1. Context
During the coronavirus disease 2019 (COVID-19) pandemic, lockdown policies restricted the public's movement and subsequently significantly affected the Pakistani community's daily living activity (1). It led to the disruption in economic and social aspects of life and access to healthcare facilities, which mainly caused fear, anxiety, and no access to emergency medical services (2). In Pakistan, the healthcare system works as a hybrid, government and private sectors are significant pillars of the health system (3).
During the COVID-19 pandemic, different hospitals closed their doors to the public due to the overburden of these hospitals (2). This situation led to anger and developed social evils in society because of difficult access to medical facilities during the pandemic. Because of these events, people have shown their frustration by verbally battering and aggressive behavior toward medical professionals (4).
The public health facilities in Pakistan are facing a shortage of medical accessories and equipment, such as personal protective equipment (PPE), including face masks, gowns, and respirators (5). The reason for this shortage is either lack of funds or supply chain disruptions. Healthcare workers (HCWs) should protect themselves from the infection by adopting safeguards measures, which helps to prevent the infection transmission to their families and patients (6). This virus has spread quietly from person to person without symptoms, and the protection of HCWs in this situation is highly important because they are an important stakeholder in the health system (7).
As the number of hospitalization increased, the workload on the healthcare providers has increased as well (8). This led to mental and physical errors and very low quality of patient management (7). Many HCWs went on long leave and sick leave. This is a vicious cycle and ultimately leads to a shortage of HCWs (9).
Many patients during the pandemic had aggressive behaviors toward hospital staff due to the lack of satisfaction with the management of their patients (10).
Violence against the HCWs is unethical in society, which leads to increased frustration and anxiety disorders among HCWs (9). It also leads to the closure of health facilities, and the community faces difficult access to healthcare services and increases the burden on the existing public health facilities (11).
Many HCWs have been infected, and the mortality rate has increased among them (11). In Pakistan, the prevalence of COVID-19 among HCWs was 46.97%. HCWs have has been at high risk of dying due to COVID-19; this risk is approximately 69.48% compared to the general population (12).
In a previous study,72.06% of HCWs were more likely to be infected with COVID-19 in the healthcare setting (12). Common causes of high mortality are unavailable PPE and working in the intensive care unit (12). The hospitals and isolation centers are overloaded, essential medical pieces of equipment are scarce, the HCWs are strained (13), and the viral load has increased in the surrounding environment of hospitals making HCWs more likely to be infected. The consequences of infection in HCWs are serious; infected HCWs can infect their family members and others (13). The number of HCWs is decreasing in Pakistan, and if the situation of this pandemic is not controlled, then this number will further decrease, and the burden on existing HCWs will increase. There is a need to take safety measures for HCWs to increase their morale.
2. Methodology
A systematic literature review was done to find out articles conducted from January 1, 2020, to December 31, 2021, on the impact of the COVID-19- pandemic on HCWs. Different databases were used, such as Scopus, web of science, PubMed, and Google Scholar. Different keywords were also used to search the articles: (((((((((((((Corona virus [Title]) OR (Health impact)) OR (Health system) AND (care provider impact [Title])) AND (stress [Title])) AND (Social impact [Title])) OR (Health workers [Title])) AND (Health System [Title])) OR (health services [Title])) OR (social determinants [Title])))))))))))).
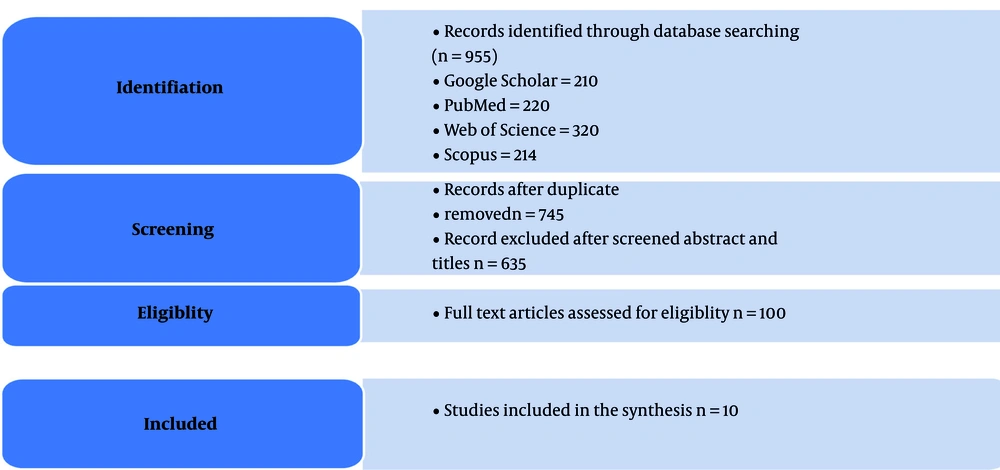
The references of the selected articles were also used to find relevant articles. A total of 955 articles were found; out of 100eligible articles, ten were included in the study.
2.1. Inclusion and Exclusion Criteria
The inclusion criteria were as follows: (1) studies on the prevalence of mental disorders among HCWs during the COVID-19 pandemic, (2) observational studies, (3) studies with available full text, (4) articles published in 2020 - 2021, and (5) studies assessing the impact of the pandemic on HCWs. Exclusion criteria were as follows: (1) irrelevant studies; (2) incomplete studies; (3) duplicate studies; and (4) studies with no available full text (Figure 1).
We included only articles in the analysis because similar articles were excluded.
2.2. Statistical Analysis
Heterogeneity was checked through the I2 (%) test. Egger’s test was used to determine the publication bias. Comprehensive meta-analysis (version 2.0) software was used for data analysis at a significance level of 0.05.
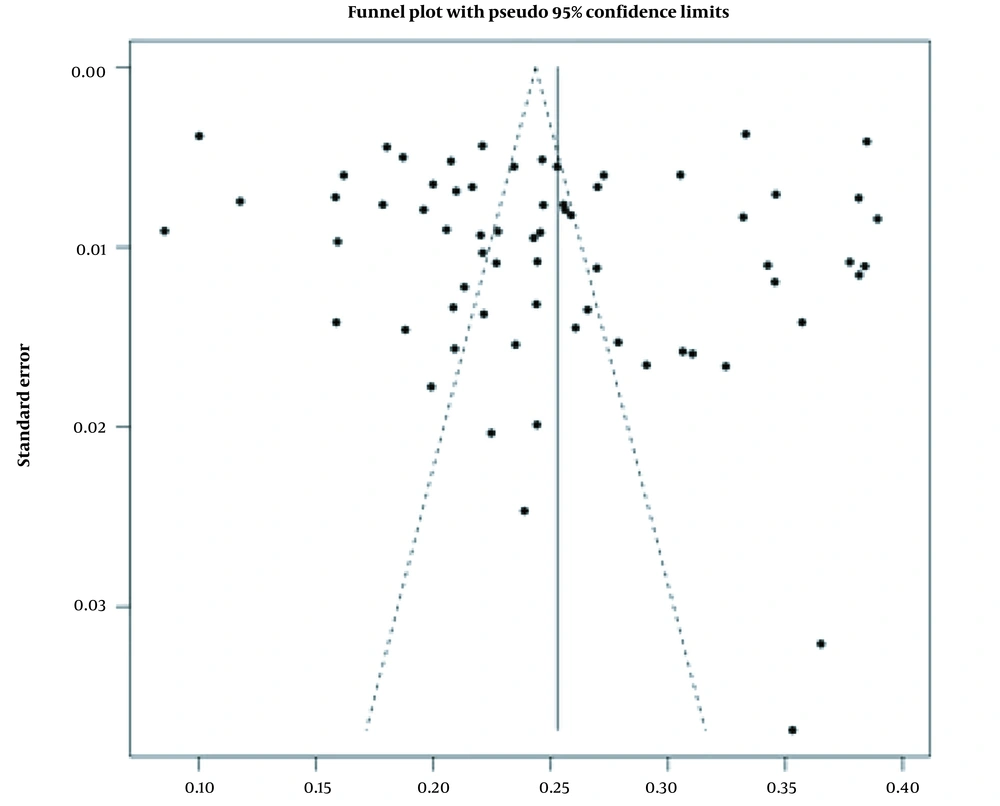
The finding showed that all groups of HCWs were affected by COVID-19. Findings also showed that more than 50% of HCWs were dying due to COVID-19-induced mental disorders (Figure 2). Figure 2 also shows heterogeneity among different studies.
3. Results and Discussion
3.1. Impact of the Pandemic on HCWs
In this study, there were various challenges faced by HCWs during the pandemic, such as heavy workload and mental health issues. The burden of COVID-19 patients has increased in all hospitals, which increased the workload of the existing medical staff. This has led to burnout of HCWs, and the quality of health services has decreased. It also has increased the mental health issues among HCWs due to workload. Different risk factors were found to cause the mental health of HCWs, such as workload, age, infection with COVID-19, and family dispute (Table 1).
| First Author’s Name (y) | Title of Paper | Sample Size | Country | Data Analysis Method | Data Collection Method | Challenges Faced by Health System and Health Care Workers (HCWs) |
|---|---|---|---|---|---|---|
| Goulia et al. (2010) (4) | General hospital staff worries, perceived sufficiency of information, and associated psychological distress during the A/H1N1 influenza pandemic | 400 | Hong Kong | To explore the impact of the pandemic on the HCW | Cross-sectional | Strong effect of the family |
| Amin et al. (2020) (8) | COVID-19 pandemic- knowledge, perception, anxiety, and depression among frontline doctors of Pakistan | 590 | Pakistan | To explore the impact of the pandemic on the HCWs | Case-control | Anxiety increased in HCWs |
| Hakim et al. (2021) (9) | Access and use experience of personal protective equipment among frontline healthcare workers in Pakistan during the COVID-19 emergency | 380 | Pakistan | To explore the impact of the pandemic on the HCWs. | Cross-sectional | Low quality of services |
| Turner and Niño (2020) (10) | Qualitative analysis of the coordination of major system changes within the Colombian health system in response to COVID-19: | 790 | Columbia | To explore the impact of the pandemic on the health system | Cross-sectional | Health system was collapsing |
| Turner et al. (2017) (12) | Evidence use in decision-making on introducing innovations: a systematic scoping review with stakeholder feedback. | 990 | Norway | To explore the impact of the pandemic on the health system | Case-control | Shortage of material resources |
| Rojas-García et al. (2018) (13) | Impact and experiences of delayed discharge: a mixed-studies | 2898 | USA | To explore the impact of the pandemic on the health system | Case-control | Lack of fund led to constraints in the hospitals for services |
| Brooks et al. (2020) (14) | The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. | 1289 | USA | To explore the impact of the pandemic on the HCWs | Case-control | Frustration and violence increased in the community |
| Roy et al. (2020) (15) | Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. | 798 | India | To explore the impact of the pandemic on the health system | Case-control | Lack of knowledge for resilience against the pandemic |
| Amin (2020) (16) | The psychology of coronavirus fear: are healthcare professionals suffering from corona-phobia | 1900 | Sweden | To explore the impact of the pandemic on the community | Case-control | Increased prevalence of psychological disorders in HCWs |
| Meyer et al. (2020) (17) | A checklist to improve health system resilience to infectious disease outbreaks and natural hazards | 479 | Austria | To explore the impact of the pandemic on the community | Case-control | Increased incidence of the outbreak of natural hazards |
There was a 33% increase in the workload of HCWs during the COVID-19 pandemic (18). The authors recommended the need for an increase in the number of staff in the ICU to combat this issue. This problem will be solved through the professional training of nurses (18).
The abuse against the HCWs has increased during the pandemic. There are several mental disorders among HCWs, such as the feeling of loss (anxiety), helplessness (depression), and fear (psychosis) (19). Violence during working in the hospitals also caused mental disorders in HCWs. The lockdown also increased the prevalence of mental disorders. Different risk factors are involved in the social damage in society. Common factors are unavailability of transport systems to access the hospitals for the treatment of patients, verbal abuse, and life threats in the majority of cases (20).
The common cause of violence against HCWs was spreading false information through social media, which created panic (20). Public hospitals in Pakistan have been in an emergency situation during the COVID-19 pandemic, and they already faced a lack of resources, which further increases the burden of the pandemic leading to collapse (21). In private hospitals, the number of admissions has increased due to the pandemic, which has led to their closure, and people were panicking to find a hospital for medical help (14). This situation may create panic in society, and people will transfer their anger to the hospital setting in the form of physical violence (16). The hospital's management behavior toward HCWs is hostile in nature, which further aggravates their situation. HCWs are the basic need of any society, and if they are stigmatized, then society will be deprived of healthcare services (17).
3.2. The COVID-19 Impact on the Health System
Different studies have been published on the impact of COVID-19 on the health system, in which policy development, training of staff, monitoring and evaluation, and early monitoring systems were used to deal with the impact of COVID-19 (15, 22-24). Quality of service should be improved to deal with the impact of this pandemic. Management of other diseases during the COVID pandemic is a major challenge, which should be fixed by providing health services for these patients by special need bases (25). Social distance, wearing a face mask, and hand washing are important measures to deal with the COVID-19 pandemic (26). Health education is an important pillar for the prevention of disease during the pandemic. Infection control measures and the development of the surveillance system are the key measures for the prevention of the impact of the COVID-19 pandemic. Applying good patient management plan obtained from previous pandemics can be an important step in preventing the transmissibility of COVID-19.
A pre-planned strategy by the health system can prevent mortality and morbidity among patients in hospitals and improve the quality of health services (27). In the pandemic situation, there is a need to strengthen primary healthcare systems because quick services will be delivered to patients leading to less burden on tertiary care hospitals. For instance, basic medical services can be provided to COVID patients at their homes through trained medical workers related to the primary healthcare care system. In addition, collaboration with private sector hospitals through a private-public partnership and continued monitoring and evaluation of surveillance systems are the basic and essential measures for the prevention of the spread of COVID-19 (28-30). Non- communicable diseases will be managed by the establishment of registry systems, which is the database system for chronic diseases. The social network is another tool to improve the lifestyle during the COVID-19 epidemic.
3.3. Community Impacts
The medical profession is a noble profession, and society should respect the HCWs. HCWs, when entering this profession, are aware of the high risk of disease and death. They have families and should make a balance between commitment to their family and profession (31-35). HCWs are the part of society that, when infected, are at high risk of transmission to society because they regularly contact patients. Most HCWs live in rent-based houses, and their owners warn them to vacate their houses because they assume the HCWs are a high-risk group of people, which transmit the infection to society (36-38).
It is well known that homemakers, public officials, students, women, and young people, which are more vulnerable in society, are affected more compared to the general public (39, 40).
4. Conclusions
The results of this study showed that the prevalence of mental stress has increased among HCWs. The study highlighted the fears among HCWs in Pakistan and the possible effect on the health system and society. These results will help the policymakers to develop policies, which reduce the impact of the pandemic on the health system and HCWs.