1. Background
Obstetric bleeding is a leading cause of nearly 14 million cases of maternal mortality that occur each year worldwide (1). Postpartum hemorrhage (PPH) is the most common type of obstetric hemorrhage. A cumulative blood loss equal to or greater than 500 mL within 24 hours following normal vaginal delivery or 1000 mL bleeding after cesarean section is considered PPH (1). Approximately one-quarter of all maternal deaths worldwide are attributed to PPH (2). It has been estimated that up to 3% of all women receive blood transfusion as a treatment for postpartum hemorrhage (3). In some conditions, patients with life-threatening bleeding require massive transfusion (i.e., transfusion of more than 10 units of blood/blood products within 24 hours) (1). Despite advances in the diagnosis, prevention, and management of obstetric hemorrhage, reducing deaths from obstetric bleeding remains a global challenge.
Most obstetric hemorrhages are preventable, and early and timely interventions can avert the development of dreadful conditions. Appropriate blood transfusion and rational clinical use of blood products are essential components of emergency obstetric care which have been shown to reduce maternal mortality (1). The reasonable use of blood products has been defined as "providing the right blood or products, in the right quantity, to the right patient and at the right time, and bridging demand and supply gap" (4).
Blood transfusion is a life-saving intervention, but inappropriate usage of blood components in obstetric emergencies is highly likely to increase the risk of morbidity and maternal mortality (5). Moreover, there are some controversies in transfusion practices carried out in obstetric emergencies, such as transfusion of a single versus multiple units of blood, utilizing blood products versus whole blood, transfusing blood products based on clinical judgment versus the level of hemoglobin, and using different guidelines for massive transfusion, which need to be scientifically addressed through the implementation of evidence-based policies (6).
Studies on the efficiency of blood transfusion practices have used various performance indicators. The three commonly used transfusion indices are as follows:
(1) Cross-match to transfusion (C/T) ratio is calculated by dividing the number of cross-matched units by the total number of actually transfused blood units. A ratio of 2.5 or below is considered an indication of appropriate blood component usage (7). A C/T ratio above 2.5 indicates that 60% of cross-matched blood units are not transfused (8).
(2) Transfusion index (TI) is defined as the number of transfused units per cross-matched patient (8). A value of 0.5 or higher indicates that the blood is being used efficiently. This indicator highlights the adequacy of the number of cross-paired blood units.
(3) Transfusion probability (T) is calculated by dividing the number of patients receiving the transfusion by the number of patients cross-matched multiplied by 100. A T value of 30% or higher is considered to indicate adequate blood transfusion requirements and usage (9).
2. Objectives
This study was conducted to identify the patterns, indications, and factors related to the transfusion of blood products in pregnant women admitted to a tertiary care hospital in Zahedan, Iran.
3. Methods
3.1. Study Setting
This cross-sectional study was carried out from September 2019 to March 2020 in Ali Ibn Abi Taleb (PBUH) Hospital, a 523-bed tertiary care and referral center in Zahedan, Iran. In addition to routine admissions, the majority of complicated obstetric cases in the province are referred to this hospital for specialist management.
3.2. Subjects
According to the data obtained from the hospital information system (HIS), during the first three months of the same year of the study, 1,400 pregnant women were hospitalized, of whom 310 (22%) patients had received the blood products. Hence, the expected prevalence of blood transfusion for sample size calculation was considered as P = 0.22, with a level of confidence of 95% (α = 0.05), and a relative precision of d = 0.03, and the estimated sample size was calculated as 733 pregnant women. The number of 733 cases was enough to determine the prevalence of blood transfusion. However, as there were about 17 independent variables in the regression modeling, a large sample size was needed to simultaneously examine the effect of the independent variables, so the sample size was doubled and rounded to 1,500 cases.
The inclusion criteria included all pregnant women admitted to maternity, obstetrics-gynecology, and postpartum wards in Ali Ibn Abi Taleb (PBUH) Hospital. Cases that had outcomes other than childbirth (natural vaginal delivery or cesarean section), such as abortion and hysterectomy, were not included in the study.
3.3. Data Collection
This study included two sets of data. First, blood requisition and transfusion by/of the hospital wards of maternity, obstetrics-gynecology, and postpartum were collected from the hospital blood bank registries for the study period of six months. For each ward, the number of requested, cross-matched, and transfused blood units and the number of cross-matched and blood-receiving patients were retrieved from blood bank records. The second data set, comprising the medical records of 1,500 pregnant women admitted to maternity, obstetrics-gynecology, and postpartum wards, was randomly selected from the hospital HIS. As a standard unique identifier, the medical record numbers for the patients admitted to those wards were compiled into three separate Microsoft Excel files and then entered into SPSS software. The required sample size and the share of each ward were determined using probability proportional to size based on the number of admissions during the first six months of the study year. The "select cases" command was used to generate a random sample of 570, 660, and 270 cases for the maternity, obstetrics-gynecology, and postpartum wards, respectively.
A 26-item checklist was developed to elicit patient-specific information on demographic characteristics, obstetrics and medical history, diagnosis, and transfusion details. The questionnaire collected data on the number of pregnancies, deliveries, and abortions, gestational age (weeks), multiple births, type of delivery (cesarean section, normal vaginal delivery, etc.), history of postpartum hemorrhage, blood transfusions in previous pregnancies, history of coagulation disorder and taking anticoagulants, placental and uterine complications, underlying disease (such as diabetes, hypertension, preeclampsia, etc.) blood transfusion in the current pregnancy, if any, the indication of blood and blood products transfusion, the type and the number of transfused blood products, patient's blood group, and Rh. All data were retrieved from the hospital HIS records.
3.4. Statistical Analysis
Numbers and percentages were used to present categorical data. In addition to the frequency and proportion of the type and the number of utilized blood component units, the C/T ratio, T%, and TI were calculated to assess blood usage patterns. The wastage rate of blood and blood product units was calculated as a percentage of the requested blood and blood product units that were not transfused to patients.
We fitted several logistic regression models using the forward likelihood ratio method to identify relevant factors associated with blood transfusion in pregnant women. The following variables that showed a conservative p value of less than 0.25 in univariate logistic regression models were included in the final model: maternal age, place of residence, education, history of abortion, history of bleeding in a previous pregnancy, history of blood transfusion in a previous pregnancy, multiple pregnancies, type of delivery, coagulation disorder in pregnancy, history of anticoagulant use, uterine complications, placental complications, underlying disease, gestational age, number of pregnancies, and number of deliveries. In all analyses, p values less than 0.05 were considered statistically significant. Data analysis was conducted using the SPSS version 23 statistical software package (Chicago, IL). Ethical approval for this study was obtained from the Zahedan University of Medical Sciences Ethics Committee (Ethics Committee Code: IR.ZAUMS.REC.1398.324).
4. Results
4.1. Blood Transfusion Indices
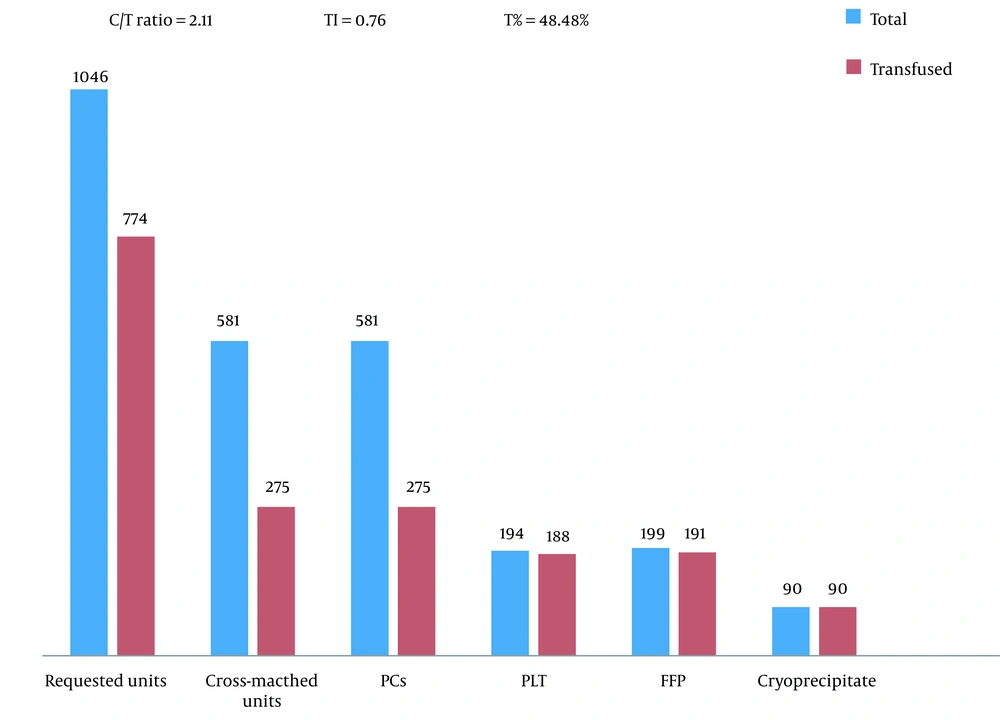
According to the hospital blood bank data during the study period of six months, a total of 1,046 units of blood products were requested by maternity, obstetrics-gynecology, and postpartum wards (Figure 1), including 581 units of packed red blood cells (54.6%), 199 units of fresh frozen plasma (18.7%), 194 units of platelets (18.2%), and 90 units of cryoprecipitate (8.5%). Out of 1,064 requested units of blood components, 774 (72.7%) units were transfused to patients. Out of 581 units of crossed-matched blood products, only 275 units were transfused, with a C/T ratio of 2.11. Overall, 275 blood units were transfused to 361 cross-matched patients yielding a TI of 0.76. Out of 361 cross-matched patients, 175 received the blood components, with a T% of 48.48%.
Frequency of requested and consumed blood products and related transfusion indices in maternity, obstetrics-gynecology, and postpartum wards, Ali Ibn Abi Taleb (PBUH) Hospital, Sep 2019 to March 2020, Zahedan, Iran (C/T ratio, cross-match transfusion ratio; TI, transfusion index; T, transfusion probability; PCs, packed red blood cells; FFP, fresh frozen plasma; PLT, platelets).
4.2. Blood Components Consumption Pattern
Out of 1,500 randomly selected pregnant women admitted to the three aforementioned hospital wards, 93 (6.2%) patients received the blood products (Table 1). A total of 37 (40%) cases received a single-unit transfusion, and eight (8.6%) cases received a massive blood transfusion. The packed red blood cells were the most frequently used blood product (71%), followed by platelets (10.6%). None of the patients experienced acute transfusion reactions.
| Variables and Subgroups | No. (%) |
|---|---|
| Number of blood product units transfused per case | |
| 1 | 37 (39.8) |
| 2 | 30 (32.2) |
| 3 - 9 | 18 (19.4) |
| 10 ≤ a | 8 (8.6) |
| Type of product | |
| Packed red blood cells | 66 (71) |
| Platelets | 10 (10.7) |
| Packed red blood cells and fresh frozen plasma | 6 (6.4) |
| Packed red blood cells and platelets- cryoprecipitate and fresh frozen plasma | 5 (5.4) |
| Packed red blood cells and fresh frozen plasma and platelets | 4 (4.3) |
| Packed red blood cells and platelets | 1 (1.1) |
| Packed red blood cells and fresh frozen plasma and cryoprecipitate | 1 (1.1) |
| Blood group | |
| O | 37 (39.8) |
| A | 22 (23.6) |
| B | 25 (27) |
| AB | 9 (9.6) |
| Rh | |
| Positive | 85 (91.4) |
| Negative | 8 (8.6) |
a Massive blood transfusion.
Uterine complications were the most frequent category of indications for blood product transfusion (37.6%), followed by placental complications (26.9%) (Table 2). Uterine atony and anemia were the most common indications for blood transfusion, constituting 32.2% and 17.2% of blood component recipients, respectively.
| Indications of Blood Transfusion and Subgroups | No. (%) |
|---|---|
| Group A: Placental complications | 25 (26.9) |
| Placenta adhesion (accrete-increta-percreta) | 9 (9.7) |
| Placenta previa | 7 (7.5) |
| Placental abruption | 5 (5.4) |
| Retained placenta | 1 (1.1) |
| A combination of complications (adhesion + previa) | 3 (3.2) |
| Group B: Uterine complications | 35 (37.6) |
| Uterine atony | 30 (32.2) |
| Rupture of the uterine wall | 5 (5.4) |
| Group C: Other causes of blood transfusions | 33 (35.5) |
| HELLP syndrome | 6 (6.5) |
| Multiple pregnancies and repeat cesarean deliveries | 2 (2.1) |
| Repeat cesarean deliveries | 4 (4.3) |
| Anemia | 16 (17.2) |
| Low platelet counts | 5 (5.4) |
4.3. Factors Associated with Blood Transfusion
According to the results of the multiple logistic regression model (Table 3), living in rural areas (OR = 2.12; 95% CI: 1.05 - 4.31), coagulation disorder during pregnancy (OR = 168.53; 95% CI: 54.69 - 519.33), uterine complications (OR = 727.32; 95% CI: 224.34 - 2357.99), placental complications (OR = 75.93; 95% CI: 30.66 - 188.08), Cesarean delivery (OR = 6.08; 95% CI: 2.51 - 14.63), and more than three deliveries (OR = 2.74; 95% CI: 1.30 - 5.72) were significantly associated with an increased chance of blood transfusion.
| Variables | Transfusion | No Transfusion | Crude OR (95% CI) | Adjusted OR (95% CI) | P-Value |
|---|---|---|---|---|---|
| Residence | 0.037 | ||||
| Urban | 55 (5.5) | 944 (94.5) | 1 | 1 | |
| Rural | 38 (7.6) | 463 (92.4) | 1.41 (0.91 - 2.16) | 2.12 (1.05 - 4.31) | |
| Type of delivery | 0.001 | ||||
| NVD | 20 (2.3) | 848 (97.7) | 1 | 1 | |
| Cesarean section | 73 (11.6) | 559 (88.4) | 5.54 (3.34 - 9.19) | 6.08 (2.51 - 14.63) | |
| Coagulation disorder in pregnancy | 0.001 | ||||
| No | 76 (5.1) | 1400 (94.9) | 1 | 1 | |
| Yes | 17 (70.8) | 7 (29.2) | 44.74 (18.01 - 111.14) | 168.53 (54.69 - 519.33) | |
| Placental problems | 0.001 | ||||
| No | 68 (4.6) | 1396 (95.4) | 1 | ||
| Yes | 25 (69.4) | 11 (30.6) | 46.66 (22.05 - 98.75) | 75.93 (30.66 - 188.08) | |
| Uterine problems | 0.001 | ||||
| No | 58 (4.0) | 1402 (96.0) | 1 | 1 | |
| Yes | 35 (87.5) | 5 (12.5) | 169.21 (63.94 - 447.77) | 727.32 (224.34 - 2357.99) | |
| Number of deliveries | 0.008 | ||||
| 3 ≥ | 62 (5.1) | 1142 (94.9) | 1 | 1 | |
| 3 < | 31 (10.5) | 265 (89.5) | 2.15 (1.37 - 3.38) | 2.74 (1.30 - 5.72) |
a The final multiple logistic regression model was adjusted for maternal age, education, history of abortion, history of bleeding in a previous pregnancy, history of blood transfusion in a previous pregnancy, multiple pregnancies, history of anticoagulant use, underlying disease, gestational age, and the number of pregnancies.
5. Discussion
This study aimed to assess the patterns of blood transfusion and related factors in pregnant women admitted to a tertiary care hospital using blood transfusion indices. In the present study, the C/T ratio was 2.11 (less than 2.5), TI was 0.76 (more than 0.5), and T was 48.48% (above 30%). All of the blood transfusion indices were within the recommended optimal range. This may be because our hospital is the only tertiary care referral institute in Sistan and Baluchestan Province, and our obstetrics and gynecology department specialists have expertise in managing complicated obstetric cases with life-threatening conditions. Every year they care for thousands of pregnant women with bleeding problems. During the past two decades, a wide range of interventions has been implemented to prevent avoidable maternal deaths resulting from bleeding, focusing on appropriate management of acute PPH and proper use of blood products in obstetrics and gynecology patients. These interventions have optimized therapeutic modalities in obstetric emergencies and improved blood transfusion indices.
Inappropriate use of blood products is common in the maternity, obstetrics, and gynecology hospital wards in Iran. In 2014, a survey on blood consumption patterns in teaching hospitals in Zahedan, Iran, found that the C/T ratio and TI indices in the gynecology ward were 2.62 and 1.31, respectively (10). A study on the efficiency of blood utilization in a teaching hospital in Birjand, Iran, showed that the C/T ratio, TI, and T for the maternity ward were 6.1, 0.2, and 12.4%, respectively. Similarly, the C/T ratio, TI, and T for the obstetrics-gynecology ward were reported as 5.3, 0.4, and 27.1%, respectively (11). Likewise, a study on the use of blood products in a university hospital in Mashhad, Iran, showed that the most unfavorable indices were observed for the obstetric and gynecologic ward where the blood transfusion indices of C/T ratio, TI, and T were 18.6, 3.37%, and 0.06, respectively (12).
In our study, a high rate of wastage (27.2%) was observed in blood products. The wastage rate of different blood products ranged from 0% for cryoprecipitate to 52.6% for PCs. This result is similar to a study in Zahedan, Iran, in 2015 that reported that the wastage rate in the maternity and obstetrics wards for different blood products was 28.4% and 24.4%, respectively (13). However, these figures showed an improvement compared to a study on the use of blood and blood components in Zahedan teaching hospitals in 2007, which found that 53.9% of requested blood product units in the obstetrics and gynecology wards were not utilized (14).
In this study, 40% of the cases received a single-unit transfusion. A review of the literature shows that the rate of single-unit transfusion ranges between 25% and 50% in both developing and developed countries (15-17). Some clinicians discourage the practice of single-unit transfusion. They believe this practice can be avoided in most cases as the patients are eligible for alternative conservative management (4). We found that the two most common indications for blood transfusion were uterine complications (especially uterine atony) and anemia. This is consistent with the findings of studies on transfusion practices in antenatal and postnatal patients conducted in developing countries (17, 18).
In this study, factors associated with an increased risk of peripartum transfusion included living in rural areas, coagulation disorder during pregnancy, uterine complications, placental complications, Cesarean deliveries, and having more than three deliveries. Women in rural areas are less likely to have timely access to skilled labor and essential emergency obstetric services. Moreover, underutilization of maternity services increases the chance of pregnant women experiencing complicated deliveries, increasing the possibility of blood transfusion in those patients. Coagulopathies that occur during pregnancy can present as obstetric emergencies with catastrophic bleeding events requiring blood components transfusion (19). Accordingly, women with abnormal placentation and uterine complications have an increased risk of postpartum transfusion. Cesarean section is associated with an increased risk of significant intra-operative blood loss; hence, women undergoing Cesarean sections are at increased risk for administering blood products in obstetric emergencies (20). In agreement with our study results, a multinational, randomized trial of 20,060 women with postpartum hemorrhage conducted in 193 hospitals in 21 countries found that cesarean section and the presence of identifiable causes of bleeding significantly increased blood transfusion likelihood in the study population (21). Accordingly, a retrospective cohort study carried out in China found that factors such as polyembryony, placental and uterine complications (including placental implantation abnormalities, placenta previa, retained placenta, intrauterine adhesions, and uterine rupture), stillbirth, and HELLP syndrome significantly increased the probability of perinatal blood transfusion (22). A timely referral to obstetrics and gynecologist specialists can help identify those risk factors. Therefore, necessary measures can be taken to prevent life-threatening complications, reduce the need for blood transfusions, and improve patient outcomes.
Patient blood management has been effectively fulfilled in various clinical settings, but it seems that some obstetricians and gynecologists are still oblivious to the importance of appropriate usage of blood products (23). Improving patient blood management in obstetrics and gynecology practices can be achieved through the training of updated standard guidelines on the appropriate utilization of blood components and regular audits of blood transfusion practices. This can be followed by active interventions to optimize therapeutic options in obstetric emergencies and prevent erroneous use of blood components (17).
One limitation of the present study is that it was conducted on data collected from a single referral hospital, and the findings only give an insight into the patterns of blood and blood product utilization in pregnant women in this single tertiary care referral center.
5.1. Conclusions
This study highlights the importance of proper and rational use of blood components in pregnant women. Development and meticulous administration of clinical guidelines for the appropriate use of different blood products and regular evaluation of transfusion practices are needed to identify areas for improvement.