1. Context
Severe Acute Respiratory Syndrome (SARS) coronavirus was first nominated as CoV-2019 (first stated in Wuhan, Hubei, the Republic of China, on December 30, 2019). Genetic specification studies on COVID-19 demonstrate a close relationship between Coronavirus and SARS in bats; hence, the source of the virus seems to be bats. The World Health Organization (WHO) renamed COVID-19 SARS-CoV-2 and explained coronavirus disease as a pandemic to be controlled (1). As it continued, different variants of this viruses spread rapidly in many countries, including Brazil (P.1), South Africa (1.351), the United Kingdom (B.1.1.7), New York (B.1.526), and California (B.1.427/B.1.429) (2). This disease has caused emergencies in general health, both physically and mentally.
Due to the lack of effective medicine, personal protective equipment (PPE), including face masks, face shields, and gloves, was discussed at the beginning of this pandemic. PPE is used as a physical barrier against infection transmission. Face masks are one of the effective supplies (3-5). The history of face masks returns to the use of the Polish surgeon in 1897 (6). Then in 1899, roller gauze masks were produced and used (7). In 1905, face masks were used to prevent the infection transmission of tuberculosis via sputum (8, 9). Later, when there was an outbreak of the epidemics such as Avian flu, SARS, Influenza, or even air pollution, face masks could decrease these pandemics dramatically (9, 10). However, at the beginning of the COVID-19 pandemic outbreak, many health officials in some countries announced that face masks were inefficacious in preventing this disease. Even in some communities, face masks have been prohibited due to social issues like terrorist attacks (10-12). According to the WHO’s preliminary guidelines, face masks were mandatory only for medical staff and vulnerable individuals with underlying health conditions and also for those who took care of COVID-19 patients (13). However, the operating instructions were different across countries (11). In the United States, wearing a face mask was mandatory for individuals aged above two years, while in Singapore, it was the same for all people. However, face masks were obligatory for those below 12 years of age, those with respiratory problems, and individuals spending a long time in public places (14). Many studies have examined the effectiveness of face masks in the coronavirus pandemic. Eikenberry et al. (15), Zeng et al. (13), Lyu et al. (14), Worby et al. (16), Wong et al. (17), Liu et al. (18), Cheng et al. (19), Swain (20), Brainard et al. (21), and Liang et al. (22) detected the use of face masks to intercept COVID-19 virus transmission.
Several studies have also surveyed the effect of environmental factors such as temperature and humidity on the stability of the COVID-19 virus against the new mortality outbreak. Davis et al. (23) investigated the impact of temperature on the stability of the influenza virus. The findings show an inverse relationship between temperature and humidity and the resistance of the COVID-19 viruses. With low humidity and cold conditions (lower temperature), the persistence of respiratory infections increases. The results show that the virus is more stable when the humidity and temperature range from 5 to 10°C (especially at 4°C). The virus is deactivated at 20°C, and finally, it is destroyed rapidly at temperatures above 60°C (24). Considering the significance of masks and given the inconsistencies in the effect of environmental conditions (temperature and humidity changes) on the spread of the COVID-19 virus in societies, these two factors were detected in this review meta-analysis study.
2. Objectives
The present systematic review meta-analysis aimed to investigate the effectiveness of face masks and environmental conditions, including temperature and humidity changes, in transmitting the COVID-19 virus.
3. Methods
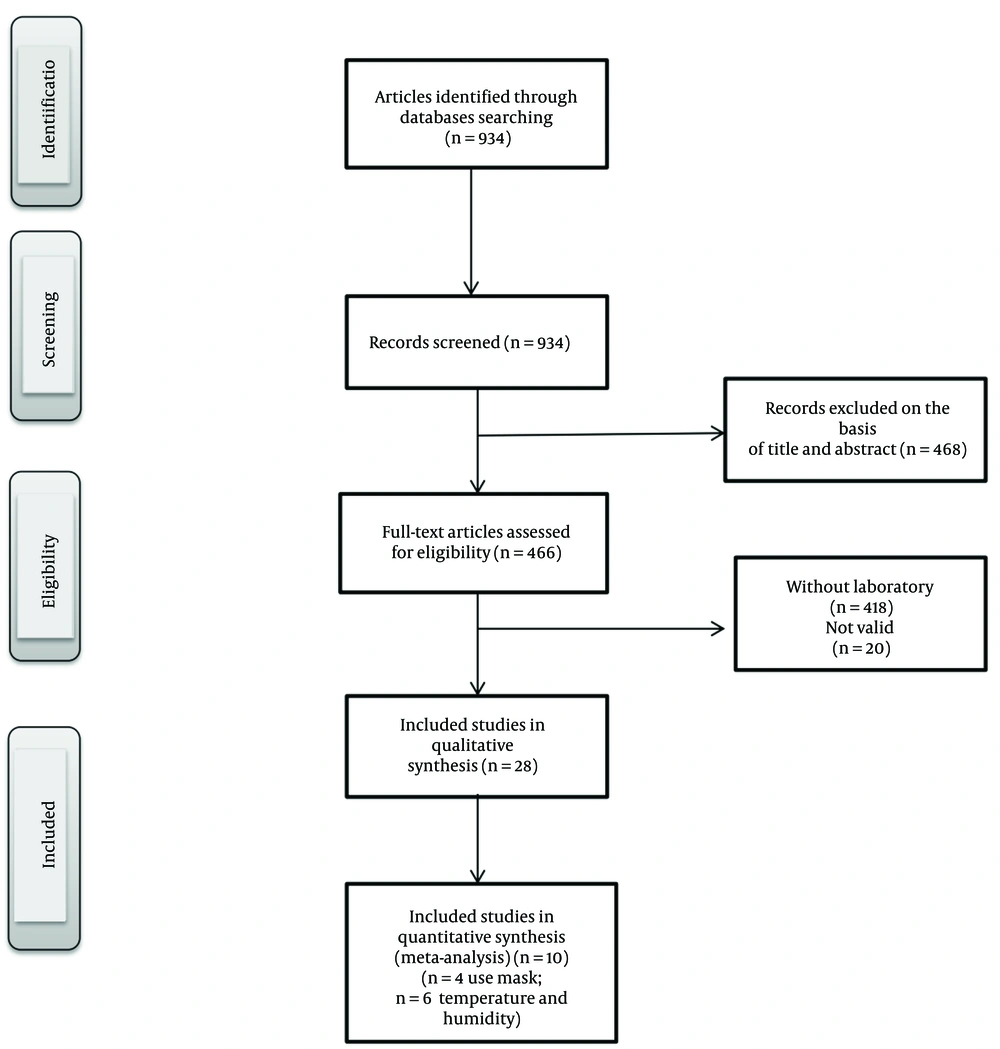
Systematic studies and meta-analysis methods are powerful tools as they combine and analyze data from different studies conducted in similar fields of research. To this end, articles from multiple electronic databases, including PubMed, Web of Science, Scopus, and Google Scholar, published by May 2020 were searched using the following keywords: (Mask) AND (Transmission), (SARS-COV) OR (COVID-19), (Temperature and Humidity) AND (Transmission), (SARS-COV) OR (COVID-19) (Figure 1).
3.1. Inclusion and Exclusion Criteria
Inclusion criteria were as follows: (1) COVID-19 virus detected in the laboratory, (2) appropriate study design, (3) high credibility of published journals, and (4) recency of obtained data. Exclusion criteria were (1) conferences/meetings abstracts, case reports, editorials, and review articles, (2) repetitive and overlapped articles, and (3) articles with no full texts.
3.2. Data Extraction and Quality Assessment
The articles were judged according to the preparation checklist. Articles were sifted by one autonomous reviewer (S.M). Disagreement was resolved in discussions by a second reviewer (Y.H). Then 934 articles were extracted from four databases, 466 of which were obtained after deleting duplicates. According to the mentioned criteria, 28 articles were selected. After checking the articles' details, those articles with similar titles or research methods were omitted. Finally, ten articles were selected, among which four cases examined the efficiency of face masks and 6 papers dealt with the effects of environmental conditions, including temperature and humidity changes, on the persistence of the COVID-19 virus.
3.3. Statistical Analysis
We assessed the relationship between face masks and temperature and humidity changes with the COVID-19 virus by estimating a relative risk (RR) and pooled mean depicted as effect size (ES) at a %95 confidence interval (CI). In this study, P < 0.05 was considered the significance level. The heterogeneity of studies included in this meta-analysis was evaluated using Cochran Q chi-squared test and I2 statistic. When Cochran Q showed P > 0.10 and I2 < %50 (25), the heterogeneity was considered to be low, and the RR and pooled mean were estimated based on the fixed-effects model; otherwise, random effects approach was adopted. The funnel plot, Begg's rank correlation test, and Egger's weighted regression tests were performed to evaluate possible publication bias; asymmetry in the funnel plot and P < 0.05 in Begg’s and Egger’s tests indicated publication bias. Trim and fill analyses were conducted to adjust the estimated pooled means when publication bias was approved (26). Moreover, a sensitivity analysis was performed by ignoring each study at a time and performing a meta-analysis on the remaining studies, and evaluating the estimated RR and pooled prevalence in the absence of the excluded studies (27). Stata software version 11.2 (Stata Corp., College Station, TX, USA) was used to analyze the collected data.
4. Results
In this study, 934 articles were extracted, from which 466 articles were removed based on the title or abstract, and 28 articles were selected. Finally, ten articles meeting the inclusion criteria were approved for meta-analysis. Table 1 presents the articles selected for this review meta-analysis on using face masks and lists some information, including the year of publication and some sample results. Table 2 also illustrates the selected articles addressing the effect of temperature and humidity changes on the prevalence of COVID-19. These researchers surveyed the effects of wearing/not wearing face masks and temperature and humidity changes on transmitting the COVID-19 virus in the study groups. Four studies compared the effects of wearing/not wearing face masks, and six studies examined temperature and humidity changes. Bae et al. (28) evaluated the efficacy of surgical and cotton masks in transmitting COVID-19. In another study, Leung et al. (29) investigated the effectiveness of using surgical masks in decreasing respiratory virus in respiratory droplets (droplet particles > 5 µm and aerosol particles ≤ 5 µm) in symptomatic individuals with coronavirus infection. Wang et al. (30) examined the risk of COVID-19 infection among medical staff using a mask.
| References | Year | Number of Samples | Temperature (°C) | Relative Humidity (%) | Relationship with Outbreak b |
|---|---|---|---|---|---|
| 1. Wang et al. (31) | 2020 | 14 | 8.72 ± 0.95 | - | + |
| 2. Ma et al. (32) | 2020 | 39 | 7.44 ± 3.96 | 82.24 ± 8.51 | + |
| 3. Wu et al. (33) | 2020 | 166 | 14.51 ± 4.83 | 49.9 ± 12.83 | + |
| 4. Shi et al. (34) | 2020 | 31 | 2 ± 0.66 | 41.52 ± 13.17 | + |
| 5. Huang et al. (35) | 2020 | 150 | 11.54 ± 5.47 | 65 ± 0.094 | + |
| 6. Bukhari et al. (36) | 2020 | 10 | 10 ± 2.33 | 44.61 ± 8.023 | + |
a Values are expressed as mean ± SD.
b + indicates an increase in outbreak, caused by temperature and humidity changes
Wang et al. (31) studied the effect of temperature change on COVID-19 transmission in 429 cities during 14 days. Ma et al. (32) investigated the effects of temperature and humidity changes on the deaths from COVID-19 in Wuhan, China, during 32 days. Wu et al. (33) discussed the daily patterns of temperature and humidity across 166 countries. The effect of temperature and humidity on coronary heart sickness was detected by Shi et al. (34) during 31 days. Huang et al. (35) studied the ideal temperature region for the scattering of COVID-19 during 150 days. Bukhari et al. (36) discussed the impact of weather on the prevalence of patients with coronavirus during 10 days.
4.1. Meta-analysis and Data Synthesis
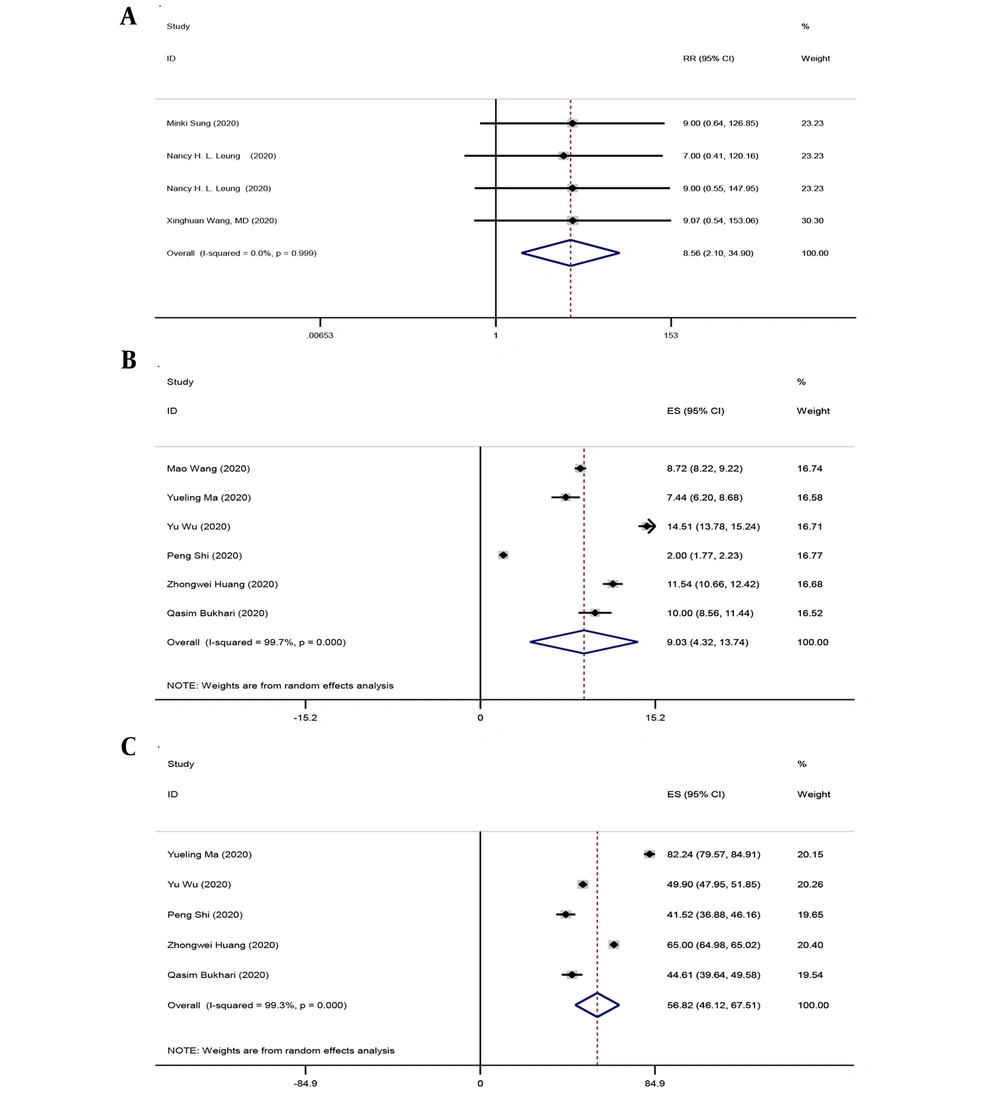
The effects of using face masks in preventing the transfer of the COVID-19 virus were examined in four articles. The meta-analysis findings revealed the effectiveness of face masks in preventing the transmission of the Covid-19 virus. According to these studies, not using face masks significantly increases the risk of virus transmission: RR (%95 CI) 8.56 ((2.10 - 34.90), I2 = %0.0 P = 0.999). (Figure 2A). Moreover, the findings of a meta-analysis of six papers addressing the effects of temperature and humidity changes on the COVID-19 virus suggested that the pooled mean of temperature changes was ES (%95 CI): 9.03 ((4.32 - 13.74), I2 = %99.7 P < 0.0001) and pooled mean of humidity changes was ES (%95 CI) 56.82 ((46.12 - 67.51), I2 = %99.3 P < 0.0001) during the outbreak of COVID-19 virus (Figure 2B-C).
4.1.2. Publication Bias and Sensitivity Analysis
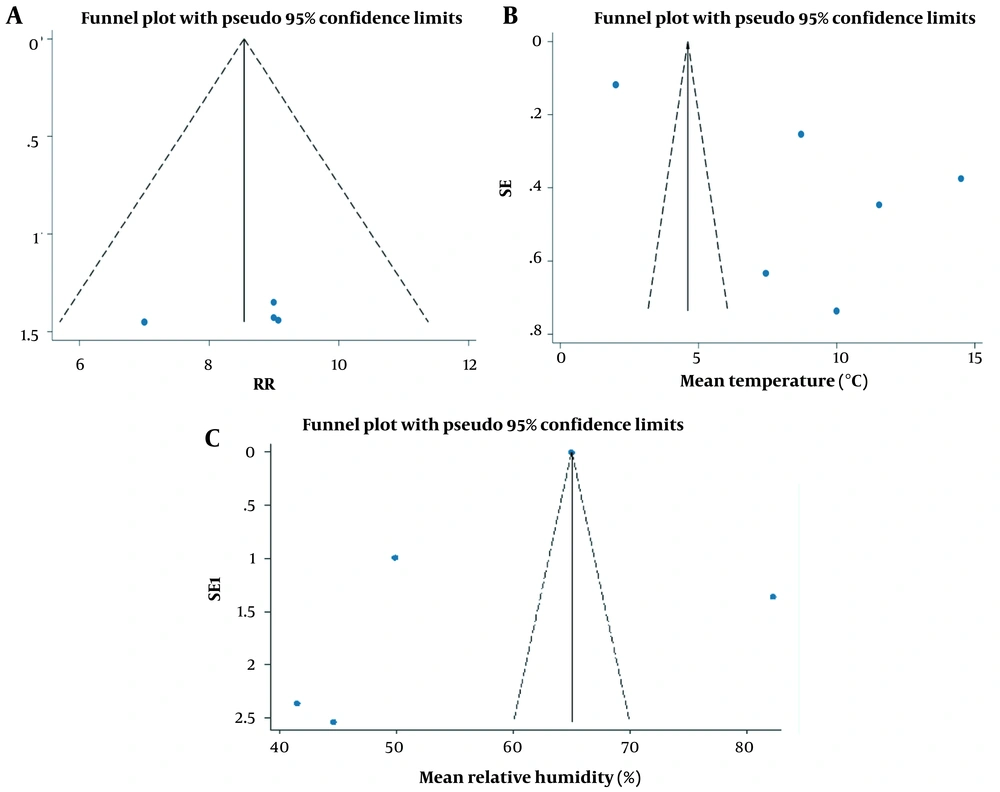
We used the Funnel plot, Egger’s regression, and Begg’s rank correlation tests to check publication bias. In the meta-analysis of using face masks, there was no significant publication bias based on the funnel plot and Begg's tests (Z = 0.34, P = 0.734) as well as Egger's test (t = -0.74, P = 0.539) (Figure 3A). The results of a meta-analysis addressing the effect of changes on temperature, Egger’s (t = 2.66, P = 0.056) and Begg’s (Z = 0.00, P = 1) tests, and the results of Begg's (Z = -0.24, P = 1) and Egger's (t = -0.84, P = 0.464) tests for the effects of humidity on transmitting COVID-19 showed relatively high asymmetry in funnel plot (Figure 3B-C); however, none of the statistical tests revealed significantly high publication bias. These tests are not powerful in detecting publication bias when the number of included studies is not high. Accordingly, we followed the trim and fill analysis to adjust the estimated RR and ES; however, the same results were obtained. We also did a sensitivity analysis to evaluate the impact of each study on the estimated effects size in our meta-analysis. For this purpose, we removed the studies one by one to determine whether or not the estimated RR and ES changed. None of the excluded studies in the sensitivity analysis showed an essential change in estimated RR and ES when all studies were included in the data synthesis.
5. Discussion
The results of this systematic meta-analysis review indicate the effectiveness of face masks in preventing the transmission of the COVID-19 virus. However, temperature and humidity changes has no effect on increasing the outbreak of the COVID-19 virus. Finally, all countries accepted face masks as a non-pharmacological intervention in the control of COVID-19 viral disease and as a strategy to prevent the spread of COVID-19 (4, 37-39). Studies on the transmission route of the COVID-19 virus have indicated that the major path of the virus transfer is respiratory fluid drops. Accordingly, individuals’ respiratory droplets at a distance of 5 - 10 m carry the virus, and the infected person’s aerosols in each drop release about 500 particles of the virus at a distance of 5 m (40). Respiratory droplets containing the virus are transmitted via three routes: (1) airborne, (2) contact, and (3) surfaces. Transmitting the contamination from one person to another is possible directly via airborne at a distance of 1 m and indirectly via contact with surfaces (41). SARS-CoV-2 and influenza are about 100 nm in size and have an aerodynamic diameter > 0.25 µm or 1 - 0.25 µm in two sizes (42, 43). These particles can bind to solid particles (bio-aerosol formation) because the smaller the particles, they are suspended more in the air and thrown out more distances (44). Drops in respiration are formed in different sizes. For example, there are particles with a size of 0.8 - 2 < m during normal respiration, 16 - 125 µm or < 0.8 - 7 µm in talking, 20 µm in shouting, 6 - 16 µm in coughing, and 125 - 7 µm in sneezing. They are deposited easily in particles > 20 µm. The formation of bioaerosols < 5 µm is important in virus transmission (45) since these bioaerosols are hung in the air for a long time and can puncture the alveolar space, and then viruses duplicate. Moreover, particles are easily transferred from one person to another at a distance of < 5 µm at an interval of 1 m via the air (46). Moreover, clinical studies have shown that aerosol inhalation from an infected person is the main transmission route. However, about %50 - %70 of individuals were unaware of their infection; hence, they are asymptomatic (47). These people simply are the source of virus transmission (48). The transfer rate of the virus from the respiratory of an asymptomatic contaminated person is equal to that of individuals with clinical symptoms (49). Accordingly, the presence of these individuals in public spaces, especially without ventilation, has caused contamination via bioaerosol droplets during coughing (40). In this regard, wearing face masks prevents accidental and unconscious hand-to-mouth contact and is a significant protection against the transmission of the COVID-19 virus. Moreover, commuting in public places after choking or sneezing, having contact with contaminated surfaces in the house, taking care of a COVID-19 person, and washing with other antiseptic combinations before and after eating are recommended (50). In their study, Brainard et al. showed that face masks decrease the likelihood of occurring respiratory signs by about %6 (OR 0.94, %95 CI 0.75 to 1.19, I2 %29). When those contaminated with a virus live in the same place with the others and wear face masks, the likelihood of getting sick for other members in the house decreases by about %19 (OR 0.81, %95 CI 0.48 to 1.37, I2 %45, 5 RCTs, (little assurance proof). Moreover, the shielding efficacy was highly insignificant if only the healthy individual or individuals contaminated with a virus wore face masks (OR 0.93, %95 CI 0.68 to 1.28, I2 %11, 2 RCTs (little assurance proof) (21). Liang et al. have conducted a systematic meta-analysis review on the effectiveness of using face masks against COVID-19. This study reviewed 21 articles, and the results showed that using face masks by health care providers and non-healthcare providers (Non-HCPs) can decrease the hazard of contamination with the COVID-19 virus by %80 (OR = 0.20, %95 CI = 0.11 - 0.37) and %47 (OR = 0.53, %95 CI = 0.36 - 0.79), respectively. Masks also had a protective effect against influenza viruses (OR = 0.55), SARS (OR = 0.26), and SARS-CoV-2 (OR = 0.04) (22). Research has revealed that hand washing decreases the likelihood of transferring the virus by about %55 (51). Maclntyre et al. (52) and Wang et al. (30) showed that washing hands and using face masks increase the protective effect so that the COVID-19 virus is eliminated by washing hands within five minutes (53). Accordingly, using face masks and handwashing can prevent the transfer of the COVID-19 virus from a contaminated person to other people in the community. The main point of using face masks is that in healthy individuals, it provides more protection to prevent the transfer of aerosols in the air, so that in infected people, even if they wear face masks, it does not completely prevent the transfer of bioaerosols. In conclusion, face masks are necessary for all individuals, either infected or healthy (54). After accepting the effectiveness of face masks, using an appropriate type of mask according to the target group is substantial. Due to the high burden of infection in health centers (40), using PPF2 and N95 masks are recommended for the staff of these centers and all individuals in direct touch with contaminated individuals. Cloth masks and surgical masks are suggested for healthy and asymptomatic people as well (55). Previous studies have showed that the effectiveness of fabric masks is not as high as surgical masks, so the penetration of particles is extremely high (%97), while it is %44 in surgical masks. In cases of shortage, the N95 mask can be disinfected (56). Some other strategies are the use of H2O2, gamma-radiation by C60, ultraviolet light, without water and moist heat, and oxirane (57-59). Generally, face masks should be in accordance with the target group, and hand washing and social distance of at least 1 meter from each other are critical functions in reducing the transfer of the COVID-19 virus. Accordingly, it can be concluded that the transmission rate of coronavirus from the air to the environment or another person depends on the size of the COVID-19 viruses, the distance of individuals, using or not using face masks, and other protective equipment (60).
Many other various factors, including environmental situations such as temperature and humidity, play a role in the transmission of the COVID-19 virus (61). They are considered to be effective in viral infections. As the results show, there was a significant relationship between weather situations such as temperature and humidity and the outbreak of the COVID-19 virus (62-65). (Many researchers believe that viruses possess a layer of fat sensitive to changes in heat, cold, humidity, and detergents. On the other, low temperatures cause physiological stress and weaken the immune system in people, which can cause the transmission and spread of viruses in communities). In contrast, many studies have confirmed the lack of a significant relationship between weather conditions such as temperature and humidity and the outbreak of the COVID-19 virus. Using conducive models, Awasthi et al. (66) concluded that there was no scientific proof to confirm the relationship between temperature and humidity and the spread of COVID-19 contamination, and that the capability to change the temperature and humidity of the environment is weak to prevent the COVID-19 pandemic. Another study by Wang et al. (67) showed that the potential impact of temperature/relative humidity on the effective reproductive number alone was not strong enough to stop the pandemic. Accordingly, an increase in temperature by 1°C is associated with a reduction in the R-value of COVID-19 by 0.026 (%95 CI (-0.0395 to -0.0125)) in China and by 0.020 (%95 CI (-0.0311 to -0.0096)) in the USA; an increase in relative humidity by %1 is associated with a decrease in the R-value by 0.0076 (%95 CI (-0.0108 to -0.0045)) in China and by 0.0080 (%95 CI (-0.0150 to -0.0010)) in the USA. Moreover, Walrand (68) found no relationship between an increase in the infection rate and temperature and humidity changes in a certain period. In general, ventilation, especially in closed places, and disinfecting surfaces with common materials such as sodium hypochlorite, hydrogen peroxide, acid peroxide, and hydrogen peroxide are effective mechanisms in controlling environmental factors (in the outbreak of COVID-19 virus).
5.1. Conclusions
The findings of this systematic review and meta-analysis illustrate the effectiveness of face masks, in general, in preventing the transmission of the COVID-19 virus. According to the findings, temperature and humidity changes do not increase the outbreak of the COVID-19 virus.