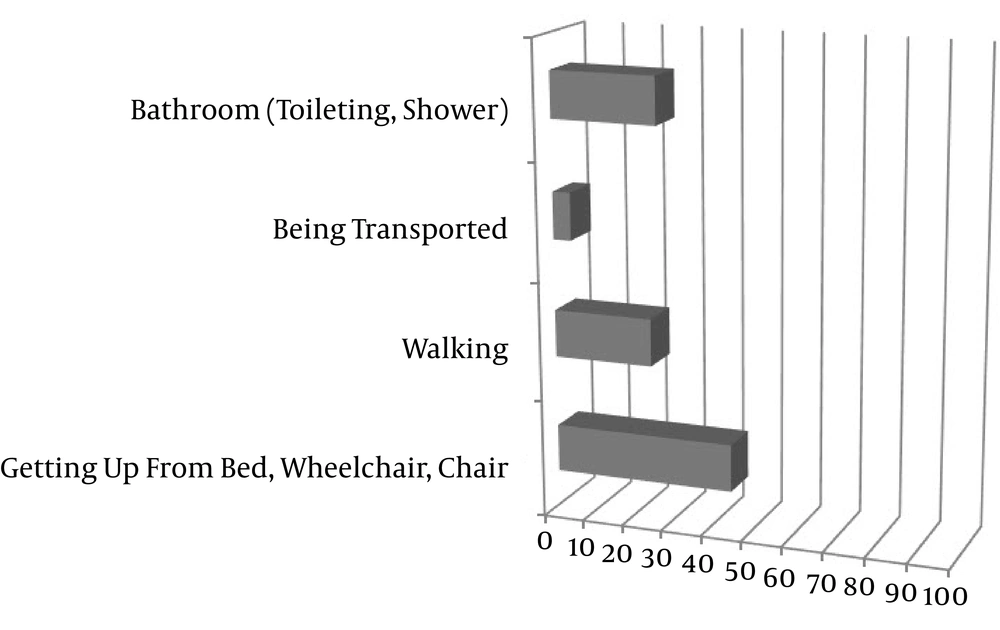
Patient’s activities before or at the time of fall are presented in Figure 1.
3.3. Root Causes of Falls
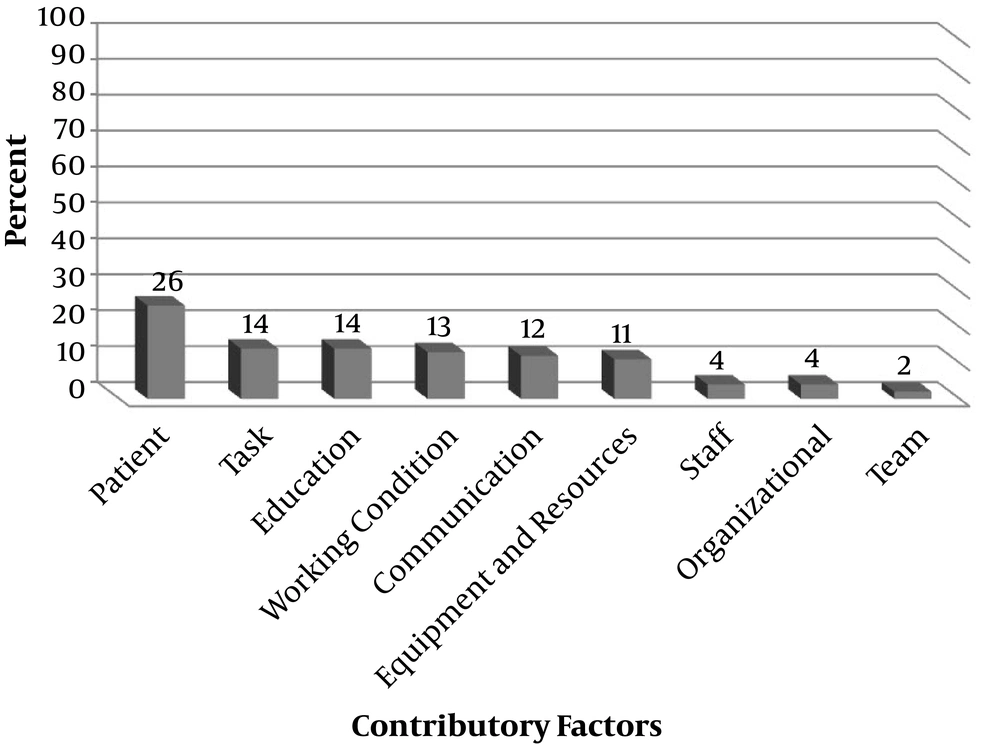
A total of 657 root causes were identified, which forms 5.9 causes for each fall. Root causes identified for inpatient fall and the resulting injuries were representing weakness in 9 related domains (Figure 2). The contribution and the details of factors are illustrated in Figure 3.
3.4. Developing Preventive Strategies
Following the expert meetings held, preventive interventions including physical exercises, examination of visual impairment, keeping floor surfaces dry, placing high risk patients near the nurse’s station, using non-skid slippers, toilet scheduling, and the patient’s justification on not to bathe without assistance obtained consensus less than 70%, therefore, they were discussed in details in the second panels (Table 4).
| Category | Ranking | |
|---|---|---|
| Importance | Possibility | |
| Environment | ||
| Proper lighting | 100 | 92 |
| Toilet floor dry | 84 | 100 |
| Keep pathway clear | 100 | 91 |
| Embedding wall side rail in corridor | 100 | 94 |
| Walking aids | ||
| Safe footwear | 100 | 88 |
| Enough number of walking aids | 97 | 92 |
| Care of plan | ||
| Pain management | 94 | 72 |
| Management of delirium | 89 | 72 |
| Management of hypoxia | 100 | 89 |
| Toileting schedule | 69 | 52 |
| Medication | ||
| Intake vitamin D | 91 | 56 |
| Medication adjustment | 94 | 86 |
| Communication | ||
| Placement of a alert sign | 94 | 94 |
| Yellow wristband | 89 | 94 |
| Bed alarm system | 100 | 92 |
| Equipment | ||
| Bed pressure sensor, hip protector | 83 | 51 |
| Placing the bed rails raised and low bed | 100 | 81 |
| Patient participant | ||
| Do not leave patients unattended | 94 | 69 |
| Encourage patients to empty their bladder prior to bedtime | 83 | 72 |
| Encouragement of patients not to leave a bed or chair without assistance | 100 | 94 |
| Encouragement of use of eyeglasses, hearing aids, footwear | 100 | 93 |
| Nursing supervision | ||
| Placing high risk patients near station | 86 | 58 |
| Increase frequency of patient rounds | 100 | 75 |
| Safety in transfer and handoff | 100 | 92 |
| Assessment of patient | ||
| Reassessing of patients after a fall | 97 | 86 |
| Refer to physiotherapist | ||
| Exercise program | 64 | 65 |
| Refer to optometrist | ||
| Treatment of visual impairment | 86 | 66 |
| Training | ||
| Patient education | 100 | 92 |
| Staff education | 100 | 94 |
Ranking Score of Fall Interventiona
4. Discussion
4.1. Characteristics of Fallers
Based on the findings, the inpatient falls seem to be resulted as a combination of patient-related factors and extrinsic factors. Various literatures have studied the impact of age and sex on the possibility of fall. Ganz et al. and Hendrich reported that the age singly may not be effective on the fall (14, 15). However, other studies have verified the effect of age (16, 17). In the meanwhile, fall incidents in men were lower than women. In contrast to what concluded in our study, Hendrich claimed a higher rate of fall incidents among men due to their incompliance with the instructions (15). Chen and Dunlop concluded that women, particularly following delivery, are more susceptible to fall incident (18, 19). Similarly, there is a consensus that the effect of age and sex can strengthen other contributing factors.
The study demonstrates a higher rate of fall incidents among patients with cardiovascular diseases. Some other studies have confirmed the effect of OH and hypertension in falling incidents (20, 21). Patients cancer was identified as a risk factor to fall incidents, 40% of fallers were identified at low risk or even no risk. Capone and Spolesra confirmed the higher risk of fall in patients with cancer and have introduced factors such as the level of pain, type of cancer, metastases, and medications as the factors contributing to fall incidents (22, 23). We think that it is critical to develop a specific or supplementary instrument to come with a more precise prediction of fall risk among cancer patients.
4.2. Fall Reports
The results indicate that the primary activities before or during fall included getting up from bed and using the toilet, which is confirmed in another study (24-27). Some interventions, including scheduled toileting and regular round of nurses can be effective (4, 28, 29).
Due to the lack of reporting, approximately half of the falls occurred by nurses, therefore, it seems that a reporting system should be developed that is capable of providing an accurate view of the type, nature, and severity of incidents at a reasonable cost (30, 31).
4.3. Root Causes
A total of 5 domains of top contributing factors were found to play greater roles in fall incidents including patient related factors, task, education, environment, and communications.
Among the attributed factors patient-related factors had the greatest share, which included demographic variables (age, sex), systemic variables (balance, strength, sight, cognition), type of diseases (cardiovascular disorders), clinical conditions (blood pressure, hypoxia, delirium, history of falls), not asking for help to get out of bed, and sedation medications. Therefore, interventions such as moderating visual impairment (32), management of delirium (33), hypoxia (33), and medication adjustment are recommended.
Another factor associated with the risk of falling was task factor. Nurses should provide the patients with training at the time of their admission (34) and reassess the risk of fall in patients after falling or changed situation (13). In addition, the majority of fall incidents, the patients, and their families were not well trained on how to consider fall safety precautions, and the patients prescribed to bed rest were not aware of the scope of their activity restrictions.
Environmental factors included inappropriate facility design of the patient’s room, long distances between bathroom and patient’s bed, lack of adequate lighting at night (35), and failure to communicate implying failure in establishing inter-professional relationships between health care providers as well as relationship with patients (36, 37). Greenberg et al. and Vealey et al. reported the highest rate of communication fault during handoffs or transferring the patient to a new ward (8, 38).
In 49% of fallers, a history of taking sedatives and anti-hypertensive drugs was reported, which correspond to the previous literature (10, 39, 40). For this reason, pharmacological interventions such as caution in prescribing drugs affecting the risk of fall and monitoring, modification of dosages, and the time of taking are recommended.
This study has a few limitations. First, this study was conducted in only one hospital, which may affect the generalizability of the results. Another limitation was the recall bias in case of elderly fallers.
Patient fall is attributable to intrinsic and extrinsic causes. The first and foremost preventive step is an accurate assessment of the patient in terms of clinical conditions and fall contributing factors as well as taking a history of previous falls performed by well trained nurses. Preventive strategies should be selected based on a patient condition and hospital, which is done following a selective and purposeful approach by nurses. With respect to the extrinsic factors, hospitals are suggested to run an environmental analysis and develop amendment plans based on the audit results.