1. Background
Health literacy (HL) is a set of "cognitive and social skills that determine the motivation and ability of individuals to assess, understand, and use information to promote and maintain health" (1). Its scope goes beyond functional abilities and includes the skills necessary to manage individual health and therapeutic measures (2). Due to the increasing role of active participation of individuals in health decision-making, the expansion of digital health information, and individuals’ responsibility for their own health, reading and writing seem not to be sufficient for using health information. Therefore, additional skills are needed to manage and use health information. The evaluation of health information coming from different sources is among the necessary skills for promoting health literacy. In this regard, HL combines different abilities or skills, depending on the necessities to which the individual is exposed (3). Health literacy has been considered a critical factor in reducing health inequities and improving public health and well-being (4). Its importance becomes impressive considering the progressively rising health-related costs of non-communicable diseases (NC), making it necessary for people to manage their health with the effective use of health services (5).
As an essential factor for understanding and using health information and making health decisions, adequate HL directs individuals toward practical health promotion efforts, nurturing health-friendly environments, implementing efficient health policies, enhancing health care outcomes, and lowering health care costs (6).
Health professionals should assess people’s HL before designing health education or promotion interventions (7). Assessing HL, as an essential task, needs suitable instruments, and measuring the HL of the public faces some challenges (8). Public health comprises a wide range of research and practice and includes a broad range of topics and views, making it challenging to develop and use a single scale to be applied in a wide variety of settings (9).
Due to the lack of short and reliable instruments to assess the health literacy of 18-65-year-old Iranians in online surveys, we aimed to adapt Abel et al.’s HL-8 questionnaire to be used in Persian/Farsi language people (10). This tool consists of eight items to measure the HL of young adults. In order to use the tool for 18-65-year-old Iranians, it is necessary to assess the psychometric properties of the instrument.
2. Objectives
We aimed to validate this tool for subsequent use in research and practice among 18-65-year-old Iranians.
3. Methods
3.1. Participants and Data Collection
This study was conducted as a part of a national cross-sectional online survey among a sample of 2375 people aged 18 - 65 years old and living in the urban areas of Iran. In order to estimate the sample size, the country was divided into five clusters. According to Morgan’s table, n = 384 was considered as the sample size for each cluster. The final sample size was decided, taking into account a design effect of 1.2. Considering the ratio of the population of each cluster to the total population of the country, the necessary sample size was allocated to each cluster. Because the study was conducted online, only people who were literate and active on social networks could participate. This five-month study was conducted between August 3 and September 30, 2021. The online data collection method was chosen because of its ease of conduct, the possibility of recruiting a larger and more heterogeneous sample size, and cost-effectiveness (11).
3.2. Instrument
We used the "brief survey instrument for research on public health and health promotion", which was developed and validated by Abel et al. (10). This instrument consists of eight items aiming at measuring HL among young adults. The range of scores for each item in this scale is from 0 (not at all) to 5/4 (a great deal), with higher scores indicating higher HL. The demographic data gathered included gender, age, marital status (single/married), and job (government employees, self-employed, student, housewife).
3.3. Translation Procedure
The standard translation/back-translation protocol (12) was applied to translate the original instrument into Persian. Two professional translators independently translated the initial questionnaire into Persian. The Persian-translated version was then back-translated into English by two other translators. All four translators were bilingual and familiar with the study’s subject.
3.4. Data Collection
We designed the questionnaire on the Porsline website (13). The questions were organized into two parts: (1) queries related to the HL-8 tool; and (2) demographic questions. The scoring of the HL-8 tool was performed on five- and four-point Likert scales from not at all (0) to a great deal (5/4). The link to the survey was propagated using email, WhatsApp, and social media like Instagram. All Iranians in the age range of 18 to 65 years, regardless of their ethnicity, had the chance to participate in the study. The only exclusion criterion included living outside Iran at the time of conducting the study.
3.5. Statistical Analysis
A significance level of 0.05 was considered for all tests, and IBM SPSS statistics version 26 was used for analyses.
3.6. Content Validity
The demographic variables of the subjects were summarized using descriptive statistics. In order to quantitatively validate the content of the scale, we applied content validity ratio (CVR) and content validity index (CVI) (14). In order to assess CVR, 11 experts in the fields of public health, psychology, health education, and health promotion were requested to appraise the necessity of each item. The scoring was based on a 3-point Likert scale (15). The initial 11 experts also evaluated the CVI of the scale in terms of the clarity, relevancy, and simplicity of the items. Scores higher than 0.99 for CVR and 0.79 for CVI were considered to be appropriate (16). An impact score of ≥ 1.5 was considered to include any item in the next stage. Then a pilot study was conducted to test the final version of the scale among 1187 participants.
3.7. Construct Validity
Principal axis factoring with varimax rotation was conducted to investigate the construct validity and factor structure of the scale. Confirmatory factor analyses (CFA), with a robust maximum likelihood, was also performed to assess the model’s parameters. To conduct exploratory factor analyses (EFA), a randomized split of the data was performed in the sample, and applying the randomization function, the data gathered from 1187 samples were selected. In the EFA, the factor loadings equal to/more than 0.4 were considered to be appropriate. Also, the eigenvalues higher than one were considered as the basis for determining the number of factors. In order to estimate the adequacy of the data, we applied Kaier-Meyer-Olkin (KMO) and Bartlett’s test of sphericity. Next, applying the analysis of moment structures (AMOS)-version 10.0, CFA was conducted on the remaining data from 1187 samples. To investigate how well the model fitted the data, the comparative fit index (CFI), the Tucker-Lewis index (TLI), and the root mean square error of approximation (RMSEA) were used (17-19).
3.8. Reliability
Cronbach’s alpha test was used to assess the internal consistency of the instrument. The least acceptable Cronbach’s alpha coefficient was considered to be 0.7 or higher. We also used intra-class correlation coefficient (ICC) to evaluate the test-retest reliability (ICC ≥ 0.70 was considered to be acceptable).
3.9. Convergent Validity
Spearman correlation was applied to investigate the relationship between different domains of the HL scale.
4. Results
4.1. Characteristics of the Participants
In this study, the data obtained from 2375 adults aged 18 - 65 years old were analyzed. Most of the participants were male (1610, 67.8%), married (1610, 67.8%), and 31-59-year-olds (1672, 70.4%). No statistically significant difference was found in the level of HL by marital status (P = 0.39). The association of age with the level of HL was statistically significant (Table 1).
| Variables | No. (%) | Health Literacy Score (Mean ± SD) | P a |
|---|---|---|---|
| Gender | < 0.001 | ||
| Female | 765 (32.2) | 24.42 ± 4.00 | |
| Male | 1610 (67.8) | 23.41 ± 4.61 | |
| Marital status | 0.39 | ||
| Married | 1610 (67.8) | 24.14 ± 4.20 | |
| Single | 765 (32.2) | 23.98 ± 4.30 | |
| Age (y) | < 0.001 | ||
| 18 - 30 | 628 (26.4) | 23.89 ± 4.23 | |
| 31 - 59 | 1672 (70.4) | 24.26 ± 4.17 | |
| 60 - 65 | 75 (3.2) | 21.96 ± 4.99 | |
| Employment statues | < 0.001 | ||
| Government employee | 1017 (42.8) | 24.79 ± 3.98 | |
| Self-employed | 306 (12.9) | 23.01 ± 4.53 | |
| Student | 663 (27.9) | 22.87 ± 4.32 | |
| Housewife | 389 (16.4) | 24.23 ± 4.16 | |
| Total | 2374 | 24.09 ± 4.23 |
a Derived from chi-square.
4.2. Content Validity
Applying the qualitative recommendations of the expert panel, which were mainly about wording and phrasing the items, some technical revisions were applied to improve the scale. The scores of CVI (0.91) and CVR (0.95) were considered to assess the relevancy of the questionnaire’s items, which showed satisfactory results for the scale and its items.
4.3. Factor Structure
The scale’s KMO score was 0.82 (approx. chi-square = 1696.131. df = 28, P ≤ o.oo1). In communalities, all items' scores were equal to 0.82 (approx. chi-square = 1696.131, df = 28, P ≤ 0.001). In the table of communalities, all items were identified to have extraction values greater than 0.4.
Four distinctive factors were extracted from the final iteration of EFA, including (1) factor 1: Finding and evaluation; (2) factor 2: Understanding; (3) factor 3: Decision-making; and (4) factor 4: Interacting. These factors altogether explained 71.9% of the total variance.
Table 2 shows the factors (subscales) and their associated means (standard deviations (SD)), number of items, ranges, skewness, and kurtosis.
| Factors (Subscales) | Number of Items | Range | Mean ± SD | Kurtosis | Skewness |
|---|---|---|---|---|---|
| Finding and evaluation | 4 | 4 - 19 | 12.46 ± 2.66 | -0.079 | -0.340 |
| Understanding | 2 | 2 - 9 | 6.35 ± 1.49 | -0.616 | -0.497 |
| Decision-making | 1 | 1 - 6 | 3.83 ± 0.8 | 0.946 | -0.609 |
| Interacting | 1 | 1 - 6 | 3.24 ± 1.04 | -0.102 | 0.215 |
Table 3 shows the data related to initial eigenvalues (before rotation), rotation sum of squares (variance accounted for after rotation), and the percent of variance explained (after rotation) by each factor.
| Health Literacy | Factors | |||
|---|---|---|---|---|
| F1 | F2 | F3 | F4 | |
| To what extent do you comprehend health topics in information brochures? (HL3) | 0.7 99 | |||
| I am aware of the resource in which I can search for information on these topics when I have questions about complaints or diseases. (HL4) | 0.783 | |||
| When I decide to do something for my health without being ill, I am aware of the resource in which I can search for information on these topics. (HL5) | 0.708 | |||
| To what extent are you capable of choosing the offers and recommendations that suit you the most? (HL8) | 0.639 | |||
| Brief survey instruments for research in public health and health promotion. (HL1) | 0.890 | |||
| To what extent do you recognize medications in the instruction leaflets? (HL2) | 0.626 | |||
| When you have some questions regarding health issues, how often do you capable of obtaining information and suggestions from others (friends and family)? (HL7) | 0.983 | |||
| If your friends or a family member have questions regarding health issues, how often do you capable of helping them? (HL6) | 0.985 | |||
| Rotation sums of squares | 2.090 | 1.320 | 1.053 | 1.005 |
| Percent of variance explained | 33.607 | 15.930 | 12.692 | 12.672 |
4.4. Confirmatory Factor Analysis
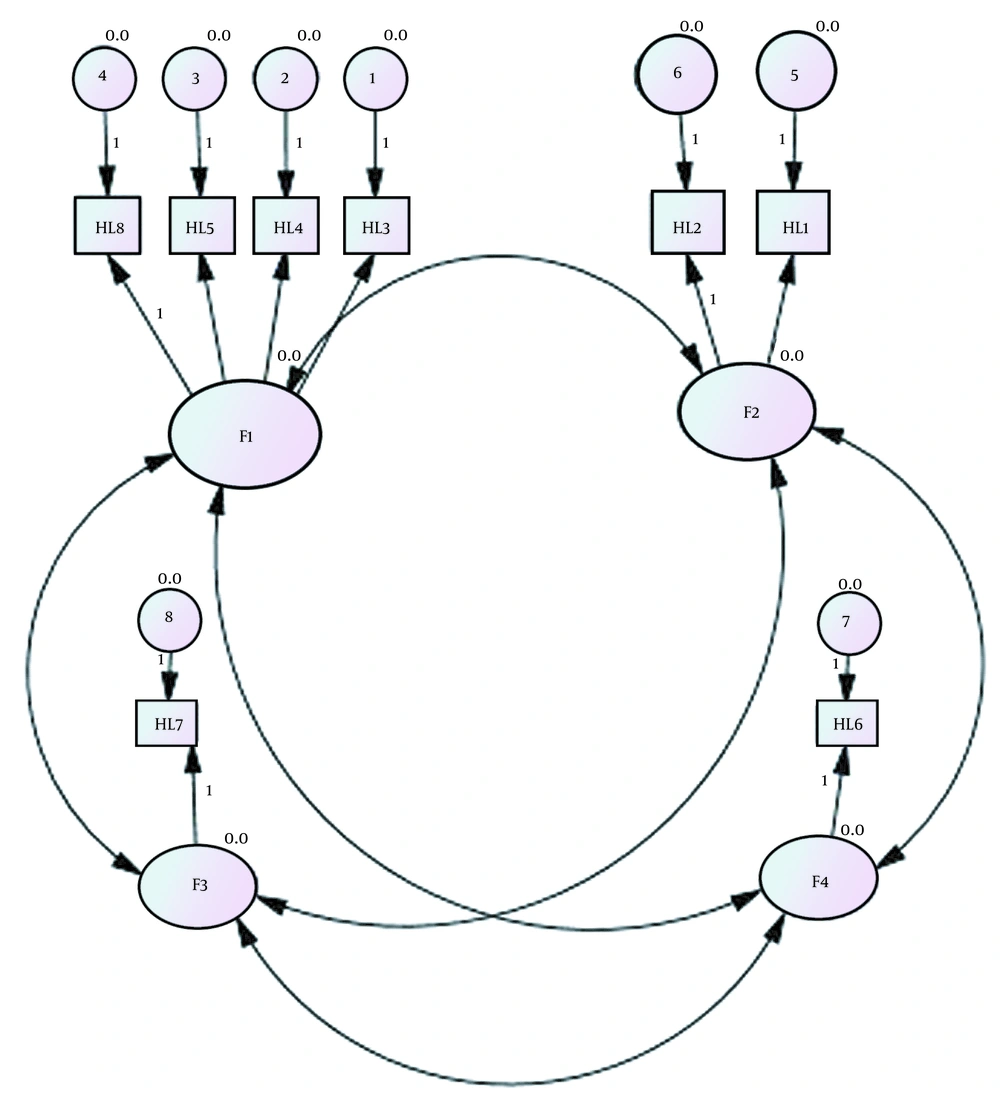
Figure 1 represents the results of CFA, showing a good fit of the results to the model (χ2 = 778.33; χ2/df = 1.60; SRMR = 0.049; RMSEA (90% CI) = 0.043 (0.038 - 0.049); CFI = 0.98; NFI = 0.95; and NNFI = 0.98; GFI = 0.87).
4.5. Reliability
Cronbach’s alpha coefficients for the dimensions of finding & evaluating, understanding, decision-making, interaction, and the questionnaire as a whole were 0.762, 0.462, 0.750, 0.820, and 0.593, respectively, and the respective test-retest correlation coefficients were also obtained as 0.85, 0.94, 0.75, 0.82, and 0.86. The F4 (interaction) domain showed a statistically significant (P < 0.001) correlation with the F1 (r = 0.695), F2 (r = 0.460), and F3 (r = 0.370) factors, and the F3 (decision-making) dimension was also significantly associated (P < 0.001) with the F1 (r = 0.567) and F2 (r = 0.453) factors. The correlation (r = 0.678) between the F1 and F2 factors was statistically significant as well (P < 0.001). Overall, correlations between the factors were statistically significant (P ≤ 0.05).
4.6. Health Literacy
The mean ± standard deviation of the HL score was 24.09 ± 4.23. Although married respondents scored higher, no significant relationship was found between HL and marital status (P = 0.39). The HL score was significantly different between females and males, as well as between different age groups and based on employment status (Table 1).
5. Discussion
The results showed that the Persian version of HL-8 (10) was a valid and reliable instrument for measuring HL among 18-65-year-old Iranian populations and could be considered a proper tool for measuring HL in online surveys among general populations (20-23). There are several tools for measuring HL, such as the rapid assessment of adult literacy in medicine (REALM) (24), the test of functional health literacy (TOFHLA) (25), and the newest vital sign (NVS) (26), which have been in used in a wide range of studies for a long time. For several reasons, there are many criticisms around these instruments, including the high number of items, and thus the need for a long time to be answered, inefficiency when used in interventional studies, not being developed based on the health promotion approach, not evaluating all domains of HL, and not primarily developed for measuring HL in general populations (27).
Tavousi et al., in their study, developed a psychometrically tool the health literacy instrument for adults (HELIA) to assess HL among Iranian adults. Although the instrument was reported to be a short and easy-to-use tool, its provisional version included 47 items (28), taking about 15 to 20 minutes to be completed by a low-literate respondent. Abel et al. (10) also developed a temporary survey that yielded a reliable HL score. They focused on assessing HL in the field of public health and developed an HL-8 scale based on the presumption that people behave dynamically in their society (i.e., a health promotion perspective). Assuming that HL gives an advantage to people in all age groups, the focus of the recent study was mainly on the private realm. In the present study, we conducted EFA on a data set gathered from a large sample of 18-65-year-old Iranians, which is a strength of our study. Also, the reliability of the initial eight-item structure of the original version of the instrument was approved in the present study. Our proposed structure included four factors: F1: Finding & evaluating, F2: Understanding, F3: Decision-making, and F4: Interacting. In the main study developing the tool (10), only two subscales, including interactive and critical HL, were described.
5.1. Conclusions
The Persian version of HL-8 was found to have appropriate validity and reliability. As we identified, all factors of HL-8 were compatible with the theoretical basis of HL domains, and considering the high level of internal consistency among their items, we could claim that this Persian version of the scale was able to appropriately assess HL based on its four basic domains. Therefore, the HL-8 developed here, containing eight short items, can be used as a time- and cost-effective tool in online health surveys among general populations.