1. Background
High sleep quality is one of the important factors in having good health (1). Sleep quality is described as a person's satisfaction with sleep experience, integrating domains of sleep initiation, sleep maintenance, sleep quantity, and refreshment upon awakening (2). Sleep plays an important role in cardiovascular system functioning, and its disruption can cause anxiety, irritability, and anger and increase the heart rate and myocardial oxygen demand (3).
Sleep disorders are one of the most prevalent complications following cardiovascular surgery (4). It is reported that 39 to 69% of patients undergoing open-heart surgery experience sleep disorders within the first month and 50% within 6 months after surgery (1). The results of studies indicate that factors such as anxiety, depression (5), age, sex, hypertension, diabetes, Body Mass Index (BMI) greater than 30, decreased activity level (1), surgical site pain (3), angina pectoris, respiratory problems, myocardial infarction, arrhythmias, inadequate pain relief, and smoking lead to sleep disorders following open-heart surgery (1). Sleep disorders have consequences such as delirium, prolonged stays in hospital, mortality, impaired immune and nervous systems, and delayed healing of wounds (3, 5, 6). Therefore, early diagnosis of sleep disorders is essential to prevent adverse health effects (7).
One way to improve sleep quality in patients after open-heart surgery is to use sleeping medications. However, many sleeping medications can cause side effects such as drug tolerance, dependence, and withdrawal reactions, which can occur after abrupt discontinuation (8). Therefore, studies recently have been conducted on psychological and behavioral approaches that can be an effective alternative to sleeping medications. The literature indicates that these approaches affect primary insomnia and drug-induced insomnia and have long-term effects on sleep latency and sleep quality (9, 10). Cognitive-behavioral therapy (CBT-I) includes several individual components, such as relaxation therapy, sleep restriction therapy, stimulus control, and sleep hygiene guidelines. Paying attention to bad sleeping habits and attitudes is the main goal of CBT-I for sleep disorders because they can lead to poor sleep quality and should be considered in all patients who pose this problem (9, 11). The CBT-I is based on individual cognitive processes that play an important role in behavioral responses among individuals. People can develop cognitive and behavioral skills using cognitive reconstructing processes and training through improving dysfunctional thoughts (12, 13). Individuals are empowered during the CBT-I to increase their ability to cope with stressful situations. The CBT-I is performed interdisciplinary and in the form of individual, group, self-help, and guided interventions (14-16). Critical care nurses (CCNs) have an important role in managing the sleep quality of patients after heart surgery. However, this requires CCNs to be aware of the mechanisms of sleep, sleep problems, and nursing-related assessments so that they can perform individual interventions to promote sleep hygiene. This can affect the sleep quality perceived by patients and reduce the consequences of poor sleep (9). Although CBT-I is a useful solution for insomnia, its application can be limited due to the availability of qualified therapists, delayed response to treatment (compared to non-pharmacological treatments), and difficulty in following a behavioral regimen (sleep restriction and stimulus control).
Pharmacological and behavioral approaches are both effective in treating sleep disorders. However, pharmacological therapy is more commonly used. It should be noted that there are several risks associated with this treatment, including possible side effects, dependence, and drug tolerance. Conversely, available psychological interventions have been shown to lead to long-lasting outcomes without the risks associated with sleeping medications. Also, many patients prefer non-pharmacological treatment regimens (17).
Few studies have been performed on the effects of CBT-I on open-heart surgery patients. The CBT-I seems to be effective in less time than the other psychotherapies. Today, the new health system has changed its direction towards maintaining and promoting health and preventing diseases. Therefore, nurses have more responsibility for health behaviors because the goal of the nursing profession is to help people achieve the desired level of health. Based on the research and experiences of the research team, limited studies have been conducted on the use of nursing-led interventions in sleep disorders after open-heart surgery, and a knowledge gap can be seen in this field. The innovation of the present study is the implementation of CBT-I by a trained CCN with a specialized degree to perform CBT-I.
2. Objectives
The present study was conducted to determine the effect of nurse-led CBT-I intervention on the sleep quality of patients undergoing open heart surgery referred to Kowsar Shiraz Hospital in 2021 - 2021.
3. Methods
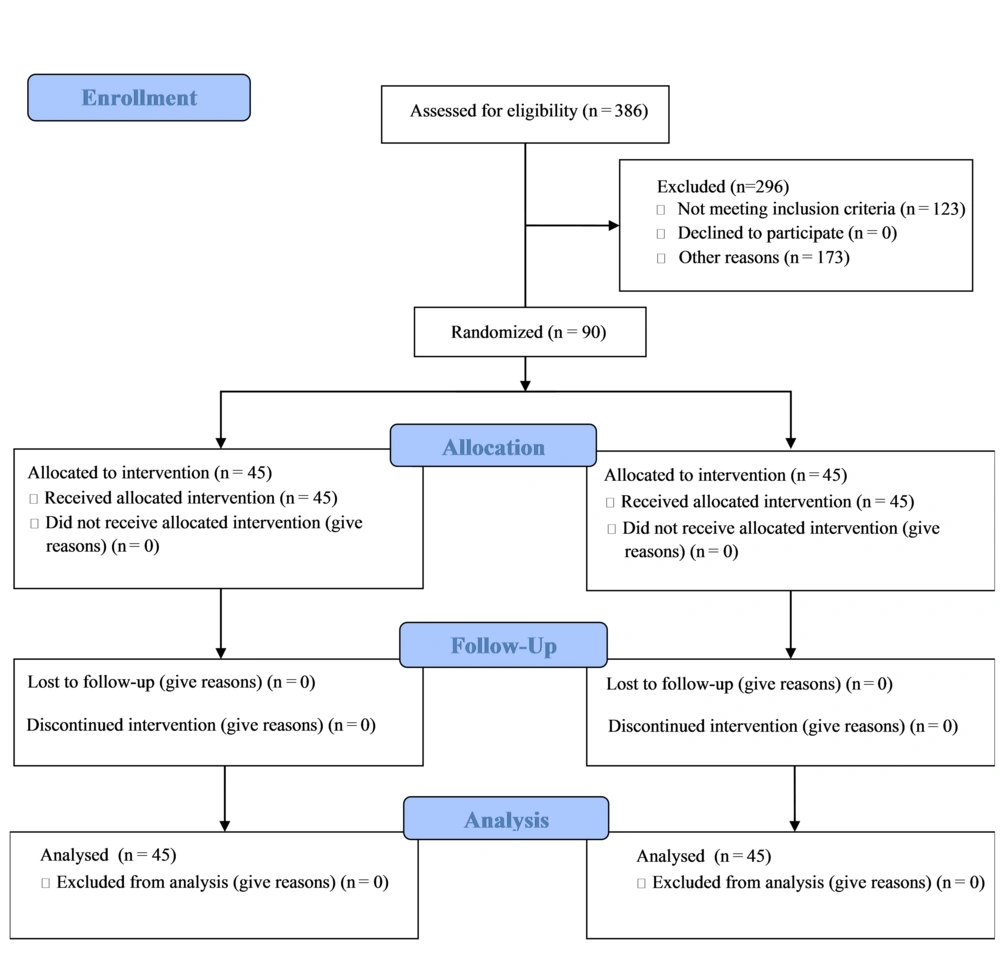
This prospective, single-blind, randomized clinical trial with pre-test-post-test design and parallel groups was performed on 90 patients undergoing open-heart surgery from 2020 to 2021. The study population included all patients undergoing open heart surgery referred to Kowsar Shiraz Hospital. The report of this study is based on the CONSORT checklist (Figure 1).
Based on previous studies (18) and by using the mean comparison formula, α = 0.05, β = 0.2, power = 0.8, S1 = 2.45, S2 = 1.61, d = 1.3 and attrition rate = 10%, the sample size was calculated 45 people in each group.
The inclusion criteria included willingness to participate in the study, ability to participate in therapeutic sessions, reading and writing literacy, age between 20 to 65 years, residence at the study setting, full consciousness and ability to speak Persian, physical and mental readiness to answer questions, and gaining Pittsburgh Sleep Quality Index (PSQI) score > 5. Participating in other educational and treatment classes simultaneously, having a specific mental illness before surgery (according to the patient's report), and having other illnesses such as malignancies or autoimmune disorders (according to the patient's report) were considered the main conditions for not including the study.
The exclusion criteria also included exposure to specific psychological crises during the work process, initiation of other psychiatric treatments (according to the patient's report or doctor's order), the need for readmission to the hospital, and missing more than 3 sessions to perform the intervention.
Each of the final samples was given a code from one to 90 (sample volume number). Then, using R software and sample command, 45 codes out of 90 codes were randomly allocated to the intervention group, and the rest of the codes represented the codes of the samples in the control group.
For blinding in the present study, the referral days of patients in the intervention group to receive counseling were considered different from the referral days of patients in the control group.
After obtaining permission, the researcher visited the study setting. She introduced herself, explained the objectives of the study, and obtained the consent of the relevant authorities.
Patients were admitted to the intensive care unit 1 to 2 days before heart surgery for necessary measures. During the preoperative period, patients who met the inclusion criteria were interviewed, and their oral and written consent to be included in the study was obtained. The PSQI tool was used for measuring sleep quality among patients. If a patient did not have a sleep disorder in the initial interview based on this instrument, a second interview would be performed 4 to 5 weeks after discharge. If the patient had sleep disorders in the second interview, he or she would be randomly assigned to one of the 2 intervention or control groups. The intervention group includes people who have developed sleep disorders after surgery, for whom, in addition to the usual care of the treatment center, the CBT-I protocol was also considered (19, 20). The control group included people who developed sleep disorders after surgery but only received the usual post-operative cardiac care at the hospital. Usual care included routine medical and nursing follow-up after heart surgery, which was mostly done to resolve patients' physical problems. The patient's mental status was not usually evaluated by a psychiatrist unless advised by a heart surgeon.
The CBT-I protocol was administered at a time and place previously coordinated with the patient by a trained and certified critical care nurse (researcher 2). Weekly sessions followed a standard format, including mood review, cross-programming, discussion, assignments, and feedback. Table 1 presents the weekly schedule:
| Content | Education Method | Duration of Sessions (h) | Place of Sessions | Instructor | Number of Sessions (Week) |
|---|---|---|---|---|---|
| Applying therapeutic communication, setting the agenda, identifying problems objectively, and setting intervention goals | Individually and face-to-face | 1 | Counseling room of Cardiac Surgery Department of Kowsar Kowsar Hospital, Shiraz | Master of Critical Care Nursing with a CBT degree | 1th |
| Increasing patients' knowledge, activating behavioral functions and problem-solving methods | 2th | ||||
| Identifying automatic thoughts, improving problem-solving skills, reducing dysfunctional cognitive processes on behavior | 3 - 4th | ||||
| Reconstructing automatic thoughts, identifying abilities, and learning self-healing techniques | 5 - 6th | ||||
| Continuing self-medication and preventing a recurrence | 7 - 8th | ||||
| Training to improve skills related to self-care in the field of the disease and increasing acceptable, enjoyable activities according to the condition of the disease, ending the intervention, terminating the therapeutic relationship | 9 - 10th |
In this intervention, 2 extra sessions were considered for completing the questionnaire or if some sessions needed to be longer and required to continue the intervention. After 10 - 12 sessions of CBT-I treatment in the intervention group, both intervention and control groups were reevaluated with the instrument. To consider the ethical principles, we administered a complete course of nurse-led CBT-I for the control group after the end of the study. To prevent the exchange of information between the intervention group and the control group and to prevent data contamination, we invited the patients in the control group on the first three days of the week and the patients in the intervention group on the second three days of the week.
Demographic data and PSQI were used to collect data. The demographic information questionnaire includes information about age, sex, duration of cardiopulmonary bypass, type of surgery, length of hospital stays, history of diabetes and hypertension, BMI, use of diuretics, smoking, and participation in sports programs, and ejection fraction (EF) of patients.
The PSQI, which is one of the best tools designed to measure sleep quality, was used to measure sleep quality. This questionnaire was developed in 1988 by Dr. Buysse et al. at the Pittsburgh Institute of Psychiatry. This questionnaire includes 19 self-rated items and 7 components: Subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction. Each item is scored on a 0-3 Likert scale. In all items, a score of "0" indicates no difficulty, and a score of "3" indicates severe difficulty. The total sleep quality score is calculated from the sum of the scores of 7 components (0 to 21). A PSQI score higher than 5 indicated poor sleep quality, whereas a PSQI score equal to or lower than 5 indicated good sleep quality (21-23). Buysse et al., who designed this questionnaire, obtained the internal consistency of the questionnaire using Cronbach's alpha of 0.83 (23). In Farrahi Moghaddam et al.'s study, the validity and reliability of the Iranian version of this questionnaire were confirmed (a = 0.77) (24). In the present study, the internal consistency method was used to evaluate the reliability of the questionnaire. Cronbach's alpha coefficient of PSQI was 0.716 and had appropriate reliability.
In the present study, the nurse-led CBT-I and sleep quality were independent and dependent variables, respectively. SPSS v. 22 (IBM Corp., Armonk, NY, USA) was used to analyze collected data, and descriptive statistics such as frequency, percentage, mean, and standard deviation were utilized to describe the characteristics of the data. Kolmogorov-Smirnov and chi-square (X2) tests were used to investigate normal distribution in quantitative variables and analyze demographic information, respectively. Independent sample t-test was used to compare the mean sleep quality score between the 2 groups before the intervention, and the paired t-test was applied to compare the mean sleep quality before and after the intervention in each group. Analysis of covariance (ANCOVA) was used to compare the mean score of sleep quality after the intervention in the 2 groups under study. The significance level was considered less than 0.05 (P < 0.05).
4. Results
Participants in the 2 groups were homogeneous in terms of demographic data, and no statistically significant difference was observed between the 2 groups (P > 0.05). The majority of the participants in the study were in the age range of 31-40 years (33.33%), male (53.33%), and had a left ventricular EF of less than 40% (70%). Fifty-three subjects underwent coronary artery surgery (58.88%). Thirty-five subjects (38.88%) stayed in the hospital for less than 5 days. The demographic characteristics of the samples are presented in Table 2.
| Variables and Groups | Control | Intervention | P-Value a |
|---|---|---|---|
| No. (%) | No. (%) | ||
| Age (y) | 0.643 | ||
| 20 - 30 | 12 (26.7) | 9 (20.0) | |
| 31 - 40 | 13 (28.9) | 17 (37.8) | |
| 41 - 50 | 10 (22.2) | 7 (15.6) | |
| 51 - 65 | 10 (22.2) | 12 (26.7) | |
| Sex | 0.673 | ||
| Female | 20 (44.4) | 22 (48.9) | |
| Male | 25 (55.6) | 23 (51.1) | |
| HTN | 0.091 | ||
| Yes | 17 (37.8) | 25 (55.6) | |
| No | 28 (62.2) | 20 (44.4) | |
| Diabetes | 0.056 | ||
| Yes | 30 (66.7) | 21 (46.7) | |
| No | 15 (33.3) | 24 (53.3) | |
| Smoking | 0.671 | ||
| Yes | 21 (46.7) | 19 (42.2) | |
| No | 24 (53.3) | 26 (57.8) | |
| EF | 0.818 | ||
| 40% ≥ | 13 (28.9) | 14 (31.1) | |
| 40% < | 32 (71.1) | 31 (68.9) | |
| Diuretic use | 0.396 | ||
| Yes | 9 (20.0) | 6 (13.3) | |
| No | 36 (80.0) | 39 (86.7) | |
| Activities and exercise | 0.671 | ||
| Yes | 19 (42.2) | 21 (46.7) | |
| No | 26 (57.8) | 24 (53.3) | |
| Cardiac bypass duration (h) | 0.911 | ||
| Less than 1 | 19 (42.2) | 17 (37.8) | |
| 1 - 2 | 15 (33.3) | 16 (35.6) | |
| More than 2 | 11 (24.4) | 12 (26.7) | |
| Length of hospital stay (days) | 0.710 | ||
| Less than 5 | 16 (35.6) | 19 (42.2) | |
| 5 - 10 | 17 (37.8) | 17 (837) | |
| More than 10 | 12 (26.7) | 9 (20.0) | |
| Type of surgery | 0.950 | ||
| Coroner | 26 (57.8) | 27 (60.0) | |
| Valve | 15 (33.3) | 15 (33.3) | |
| Both | 2 (4.4) | 2 (4.4) | |
| BMI | 0.308 | ||
| Less than 18.5 (underweight) | 10 (22.2) | 5 (11.1) | |
| 5.9 - 18.24 (normal weight) | 14 (31.1) | 16 (35.6) | |
| 25.9 - 29 (overweight) | 16 (35.6) | 14 (31.1) | |
| More than 30 (obese) | 5 (11.1) | 10 (22.2) |
Abbreviations: EF, ejection fraction; BMI, Body Mass Index; HTN, hypertension.
a Chi-square test.
The results of the independent t -test showed that the mean score of subjective sleep quality in the 2 groups before the intervention had a statistically significant difference (P = 0.003). The results of ANCOVA showed that the mean score of subjective sleep quality after the intervention has a significant difference in the 2 groups (P = 0.0001) and is higher in the control group. The results of the paired t-test showed that the changes in the subjective sleep quality score were significant in the 2 groups, but in the control group, it increased, and in the intervention group, it decreased (Table 3).
| Components and Group | Before | After | Difference | P-Value | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SE | Mean | SD | ||
| Subjective sleep quality | |||||||
| Control | 0.911 | 0.51 | 1.44 | 0.54 | -0.53 | 0.69 | 0.0001 |
| Intervention | 1.311 | 0.7 | 0.2 | 0.40 | 1.11 | 0.64 | 0.0001 |
| P-value | 0.003 | 0.0001 a | |||||
| Sleep latency | |||||||
| Control | 1.97 | 0.83 | 2.55 | 0.54 | -0.57 | 0.83 | 0.0001 |
| Intervention | 2.22 | 0.70 | 0.911 | 0.55 | 1.31 | 0.51 | 0.0001 |
| P-value | 0.138 | 0.0001 | |||||
| Sleep duration | |||||||
| Control | 4.66 | 1.60 | 4.17 | 1.09 | 0.48 | 1.53 | 0.038 |
| Intervention | 5.71 | 1.77 | 7.2 | 0.66 | -1.48 | 1.73 | 0.0001 |
| P-value | 0.004 | 0.0001 a | |||||
| Habitual sleep efficiency | |||||||
| Control | 75.73 | 10.37 | 79.11 | 8.55 | -3.37 | 13.70 | 0.105 |
| Intervention | 80.68 | 7.09 | 91.29 | 5.85 | -10.61 | 9.09 | 0.0001 |
| P-value | 0.01 | 0.0001 a | |||||
| Sleep disturbances | |||||||
| Control | 12.13 | 2.54 | 16.37 | 2.36 | -4.24 | 1.82 | 0.0001 |
| Intervention | 12.95 | 4.67 | 6.04 | 4.03 | 6.91 | 5.75 | 0.0001 |
| P-value | 0.303 | 0.0001 | |||||
| Use of sleeping medication | |||||||
| Control | 0.311 | 0.63 | 1.06 | 0.75 | -0.75 | 0.77 | 0.0001 |
| Intervention | 1.33 | 1.08 | 0.55 | 0.69 | 0.77 | 1.20 | 0.0001 |
| P-value | 0.0001 | 0.0001 a | |||||
| Daytime dysfunction | |||||||
| Control | 3.4 | 1.009 | 3.06 | 1.45 | 0.33 | 1.44 | 0.129 |
| Intervention | 3.55 | 1.53 | 1 | 1.08 | 2.55 | 1.53 | 0.0001 |
| P-value | 0.571 | 0.0001 | |||||
| Total PSQI | |||||||
| Control | 10.31 | 2.18 | 12.53 | 2.09 | -2.22 | 2.2 | 0.0001 |
| Intervention | 10.93 | 2.81 | 3.8 | 1.68 | 7.13 | 2.94 | 0.0001 |
| P-value | 0.245 | 0.0001 | |||||
Abbreviation: PSQI, Pittsburgh Sleep Quality Index.
a ANCOVA.
The results of the independent t test showed that the mean score of sleep latency in the 2 groups before the intervention did not have a statistically significant difference (P = 0.138). Also, the mean score of sleep latency after the intervention has a significant difference in the 2 groups (P = 0.0001) and is higher in the control group. The results of the paired t-test showed that the changes in the sleep latency score were significant in the 2 groups, but in the control group, it increased, and in the intervention group, it decreased (Table 3).
The results of the independent t-test showed that the mean score of sleep duration in the 2 groups before the intervention had a statistically significant difference (P = 0.004). Also, the results of ANCOVA showed that the mean score of sleep duration after the intervention has a significant difference in the 2 groups (P = 0.0001) and is lower in the control group. The results of the paired t -test showed that the changes in the sleep duration score were significant in the 2 groups, but in the control group, it decreased, and in the intervention group, it increased (Table 3).
The results of the independent t-test showed that the mean score of habitual sleep efficiency in the 2 groups before the intervention had a statistically significant difference (P = 0.01). The results of ANCOVA showed that the mean score of habitual sleep efficiency after the intervention has a significant difference in the 2 groups (P = 0.0001) and is lower in the control group. The results of the paired t-test showed that the changes in habitual sleep efficiency score were significant in both groups, but the increase was greater in the intervention group (Table 3).
The results of the independent t test showed that the mean score of sleep disturbances in the 2 groups before the intervention had no statistically significant difference (P = 0.303), and the mean score of sleep disturbances after the intervention had a significant difference in the 2 groups (P = 0.0001) and is more in the control group. The results of the paired t-test showed that the changes in the sleep disturbances score were significant in the 2 groups, but in the control group, it was increasing, and in the intervention group, it was decreasing (Table 3).
The results of the independent t test showed that the mean score of the use of sleeping medication in the 2 groups before the intervention had a statistically significant difference (P = 0.0001). Also, the results of ANCOVA showed that the mean score of use of sleeping medication after the intervention has a significant difference in the 2 groups (P = 0.0001) and is higher in the control group. The results of the paired t-test showed that the changes in the score of use of sleeping medication in the 2 groups were significant, but in the control group, it was increasing, and it was decreasing in the intervention group (Table 3).
The results of the independent t test showed that the mean score of daytime dysfunction in the 2 groups before the intervention had no statistically significant difference (P = 0.571); the mean score of daytime dysfunction after the intervention had a significant difference in the 2 groups (P = 0.0001) and was more in the control group. The results of the paired t-test showed that the changes in the daytime dysfunction score in the intervention group were significant and decreased (Table 3).
The results of the independent t test showed that the mean total PSQI score in the 2 groups before the intervention had no statistically significant difference (P = 0.245); the mean total PSQI score after the intervention had a significant difference in the 2 groups (P = 0.0001) and was more in the control group. The results of the paired t-test showed that the changes in total PSQI score are significant in 2 groups, but in the control group, they are increasing, and in the intervention group, they are decreasing (Table 3).
5. Discussion
This study aimed to determine the effect of CBT-I on sleep quality among patients undergoing open-heart surgery.
Our results confirmed the hypothesis of the study and showed that nurse-led CBT-I affects sleep quality among patients undergoing open-heart surgery.
In a meta-analysis evaluating the association between sleep disorders and cardiovascular disease, the presence of insomnia was found to increase the risk of death from cardiovascular disease (25). The results of a study indicated that the prevalence of insomnia among patients undergoing open-heart surgery is higher than among patients undergoing coronary interventions such as angioplasty (26).
The CBT-I is an effective non-pharmacological approach to increase sleep quality that is performed individually or in groups. It includes educational, behavioral, and cognitive components. The educational part attempts to improve understanding of the basic principles of sleep regulation, good sleep hygiene, and etiological factors of sleep disorders. The behavioral component consists of relaxation techniques that can reduce stress and anxiety and other techniques that increase sleep quality through adjusting sleep patterns. The cognitive component tries to cure dysfunctional sleep beliefs and attitudes that may cause sleep anxiety or lead to maladaptive sleep patterns (27).
Based on the findings of the current study, after performing CBT-I, subjective sleep quality, sleep duration, and habitual sleep efficiency increased in the experimental group compared to the control group. Also, in the experimental group, sleep latency, sleep disturbances, use of sleeping medication, and daytime dysfunction were lower than in the control group.
However, too little attention has been paid to investigating the effectiveness of nurse-led CBT-I on sleep quality among patients after open-heart surgery. The following are the results of some studies that have used CBT-I to improve sleep quality. In Williams-Cooke's study, CBT-I in people with multiple sclerosis did not show a significant reduction in sleep latency (28), which is inconsistent with the results of the present study. The contradictory results can be justified based on the small sample size or comorbid problems often experienced by people with multiple sclerosis (such as pain, fatigue, and spasticity), which may affect sleep outcomes.
In Bensen-Boakes's study, CBT-I improved habitual sleep efficiency in people with comorbid insomnia and sleep apnea, but the difference between the experimental and control groups was not significant (29), which does not support the results of the present study. Polysomnography studies in wait-list samples may highlight sleep variables and affect their subjective responses over time.
Javaheri et al. examined the effectiveness of CBT-I on sleep quality among people with coronary artery disease. Web-based CBT-I was performed on 24 subjects for 6 weeks (42 days). They acknowledged that CBT-I is effective in enhancing sleep quality among subjects (30). The findings of this study are in line with their study. In the above study, despite the use of a small sample size in this program, a statistically significant improvement in sleep latency and efficiency was observed in the intervention group. One of the benefits of web-based CBT-I is its flexibility and ease of use.
Heenan et al. investigated the effect of CBT-I in 6 sessions on 47 people with cardiovascular disease in groups of 6 to 12 people. The results of this study showed that after group intervention, the total sleep duration and efficiency significantly increased, and sleep latency and sleep quality improved. However, it did not have a significant effect on the duration or frequency of naps. They also reported that people with cardiovascular disease experienced significantly fewer symptoms of anxiety, depression, and insomnia following CBT-I (31). The results of the above study support our findings, but this study differed from our study in terms of the tools used to assess sleep quality, lack of control group, number of samples, intervention method, and number of CBT-I sessions.
The findings of the current study are consistent with those of Lai et al., who showed that at the end of the first and third months after CBT-I with coping management among patients with breast cancer, sleep quality increased, anxiety and depression symptoms decreased, and life quality improved (32).
The results of this study confirm those of Farrokhi et al., who reported that CBT-I was effective in enhancing the elderly sleep quality. In their study, CBT-I was performed in 6 sessions of 90 minutes by a clinical psychologist (33). their study was performed on male elderly, and this limits the possibility of generalizing the results to female elderly.
The findings of the current study are consistent with those of Li et al., who showed that CBT-I improves sleep quality in patients with hypertension (34).
Based on the results of the present study, a decrease in overall sleep quality score after CBT-I in the experimental group compared to before indicated an improvement in sleep quality and effectiveness of CBT-I, which is consistent with those of some studies (10, 35).
Also, comparing the overall score of sleep quality in the current study before and after CBT-I in the control group showed that the mean total score of sleep quality after the intervention was higher than before, and this difference was statistically significant, which indicated a decrease in sleep quality among the control group. This finding is consistent with that of Lai et al. study (32). This finding explains that in the control group, CBT-I was not performed, and this issue can confirm the effectiveness of CBT-I.
One of the limitations of the present study is the lack of long follow-up of the samples participating in the study after CBT-I. It is suggested that in future studies, the sleep quality of these patients be monitored for a longer time. The heterogeneity of the samples in the experimental and control groups in terms of components of subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, and use of sleeping medication before the intervention were other limitations of the present study that were removed by using ANCOVA.
5.1. Conclusions
The results of the present study showed that nurse-led CBT-I improves sleep quality among patients undergoing open-heart surgery and can be applied as an effective intervention. The results can be used to familiarize and inform specialized nurses, physicians, and psychologists who are involved in this subject. Due to the interdisciplinary nature of this intervention between nursing and psychiatry and patients' needs for cognitive-behavioral rehabilitation, it is recommended that the training of nurse-led CBT-I be included in the academic training program for nurses. Furthermore, the conditions for participating in CBT-I programs in continuing education programs for nurses working in heart surgery wards should be prepared to enable them to perform this effective intervention after heart surgery in the required situations.