1. Background
Hospital staff members are among the most valuable resources of this organization, and they play a crucial role in the effectiveness of healthcare services (1). Hospitals' clinical and non-clinical staff must have the necessary skills to carry out their duties. Patient transporters are essential in displacing patients and equipment among different hospital wards. They are usually among the first staff members to contact patients, patients' companions, and visitors (2).
The duties and responsibilities of patient transporters have undergone many changes in recent years in a way that a patient transporter is no longer only expected to perform different displacements in a hospital. Scotland Health Facilities has presented several reasons for the changes in patient transporters' roles; these include the incidence and prevalence of different types of nosocomial infections, changes in clinical care, changes and advancements in medical technologies, vastness and complexity of hospitals, insufficient resources and the need for efficient resource allocation, and passage of various laws regarding patient rights (2).
Given the extensive changes in patient transporters' roles, training these staff members as well as improving their professional competencies have gained added importance recently. In the context of workplace, competency refers to a set of practical skills and knowledge an individual must possess in order to perform his/her duties. Professional competency can be evaluated using accepted standards and be developed through training. Performance is a significant part of professional competency, and is one of the fundamental components of establishing meritocracy in organizations (3).
Due to the importance of training hospital workers, various pre-service and in-service training courses have been designed in different countries to improve their professional competency. In Ireland, for instance, patient transporters are trained to address safety and hygiene issues as well as implement appropriate patient and equipment/material transfer techniques. The NHS (England) has also specified different requirements and skills for patient transporters; these requirements and skills include physical fitness, hard work, as well as the abilities to establish a friendly and appropriate relationship with visitors, establish an appropriate relationship with other staff members, receive training and following instructions, endure heavy workload, keep calm and act promptly in emergencies, and confront different diseases and the bodies of the deceased (1, 4).
Patient transporter duties have been discussed in many studies. It has been reported that developing and updating health and safety policies, guidelines, and standards play important roles in adequate preparation of the patient transporters for their professional career. In addition, it has been argued that the training programs for patient transporters should be evaluated constantly (1, 5).
Available evidence about training and empowering patient transporters as well as training programs in Iran points to existence of certain deficiencies and flaws. Reviewing the literature on training and improving the professional competency of hospital staff in Iran indicates that no study has ever been conducted on patient transporter competencies. On the other hand, numerous studies have been conducted on the competencies of clinical and non-clinical staff (6-9). This can be one of the plausible reasons for the insufficient attention to training patient transporters and improving their status in hospitals.
2. Objectives
This study aimed to identify the challenges and problems facing patient transporters and provide strategies to improve their competencies in teaching hospitals. In this study, the current status of patient transporters' competency regarding the knowledge and professional skills in teaching hospitals was evaluated.
2.1. Research Questions
(1) What is the most important competency regarding professional knowledge and skills required for hospital porters in teaching hospitals?
(2) What is the current status of competencies regarding the knowledge and professional skills of hospital porters in teaching hospitals?
(3) What are the components of a competency model regarding hospital porters' knowledge and skills?
3. Method
3.1. Study Design
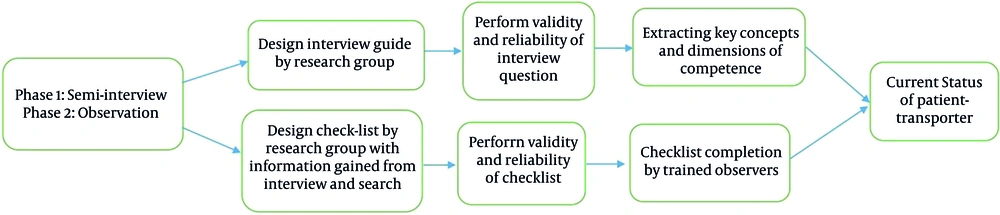
This study was an exploratory mixed method carried out in two phases in 2021. In the first phase, different competencies required for patient transporters were identified by conducting interviews. In the next phase, the status of patient transporters' job competencies was assessed through observation and using a checklist in the teaching hospitals in southeastern of Iran (Figure 1).
3.2. Data Collection and Sample
3.2.1. Qualitative Section
3.2.1.1. Determining the Required Competencies for Patient Transporters
The current status and required competencies for patient transporters were determined conducting semi-structured interviews. A primary framework was specified for the competencies caring out a comprehensive study, and a guideline was provided to perform interviews according to this framework. Interviewees were asked about the most critical competencies a patient transporter needs. The interviewees were patient transporters with a minimum work experience of three years, patients, medical staff (i.e., personnel in direct contact with patient transporters), hospital managers with a minimum management experience of three years, and faculty members and researchers with expertise on human resource and health system management. Purposive and snowball sampling were used, and interviews were carried out until saturation was obtained. First, experts having expertise on the subject of the study were selected, and the reasons for conducting the interview were explained to each of them and, then, the questions were discussed with the interviewees. The place and time of the interview was agreed upon by the interviewees. Interviews were conducted in teaching hospitals and University of Medical Sciences. All interviews were recorded and notes were taken. The average of interview time was about 40 minutes. The minimum and maximum interview times were 10 and 75 minutes, respectively. The interviews were conducted between March 2021 and August 2021.
In order to ensure the validity of the data, the interview summary was presented to the interviewees at the end of each interview for obtaining their approval. In order to objectify the data, simultaneous coding was used by two researchers, and the codes and classes were compared with each other. In order to increase the reliability of the data, all the codes and classes resulting from the analysis were cross-checked by the research team, and the results were compared. Furthermore, Lincoln-Guba's four criteria (i.e., credibility, dependability, confirmability and transferability) were used for examining the reliability. Inclusion criteria were: Those having direct working relationship with patient transporter, hospital managers with at least four years of management experience, faculty members and researchers in the field of healthcare human resource training, as well as managers and experts of the deputy development and management.
3.2.2. Quantitative Section
3.2.2.1. Determining the Status of Patient Transporters’ Competencies
In the second phase, the current status of patient transporter competencies was evaluated through observation and using the first phase results. Out of 14 hospitals in southeast of Iran, six hospitals were randomly selected; and of 210 patient transporters, 92 transporters were selected using available random sampling method. A checklist was produced by the researcher based on the results from first phase to assess the patient transporters' professional competencies. Using the checklist provided by the research team, the data were collected by the trained team through observation. It is worth mentioning that the data collection task was performed without disrupting the routine activities of patient transporters. The checklist used in this study explored four aspects including discipline and cleanliness, respect, communication, as well as technical and specialized issues. Each one of these dimensions included items with sub-items which included 5, 3, 3, and 8 items respectively. Grading was based on a spectrum of three options: Yes, no, and partly.
The face validity of the checklist, which included the arrangement of the questions, writing style, and appearance, was approved by five experts in healthcare and human resource management. Lawshe method was adopted to determine the content validity of the checklist. A copy of the checklist was sent to five faculty members of the above-mentioned fields in order to check and give comment on each question. To ensure the selection of the most critical and suitable content (item necessity), the content validity ratio (CVR) was used; the content validity index (CVI) was also used to check the items of the instrument (i.e., to examine the content). In order to quantitatively determine the CVR, moreover, five experts and professionals were asked to categorize the items into three categories, namely necessary, helpful but not necessary, and not necessary.
CVR was calculated using the reviewers’ opinions as follows:
where stands for the number of evaluators who think the item is necessary, and N is the number of all evaluators or reviewers who evaluate the item. In order to calculate the CVR, a score was attributed to each item by evaluators in terms of relevancy, simplicity and lucidity, and clarity based on a 3-point Likert scale. Afterwards, the content validity index was measured using the CVI formula.
Moreover, parallel form reliability was employed to check the reliability of the checklist. In this method, two separate forms probing the same issue were given to a group of individuals; each form included a selection of the test questions. In other words, two equivalent tests on the same concept or variable were designed and given to the same group in short intervals. Finally, the correlation coefficient of the scores before and after was found to be 0.98. The CI (0.99 – 0.85) validated the reliability of this checklist (10, 11).
3.3. Statistical Analysis
3.3.1. Qualitative Section
All interviews were transcribed on the same day, and the data analysis was done using Gal et al. adapted to this study, in which the steps included the problem understanding, data gathering, design and development, validation, product improvement, product testing, product revision, installation, design improvement, and product distribution (12). Max QDA version 20 software was also used for coding.
3.3.2. Quantitative Section
The required data were collected by the researcher in the field through observing patient transporters and using the checklist, without interfering their work. Then, the collected data were analyzed using descriptive and analytical statistics and SPSS 22.
3.4. Ethical Consideration
The study permit was issued by Kerman University of Medical Sciences and other southeastern hospitals. Also, verbal informed consent was obtained from patient transporters, hospital staff, managers, and patients. Data were collected using interviews and the designed checklists by a trained researcher. The objectives and importance of the study were explained to managers, hospital staff, patient transporters, and patients, and they were ensured about the confidentiality of their responses. They were also informed about the voluntariness of the study subjects’ participation. There was no time limit for answering the interview and checklist, and the average time to complete the checklist was about half an hour while the average interview time was about 40 minutes. This study was conducted in accordance with the 1975 Declaration of Helsinki (13).
4. Results
Table 1 presents the general information of interviewees regarding their gender, age, education, profession, and years of work experience. Majority of the respondents were between the ages of 36 - 45, and 67.2% of them were females.
| Variables | Frequency (%) |
|---|---|
| Sex | |
| Female | 45 (67.2) |
| Male | 22 (32.8) |
| Age | |
| 25 – 35 | 27 (40.3) |
| 36 – 45 | 28 (41.8) |
| 46 – 55 | 12 (17.9) |
| Education degree | |
| Specialist | 8 (11.9) |
| General doctor | 6 (9) |
| PhD | 8 (11.9) |
| Bachelor | 27 (40.3) |
| High-school diploma | 18 (26.9) |
| Type of specialist | |
| Faculty member | 6 (9) |
| Hospital management | 6 (9) |
| Physician | 10 (14.9) |
| Nurse | 12 (17.9) |
| Patient transporter | 13 (19.4) |
| Patient | 20 (29.9) |
| Years of service | |
| 1 – 8 | 30 (63.8) |
| 9 – 17 | 16 (34) |
| > 17 | 1 (2.1) |
Frequency and Percentage of Interviewees by Gender, Age, Education, Profession and Years of Work
According to the findings of the qualitative phase, the patient transporter job competency was divided into the two main categories of general and specialized skills and the six secondary categories of communication, respect, management, discipline, displacement and transfer, and professional knowledge. The findings showed that two main themes and six main codes were extracted from the results of the qualitative study as a framework for describing the ongoing situation. According to our research findings, each of the concepts contained several codes that demonstrated the different aspects of the given concepts. In general, 6 codes and 18 sub-codes were used for interview analysis (Table 2).
| Main Theme | Main Codes | Sub-codes |
|---|---|---|
| General skills | Communication | Communication with patients and their companions |
| Communication with doctors | ||
| Communication with nurses | ||
| Communication with other porters | ||
| Respect | Respecting patients | |
| Observing privacy | ||
| Respecting the confidentiality of patients’ files | ||
| Management | Control | |
| Time management | ||
| Planning | ||
| Discipline | Appearance | |
| Specialized skills | Displacement and transfer | Patient displacement |
| Equipment and supplies displacement | ||
| Occupational knowledge | Awareness of job description | |
| Awareness of displacement techniques | ||
| Familiarity with medical equipment |
Main Concepts and Related Codes in Qualitative Analysis
4.1. Communications
Patient transporters communicate with various groups of people in hospitals due to the nature of their job. Establishing effective communication and interaction with patients and their companions are among the most fundamental requirements in patient transport profession. The communication was so important that it was strongly emphasized by many interviewees during interview sessions: “If patient transporters receive the necessary training such as empathy, their performance improves significantly” (Faculty member).
4.2. Management
Having management competencies is another requisite skill for patient transporters to do their job correctly. patient transporters should have an effective plan for doing their job under the supervision of their supervisor, and they should constantly monitor and check this plan. Many timetables of hospital wards depend on the management skills of these staff members: "task prioritization leads to the timely presence and improved performance of patient transporters in the ward and minimizes the delays in the displacement of patients, equipment, and other things” (Hospital manager).
4.3. Discipline
Patient transporters are among the staff who communicate with the patients, patients' companions, clinical and managerial staff of hospitals. One of the critical factors in this regard is the maintenance of a proper appearance; "Patient transporters must have uniforms to be recognized more easily. They should be elegant in terms of appearance to gain people's trust. Moreover, they must minimize the transmission of infection or diseases by regularly washing their hands due to the high traffic in different hospital wards, especially in infectious disease wards" (Physician).
4.4. Displacement and Transfer
Patient transporters' primary duty in hospitals is the displacement of patients, equipment, and supplies. This duty is so important that any breaches of it can negatively influence the performance of whole hospital. Therefore, patient transporters need to have comprehensive and proper knowledge and competencies. "Patient transporters need to take part in training courses regarding proper displacement of different patients such as unconscious patients, patients who have undergone major surgeries, as well as patients of the intensive care unit to ambulances, internal medicine wards, diagnostic-therapeutic wards, and recovery rooms with no mistakes. patient transporters need to have the necessary knowledge and even know how to handle an instrument in displacing equipment and supplies (e.g., lab samples, files, bodies, letters, etc.) to minimize the damage” (Hospital manager and faculty member).
4.5. Patient Transporter Competency Status in the Studied Hospitals
Table 3 presents the mean of competency dimensions based on the questions. The highest mean was attributed to the special color of porter clothes, followed by checking the brakes on stretchers and wheelchairs, with scores of 2.97 and 2.68, respectively. The lowest mean was attributed to checking patient fittings before displacement and proper and friendly behavior, with scores of 1.40 and 1.46, respectively.
| Number | Competency | Mean (of 3 Points) | Standard Deviation |
|---|---|---|---|
| 1 | Punctuality | 1.75 | 0.94 |
| 2 | Identification badge | 2.36 | 0.93 |
| 3 | Special clothes color | 2.97 | 0.20 |
| 4 | Hand hygiene observation | 1.55 | 0.77 |
| 5 | Appearance | 2.61 | 0.60 |
| 6 | Respecting patient privacy | 1.75 | 0.85 |
| 7 | Respecting patient dignity | 1.97 | 0.59 |
| 8 | Suitable and friendly behavior toward patients | 1.46 | 0.52 |
| 9 | Having a sympathetic ear | 1.79 | 0.77 |
| 10 | Introducing themselves to patients | 2.64 | 0.71 |
| 11 | Paying attention to patients’ gestures and words | 1.96 | 0.63 |
| 12 | Getting help from other staff | 1.54 | 0.80 |
| 13 | Checking airways and ventilators before displacement | 1.48 | 0.74 |
| 14 | Checking patient fittings before displacement | 1.40 | 0.64 |
| 15 | Checking the brakes on stretchers and wheelchairs | 2.68 | 0.69 |
| 16 | Ensuring that wheelchair safety belt is fastened before displacement | 1.70 | 0.89 |
| 17 | Paying attention to patient comfort | 2.22 | 0.71 |
| 18 | Unnecessary stops when displacing patients | 1.53 | 0.83 |
| 19 | Observing safety rules in equipment displacement | 1.61 | 0.66 |
Means and Standard Deviation of Patient Transporter Competency Dimensions Based on Questions
Findings presented in Table 4 confirmed that the score given to porters by patients regarding the dimension of respect was low (1.71 out of 3), and the score for the technical and specialized dimension was average or lower (1.98). The highest score was found for the dimension of discipline (2.70), whereas the lowest one was recorded for the dimension of respect (1.71).
| Indicator Variables | Score |
|---|---|
| Discipline | 2.70 |
| Respect | 1.71 |
| Communication | 2.08 |
| Technical and specialized | 1.98 |
The Means of Patient Transporter Competency Dimensions in Teaching Hospitals
5. Discussion
Identifying the status of patient transporter competencies is very important for their career development. The results of the present study indicated that the list of required competencies for patient transporters included: establishing proper and effective communication with colleagues as well as with patients and their companions, respecting patient dignity, having a sympathetic ear, observing personal hygiene, having attractive appearance, displacing the patient properly, ensuring safety rules when displacing equipment, transferring the patient from bed to stretcher or wheelchair properly, and having basic knowledge of the patient fittings.
The study by Clark introduces the United States Department of Labor's competency model as a pyramid. This pyramid was in line with the list of competencies obtained in the present study. These competencies generally include management competencies, academic competencies, workplace competencies, technical competencies, and personal effectiveness competencies. Each of these competencies has sub-categories required for the staff to perform their tasks (14).
The present study results revealed that patient transporters' status was low regarding proper and effective communication as well as technical and specialized competencies. This may have been due to the lack of proper scientific and theoretical training courses for patient transporters, insufficient attention paid by hospital managers, low job rank, and insufficient knowledge to understand proper behaviors toward patients and their colleagues. According to the study conducted by Haran Ratna, effective communication in health service provision is of great importance, and the quality of health services decreases without it. Effective communication between patients and the health care system is a two-way process. If patients or service providers fail to clearly understand the conveyed information, the quality of service decreases (15). Parvizi et al. argued that the knowledge, attitude, and performance of staff in communication skills were undesirable (16). Other studies showed that the medical staff in many countries faced serious problems in establishing communication, and their communication skill levels were low (17, 18).
The variables of checking airways and ventilators as well as patient fittings are significantly low for patient transporting. This could be due to the lack of proper initial and in-service training of patient transporters and inadequate supervision of their duties. Moreover, their low job rank in hospitals can also be a factor contributing to the issue. In order to improve patient transporters’ technical and specialized competencies in hospitals, experienced and capable patient transporters can be employed to supervise other patient transporters in order for improving the services; moreover, the allocation of the tasks should be done based on patient transporters' capabilities, enabling them to do their jobs adequately. These components were not discussed by previous studies.
Proper and friendly behavior toward patients was poor, which increases stress and worsens the patients' psychological status. This may have been due to inadequate skills in establishing friendly communication with patients, lack of proper training in communication skills, and problems in the porters' daily lives. Furthermore, the study conducted by Rosenstein and O’Daniel indicated that destructive behaviors caused feelings of stress and frustration, loss of concentration, ineffective teamwork, and disruption of information transmission. It also found that destructive behaviors led to poor communication and disruption in the relationship among nurses, doctors, and patients (19). Due to the important role of patient transporters in increasing patient satisfaction, therefore, it was recommended that their morale and communication skills should be considered. It was also suggested that patient transporters should be educated sufficiently about the significance of proper patient communication in increasing patient satisfaction.
Another variable considered in the observation phase was unnecessary delays when displacing patients, which was average. This may have been attributable to the unnecessary conversations between colleagues, lack of proper training in the importance of taking the patients to the target ward on time, low social responsibility felt by patient transporters, and lack of adequate supervision of their duties. To resolve this issue, holding training sessions, familiarizing patient transporters with the importance of the assigned tasks, and increasing their professional motivation were recommended. Kulshrestha and Singh also highlighted the importance of proper patient and medical equipment displacement. They determined that the patient transfer was an important step, but was often overlooked. Therefore, they suggested that patient transporters and the staff in target wards should pay sufficient attention to constant delivery of the medical care (20).
Furthermore, the results of the present study indicated that hand hygiene was poor among patient transporters, which increases the risk of nosocomial infections. Lack of proper training for patient transporters, their insufficient attention to hand hygiene, and low levels of education are among the causes of their poor hand hygiene. The study conducted by Helena Ojanpera titled “Hand-Hygiene Compliance by Hospital Staff and Incidence of Health-care-associated Infections, Finland” also found that good hand hygiene compliance reduced the nosocomial infections in both patients and hospital personnel (21).
5.1. Advantages and Limitation
The checklist was designed based on the conducted interviews (in the comprehensive study, there was no specific checklist to examine the dimensions of patient transporter competencies). Patient transporter performance in hospitals was investigated without interfering with their work and causing any behavioral changes. Due to the limited number of national and international studies on patient transfer, it was highly recommended that further comprehensive studies should be carried out through interviewing and observing the behavior of patient transporters.
This study faced some limitations. First, a small population of interviewees was investigated in this study; therefore, its study results may not have been generalizable to all hospitals. In addition, greater participation of different specialists was not possible because of the access restrictions. Third, a local checklist was designed due to the lack of a standard checklist for patient transporters. Fourth, some of the interviewees may not have provided honest answers in consideration of administrative situation. Finally, this study was a cross-sectional study and, therefore, drawing firm conclusions about the causes was difficult.
5.2. Conclusions
Patient transfer was found an essential but often overlooked procedure in patient care. It was recommended that the transfer should be performed after stabilizing the patient to prevent any risks. Due to the importance of patient displacement to different wards and implementing diagnostic and therapeutic procedures, the patient transporters were detected in need of receiving initial and in-service training to improve their general and specialized competencies. Furthermore, it was suggested that patient transporters should receive incentives such as promotions, pay raise, and cash or non-cash rewards in order to improve their professional competencies. Therefore, the hospital managers were recommended to increase their awareness of the importance and effectiveness of the services provided by these staff members in hospitals.
The recommended incentives to motivate patient transporters were found multidimensional. One dimension concerned the financial incentives and adoption of performance-based payment policy, in which differences in the quality of service and patient satisfaction are carefully considered. Therefore, consideration of the patient satisfaction dimension in increasing or decreasing the payments may have affected the motivation of patient transporters to acquire the required skills. The second dimension concerned the job-esteem of patient transporters among the service providers in hospitals and service recipients. In this regard, improving patient transporters' job-esteem was found a strong motivation contributing to improving the quality of their services. It was suggested that the dimensions of their competence should be evaluated annually, and the training should be provided according to the evaluation results. It was also recommended that their work contracts should be renewed according to the training course completion and grades.