1. Introduction
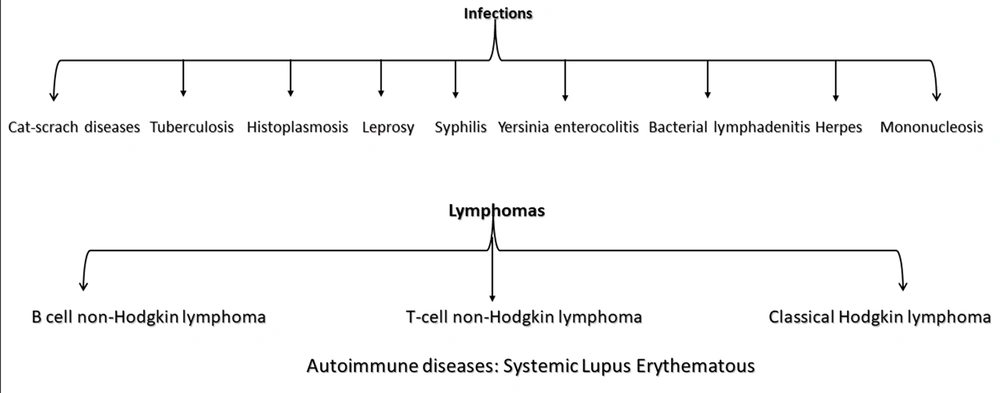
Kikuchi disease, or necrotizing histiocytic lymphadenitis, is more common in Asians than others, with young people being more susceptible than the elderly. The incidence of Kikuchi-Fujimoto disease (KFD) is currently unknown. Although all age groups may be affected, the disease usually occurs in people under 30. It is more common in women than men. However, recent studies have shown that the proportions are equal between the two genders. Several infectious and autoimmune agents, including herpes simplex types 6 and 8, parvovirus B19, human immunodeficiency virus (HIV), and infectious mononucleosis, have been proposed as the causes of the disease. The immune response of T cells and histiocytes to infectious agents is likely to play a role in the pathogenesis of KFD (1) (Figure 1).
One of the most common clinical manifestations of KFD is unilateral neck lymphadenopathy. It can lead to multiple and widespread adenopathies in other body parts with a firm and rubbery consistency, rarely larger than 2 cm in diameter, and sometimes painful when touched. Fever is reported in 20% - 50% of patients. Other symptoms include nausea, vomiting, sweating, weight loss, chills, diarrhea, abdominal pain, headache, myofascial pain, and peripheral neuropathy (2).
The prevalence of leukopenia and atypical lymphocytosis in KFD is 25% - 50% and 25%, respectively. An increase in CRP, ALT, and LDH and a slight increase in erythrocyte sedimentation rate (ESR) are also observed. The anti-nuclear antibody, rheumatoid factor (RF), and systemic lupus erythematosus (SLE) cytology tests are usually negative. This disease is benign and usually resolves spontaneously within a few weeks to a few months, and its recurrence is rare (3). The clinical and paraclinical features of this disease are very similar to lymphoma and lupus. In addition to these two diseases, Kawasaki disease, tuberculosis, cat scratch diseases, Yersinia, toxoplasma, and infectious mononucleosis should also be considered. Patients with persistent fever and cervical lymphadenopathy should be considered for this disease (4). Pathology of lymph nodes is the key to diagnosing this disease. Ultrasound findings, including the size, shape, and boundaries of the lesion, can help distinguish Kikochi lymphadenopathy from lymphoma. One of the most important differential diagnoses of this disease is lupus, which should be ruled out in all patients diagnosed with KFD. Therefore, females should be monitored for autoimmune diseases. This disease has no specific treatment, and the treatment is supportive with anti-fever and anti-inflammatory drugs, but glucocorticoids are used in severe cases of the disease (5, 6).
The incidence of KFD after vaccination is relatively low. Therefore, in this report, we are trying to raise awareness among doctors and pathologists about the rarity of this disease and how to deal with similar cases. It should be noted that the purpose of this paper is not to describe the type and dosage of treatment.
2. Case Presentation
A 30-year-old woman with painless cervical lymphadenopathy visited Yasrebi Hospital, Iran, in October 2022. Clinical examination revealed that she had received the first dose of Sinopharm in her right arm 30 days earlier with no side effects. The second dose was injected into the left arm 24 days after the first one. Five days after the second injection, she experienced fatigue and a non-painful left cervical nodule of 8 × 6 cm behind the sternocleidomastoid muscle. The nodule was soft, mobile, and without tenderness or redness. A computerized tomography scan showed multiple highly hypoechoic lymph nodes behind the sternocleidomastoid muscle on the right side of the neck, each measuring approximately 1.5 × 1.6 cm (Figure 2). Abdominal and pelvic ultrasound revealed only slight spleen enlargement. A serological test for (severe acute respiratory syndrome-Coronavirus 2) SARS-CoV-2 RNA was negative. Preliminary tests at the hospital were Hb: 12.5 g/dL, WBC: 3600/µL (Neutrophils: %67), and platelets: 235000/µL. However, C-reactive protein (CRP), Rheumatoid factor (RF), and purified protein derivative (PPD) were negative, and liver, thyroid, and urine tests were normal.
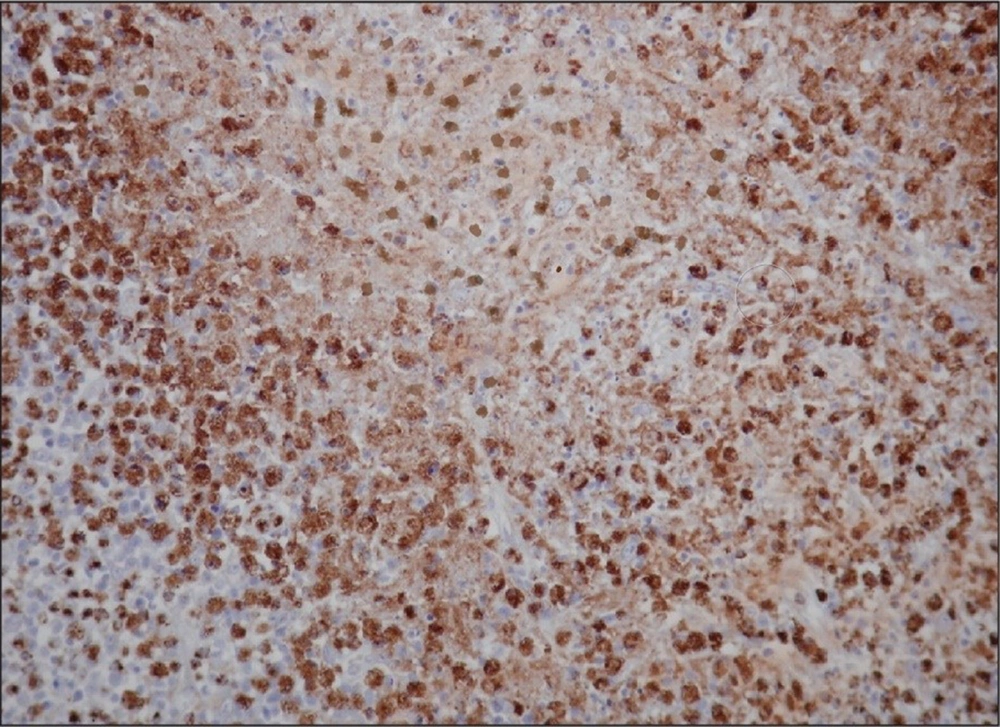
After treatment with broad-spectrum antibiotics, the ESR increased to 100 with WBC: 2600/µL, LDH, and liver enzymes increased, and Ab HCV, Ag HBS, and ANA were negative, so it was recommended to consult with a hematologist to investigate lymphoma, and finally lymph node biopsy was suggested. In the pathology report, the structure of the lymph nodes was severely necrotic, with much karyocardial debris, fibrin deposits, and accumulations of mononuclear cells. Moreover, the number of neutrophils and plasma cells was low, for which necrotizing lymphadenitis (Kikuchis disease) diagnosis was confirmed (Figure 3). According to the pathological results, the patient was prescribed prednisolone, and finally, after 15 days of hospitalization, the patient was discharged.
3. Discussion
The first case of Kikuchi's disease was reported in Kashan, Iran, in 2014 (7, 8), and after that, several cases were reported in different cities across Iran. Most patients were female, except for two studies involving two 16-year-old boys and a 24-year-old man from Mashhad, Iran (9, 10). Our patient was a 30-year-old woman who had no history of the disease and acquired this disease as a result of a Sinopharm vaccine injection. After admission, the patient's ESR increased from 35 to 98. Symptoms of fever, adenopathy, leukopenia, and a high ESR in our patient were unresponsive to antibiotic treatment. KFD was confirmed as a diagnosis in lymph node biopsy after ruling out lymphoma (11).
Kikuchi-Fujimoto disease can generally be considered in patients with long-term fever and cervical lymphadenopathy after ruling out tuberculosis, lymphoma, and autoimmune diseases, especially after COVID-19 vaccination. Lymph node biopsy is the only definite diagnosis of the disease, and most cases are benign and require supportive care. The most striking histological features of KFD are coagulative necrosis, apoptosis associated with karyorrhexis, and marked nuclear and phagocytic activity (12). However, in some cases, laboratory tests have shown reductions in hemoglobin and bilirubin and slight changes in SGOT and SGPT (13).
In another similar study, this disease was observed in an 18-year-old male from Qatar with a history of two episodes of KFD and fever and swelling on the left side of the neck within ten days of receiving the vaccine (11). In addition, KFD after vaccination was reported in a woman, an 18-year-old Asian man without a history of the disease at 35 days, and a 34-year-old man with diabetes and hypertension at 23 days (14-16). In our study, this disease occurred while patients were vaccinated with the Sinopharm vaccine. However, it cannot be said with certainty that this complication is related to the vaccine.
Given that KFD affects cervical lymph nodes with a frequency of 60% - 90%, we can assume that vaccines can be one of the risk factors and inducers of this disease (17). The mechanism of KFD is unclear. However, three main theories have been proposed. The first theory is a viral infection. Several studies have found a link between viral infections (e.g., herpes, Epstein-Barr, and varicella-zoster) and KFD, but no study has found a clear link between them. The second hypothesis is autoimmunity, as KFD leukocytes and macrophages have a tubular network structure similar to SLE. Therefore, one of the important differential diagnoses of KFD is SLE. In addition, there is evidence that patients with a protein genetic element called human leukocyte secondary antigens secondary B cell human leukocyte secondary antigens secondary B-cell (HLA-SB) have a CD8+ T cell-mediated immune response (14). The third hypothesis of intramuscular vaccine injection is that the COVID-19 vaccine may stimulate the production of CD8+ T cells and antibodies, triggering the production of pro-inflammatory factors after injection in the injected area and causing lymph formation. Inflammatory factors irritate the nodes in the injected areas and cause KFD. However, this hypothesis needs further investigation (18-20).
5.1. Conclusions
Kikuchi-Fujimoto disease is an important differential diagnosis for physicians, and they must be careful not to confuse it with lymphoma so that it does not lead to unnecessary treatment. Lymph node biopsy is KFD definite diagnosis. Moreover, health institutions must ensure the effectiveness and safety of vaccines. According to reports, KFD might have occurred in several cases after COVID-19 vaccination, particularly in patients with inflammatory symptoms after vaccination. Consequently, doctors should be aware of this issue and conduct the necessary tests to ensure accurate diagnosis.