1. Context
Nowadays, developing strategies to improve the quality of care plays a vital role in international health policies. This factor has prompted governments to improve the quality of care. The four components of quality, from the perspective of the World Health Organization, which are the basis for the formation of clinical service support are professional performance (technical quality), resource use (productivity), patient satisfaction with the services provided, and risk management (risk of injury or illness in connection with the services provided) (1).
Risk management in health care refers to a diverse group of measures performed to improve the quality and ensure the safety of services for patients. The daily concern of high-risk organizations, including hospitals, is the management of unexpected events (2). Risk management is crucial in improving health care quality, effective communication between hospital staff and patients, patient desirability, and Limiting abortion practices in hospitals (3, 4). In the past, risk management in clinical settings was examined with a reactive view. In other words, risk management was performed after the incident, and its causes and factors were analyzed to prevent its recurrence. However, nowadays, the emphasis is on the active method in which risk probability is accepted and managed adequately before the threat occurs (5).
Studies showed that the operating room is only a small part of the total hospital in terms of physical space, comprising less than 4% of the total hospital space and less than 3% of the total hospital staff, but 35% of the complaints related to risks related to the operating room (6). Other studies reported that the risk rate in the operating room is 71.8% and more than 50 unknown types (7). Therefore, risk management in the operating room should be prioritized over other hospital sections. About 234 million surgeries are performed annually worldwide (8, 9). Using a systematic and comprehensive method in surgical departments to prevent the possibility of error will bring good results. However, even in industrialized countries, error prevention is not done properly (10). Surgery is an important healthcare service accounting for 40% of hospital costs. Also, due to the higher probability of error in the operating room and its consequences for patients, the performance of this department is very effective in assessing the quality of services provided to patients and their satisfaction (11, 12). The high error rate in intensive care units, operating rooms (ORs), and emergency departments might be explained by the complex nature of the operation (13). Among the above-mentioned healthcare facilities, operating rooms are more concerned with high-risk operations. Therefore, errors are more likely for patients and staff in operating rooms (14). These errors are classified into eight general themes: Operational risks, technology, legal, human capacity, financial, strategic, clinical, and patient safety and risk (15).
Errors and adverse events occur due to inefficient management and other technical, human, and organizational inadequacies (e.g., lack of proper communication and training and insufficient standard methods). These cases have led to issues such as wrong place surgery and wrong anesthesia management, which are significant in operating rooms and endanger patients’ lives and impose huge costs on healthcare systems (14). Among other incidents in the operating room, we can mention the possibility of physical damage due to electric shock, burns, fire, contact with blood products, and inhalation of toxic substances. Some devices used in the operating room, such as lasers, radiography equipment, and chemical sterilizers, can also lead to long-term damage if the staff is careless in the security field (16). Therefore, some effective factors in the occurrence of medical errors in the operating room can be prevented, reducing errors and adverse operating room accidents and leading to increased quality of care (14).
2. New Contributions
Numerous studies have used different models for risk management in the operating room. In Guo’s study, for risk management in the operating room, a risk quantification matrix and a risk registration form were implemented to identify potential hazards, and then policies were designed and implemented to reduce or eliminate these hazards (17). A counseling mechanism and risk monitoring system were also used to minimize risks among operating room nurses (17). In a study by DeRosier et al. on operating room risk management, a surgical risk assessment model was implemented using failure modes and effects analysis (FMEA), and multi-objective optimization based on analysis was presented (18). This work aimed to determine the most important risk points during the surgical process and analyze the relevant solutions (18). So far, no study has attempted to provide a comprehensive picture of the characteristics of risk management programs implemented in different countries. Therefore, this study aimed to implement a scoping review approach to analyze and review the characteristics of risk management programs implemented in the operating room of hospitals in various countries worldwide. Our results will provide a comprehensive picture of this program to help develop a risk management program in the operating room of hospitals.
3. Evidence Acquisition
In this study, we used Arksey and O’Malley’s framework (19). The framework includes six steps: Identifying the research question, identifying relevant studies, selecting/screening studies, scaling/segmenting data, summarizing, reporting results, and optional consultation with experts on findings. The detailed explanation of the six main steps is as follows:
(1) Identifying the research question: Like systematic review studies, in this method, the starting point is identifying the research question on which search strategies are built. The study question is: What are the characteristics of risk management programs implemented in the operating room of hospitals in various countries worldwide?
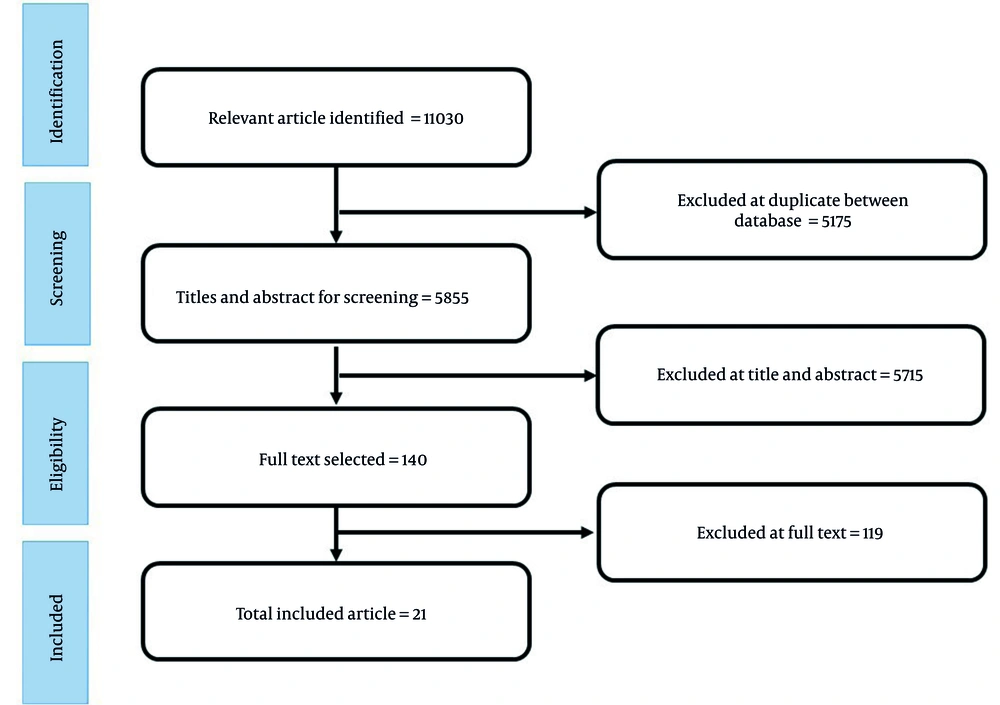
(2) Identification of related studies: The scoping review focuses on identifying the original studies (published and gray studies) and appropriate review studies to answer the main research question as comprehensively as possible. In the present study, appropriate keywords and their combination, such as proactive risk management (PRM), proactive risk assessment, risk management, health systems, hospitals, operating room, objectives, steps, components, outcomes, facilitators, and prerequisites, were searched in various databases such as Web of Knowledge, PubMed, Scopus, Cochrane, Springer, ProQuest, Iranian databases, including SID, Magiran, and Google search engine. All published articles and reports in this field were selected. The search was done on December 21, 202. In addition to manually searching the journals and sources of selected articles, organizational reports, published government documents, websites, and other available information and gray resources were also reviewed. Based on the search, about 11,030 related articles were obtained (Figure 1).
(3) Selection/screening of studies: All stages of selection and screening of articles were performed separately by two research team members. Disputes were resolved through discussion, and if necessary, they were referred to a third party with more information and experience. First, the titles of all studies reviewed and articles inconsistent with the study’s objectives were removed. In the following steps, the abstract and full text of the articles were reviewed to exclude studies that met exclusion criteria and had poor relevance to study objectives. This study was performed without a time limit and with the following inclusion and exclusion criteria. Inclusion criteria included studies that reviewed the risk management program in health systems. Exclusion criteria included studies conducted outside the health system and non-English and Persian articles. Out of 11,030 articles in this study, about 5,175 were removed due to duplication. Also, 5,715 articles were removed due to the mismatch of the title and abstract of the article with the main purpose. Likewise, about 119 articles were removed due to the mismatch of the article’s main text with the main objective; finally, 21 articles were extracted (Figure 1).
(4) Data segmentation: This stage arranges key items from the reviewed reports. The results of the selected studies were managed through a data extraction form designed by the research team, including the authors, year of publication, type of risk, purpose, steps, and components of risk management. Two people independently extracted the information from the selected articles, and the ambiguities were resolved in consultation with other research team members.
(5) Summarizing and reporting the results: The results were analyzed using thematic analysis. This way, a preliminary study was conducted to identify the extracted studies. As a result, a thematic framework based on codes specific to the studies was designed. Another researcher reviewed each study, and the findings were extracted in specific codes. In the next step, the main themes were extracted following the semantic framework and connection and sometimes integration between codes, and the findings were organized within the main themes. Finally, after ensuring the validity of the main themes, they were organized based on their fit with the main research question of the category and then presented in the form of a table of findings.
(6) Presenting practical tips and recommendations: After performing the previous steps, based on the extracted data and the opinions of the research team members, tips and recommendations were made in the form of article discussion and knowledge translation.
4. Results
Based on the presented framework, six main themes of findings were extracted, including objectives, components, steps, results, prerequisites, and facilitators of the risk management program. The goals of the risk management program included seven sub-themes: Quality improvement, safety improvement, cost reduction, satisfaction increase, risk prevention and reduction, financial loss protection, and risk eradication. Among these goals are risk eradication with 62%, safety improvement with 57%, quality improvement and prevention and reduction of risks with 52%, protection of financial losses with 14%, reduction of costs with 10%, and increase of satisfaction with 5%, which are the most frequent purposes among the articles (Table 1).
| No. | Author Name and Year of Publication | Country | Error Type | Risk Management Model | Objectives of the Risk Management Program | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Quality Improvement | Safety Promotion | Reduction of Costs | Increasing Satisfaction | Prevention and Reduction of Risks | Protecting Financial Losses | Rooting the Risks | |||||
| 1 | Sayed et al., 2013 (20) | Egypt | Any kind of error | WHO safety guidelines | * | * | |||||
| 2 | Guo, 2015 (17) | China | Any kind of error | AS-NZS4360 risk management standards | * | * | * | ||||
| 3 | van Beuzekom et al., 2012 (21) | Netherlands | Any kind of error | The Leiden Operating Theatre and Intensive Care Safety (LOTICS) scale | * | * | * | ||||
| 4 | Schimpff,2007 (22) | USA | Any kind of error | Root-cause analyses | * | * | |||||
| 5 | Borie et al., 2018 (23) | France | Fire and burns | Root-cause analyses | * | * | * | * | |||
| 6 | Frabetti et al., 2005 (24) | Italy | Microbiological risk | Root-cause analyses | * | * | * | ||||
| 7 | Amghar et al., 2017 (25) | Morocco | Surgical infection, surgical foreign body, medication error, equipment failure, operation error, patient injury, wrong location | The Fuzzy Bayesian Network Model | * | * | |||||
| 8 | Silen-Lipponen et al., 2005 (26) | Finland, the USA, and the UK | Human errors | Failure mode and effect analysis | * | ||||||
| 9 | Pomerantz et al., 2011 (27) | USA | Risks associated with skin surgery patients | Failure mode and effect analysis | * | * | * | ||||
| 10 | DeRosier et al., 2019 (18) | USA | Errors related to the process of selection and implantation of intraocular lens (IOL) | Healthcare failure mode and effect analysis | * | * | * | ||||
| 11 | Kavosi et al., 2017 (28) | Iran | Any kind of error | Failure mode and effect analysis | * | * | |||||
| 12 | Le Bourg and Gallois, 2011 (29) | French | Any kind of error | - | * | * | * | ||||
| 13 | Lepanluoma et al., 2014 (30) | Finland | Errors related to the neurosurgery patients | WHO surgical safety guidelines | * | * | |||||
| 14 | American College of Obstetricians and Gynecologists, 2010 (31) | USA | Any kind of error | Universal protocol for preventing wrong site, wrong procedure, and wrong person surgery - WHO surgical safety guidelines | * | ||||||
| 15 | American Society of Anesthesiologists Task Force on Operating Room Fires et al, 2008 (32) | USA | Operating room fire | Practice Advisory for the Prevention and Management of Operating Room Fires | * | * | |||||
| 16 | Bower, 2002 (33) | USA | Any kind of error | Another department’s successful program as a model | * | * | * | * | * | ||
| 17 | McLain, 1980 (34) | USA | Medical mismanagement, diagnostic and treatment problems, inadequate procedures, equipment failure | Liability control systems | * | * | * | ||||
| 18 | Alfredsdottir and Bjornsdottir, 2008 (35) | Iceland | Any kind of error | Root-cause analyses | * | * | |||||
| 19 | Tabibzadeh and Jahangiri, 2018 (14) | USA | Any kind of error | Rasmussen’s framework | * | * | |||||
| 20 | Guedon et al., 2014 (36) | Netherlands | Equipment accidents | Safety status system for operating room devices | * | * | |||||
| 21 | Frosini et al., 2016 (37) | Italy | Any kind of error | Web-based monitoring system | * | * | * | ||||
The components of the risk management program include six sub-themes: Resources, leadership, organizational culture, communication, monitoring, and training. Among these components, communication (57%), supervision (52%), resources (43%), leadership (33%), organizational culture (24%), and education (19%) were the most frequent risk management components among the articles (Table 2).
| No. | Author Name and Year of Publication | Components of the Risk Management Program | |||||
|---|---|---|---|---|---|---|---|
| References | Leadership | Organizational Culture | Connections | Monitoring | Education | ||
| 1 | Sayed et al., 2013 (20) | * | * | ||||
| 2 | Guo, 2015 (17) | * | * | ||||
| 3 | van Beuzekom et al., 2012 (21) | * | * | ||||
| 4 | Schimpff, 2007 (22) | * | * | * | * | * | |
| 5 | Borie et al., 2018 (23) | * | * | ||||
| 6 | Frabetti et al., 2005 (24) | * | * | ||||
| 7 | Amghar et al., 2017 (25) | * | |||||
| 8 | Silen-Lipponen et al., 2005 (26) | * | * | ||||
| 9 | Pomerantz et al., 2011 (27) | * | * | ||||
| 10 | DeRosier et al., 2019 (18) | * | * | * | |||
| 11 | Kavosi et al., 2017 (28) | * | * | * | |||
| 12 | Le Bourg and Gallois, 2011 (29) | * | * | ||||
| 13 | Lepanluoma et al., 2013 (30) | * | * | ||||
| 14 | American College of Obstetricians and Gynecologists, 2010 (31) | * | * | * | |||
| 15 | American Society of Anesthesiologists Task Force on Operating Room Fires et al., 2008 (32) | * | |||||
| 16 | Bower, 2002 (33) | * | * | ||||
| 17 | McLain, 1980 (34) | * | * | * | * | ||
| 18 | Alfredsdottir and Bjornsdottir, 2008 (35) | * | * | * | |||
| 19 | Tabibzadeh and Jahangiri, 2018 (14) | * | |||||
| 20 | Guedon et al., 2014 (36) | * | * | ||||
| 21 | Frosini et al., 2016 (37) | * | * | ||||
The stages of the risk management program include four main models; model 3 (57%) and models 1, 2, and 4 (14%) were the most frequent risk management steps among the articles (Table 3). The results of the risk management program include four sub-themes consisting of identifying the main causes of errors, achieving effective methods in reporting errors, achieving effective methods in reducing errors, and the need for informed consent. Achieving effective methods in reducing errors (57%), achieving effective methods in reporting errors (38%), identifying the main causes of errors (24%), and the need for informed consent (5%) were the most common types of the risk management program among the articles (Table 4).
| No. | Author Name and Year of Publication | Steps for Implementing Risk Management | |||
|---|---|---|---|---|---|
| 1- Creating an Environment 2- Risk Identification 3- Risk Analysis 4- Risk Assessment 5- Risk Elimination 6- Creating a Communication and Advisory Mechanism 7- Creating a Monitoring and Evaluation Mechanism (Model 1) | 1- Selecting the High-risk Section 2- Selecting the Team 3- Drawing Process Diagrams 4- Precipitation of Possible Error Modes and Determining the Effects of Error Modes 5- Prioritizing Error Modes Based on Severity and Probability 6- Identifying the Root Causes of Error Modes 7- Documenting Any Control Measures and Corrective Measures (Model 2) | 1- Preoperative Evaluation (Log in) 2- Evaluation During Surgery 3- Postoperative Evaluation (Logout) (Model 3) | 1- Checking Equipment, Physical Conditions, Environment, Policies, and Procedures to Expose Hazardous Conditions 2- Emphasizing the Safe Operation of Equipment and Preventive Maintenance Plan 3- Early Notification of Preventive Plan Before the Crisis 4- Creating Reporting Channels, Reporting Format, Review, and Timely Documentation and Timely Routing of Error Reports 5- Extensive Internal Training for All Operating Room Staff 6- Finally, Consultation with Operating Room Surgeons (Model 4) | ||
| 1 | Sayed et al., 2013 (20) | * | |||
| 2 | Guo, 2015 (17) | * | |||
| 3 | van Beuzekom et al, 2012 (21) | * | |||
| 4 | Schimpff, 2007 (22) | * | |||
| 5 | Borie et al., 2018 (23) | * | |||
| 6 | Frabetti et al., 2005 (24) | * | |||
| 7 | Amghar et al., 2017 (25) | * | |||
| 8 | Silen-Lipponen et al., 2005 (26) | * | |||
| 9 | Pomerantz et al., 2011 (27) | * | |||
| 10 | DeRosier et al., 2019 (18) | * | |||
| 11 | Kavosi et al., 2017 (28) | * | |||
| 12 | Le Bourg and Gallois, 2011 (29) | * | |||
| 13 | Lepanluoma et al., 2013 (30) | * | |||
| 14 | American College of Obstetricians and Gynecologists, 2010 (31) | * | |||
| 15 | American Society of Anesthesiologists Task Force on Operating Room Fires et al., 2008 (32) | * | |||
| 16 | Bower, 2002 (33) | * | |||
| 17 | McLain, 1980 (34) | * | |||
| 18 | Alfredsdottir and Bjornsdottir, 2007 (35) | * | |||
| 19 | Tabibzadeh and Jahangiri, 2018 (14) | * | |||
| 20 | Guedon et al., 2014 (36) | * | |||
| 21 | Frosini et al., 2016 (37) | * | |||
| No. | Author Name and Year of Publication | Risk Management Program Results | |||
|---|---|---|---|---|---|
| Identifying the Main Causes of Errors | Achieving Effective Methods in Reporting Errors | Achieving Effective Methods to Reduce Errors | The Need for Informed Consent | ||
| 1 | Sayed et al., 2013 (20) | * | * | * | |
| 2 | Guo, 2015 (17) | * | |||
| 3 | van Beuzekom et al., 2012 (21) | * | * | ||
| 4 | Schimpff, 2007 (22) | * | |||
| 5 | Borie et al., 2018 (23) | * | |||
| 6 | Frabetti et al., 2005 (24) | * | |||
| 7 | Amghar et al., 2017 (25) | * | |||
| 8 | Silen-Lipponen et al., 2005 (26) | * | |||
| 9 | Pomerantz et al., 2011 (27) | * | |||
| 10 | DeRosier et al., 2019 (18) | * | |||
| 11 | Kavosi et al., 2017 (28) | * | |||
| 12 | Le Bourg and Gallois, 2011 (29) | * | |||
| 13 | Lepanluoma et al., 2013 (30) | * | * | ||
| 14 | American College of Obstetricians and Gynecologists, 2010 (31) | * | |||
| 15 | American Society of Anesthesiologists Task Force on Operating Room Fires et al., 2008 (32) | * | |||
| 16 | Bower, 2002 (33) | * | |||
| 17 | McLain, 1980 (34) | * | * | ||
| 18 | Alfredsdottir and Bjornsdottir, 2008 (35) | * | |||
| 19 | Tabibzadeh and Jahangiri, 2018 (14) | * | |||
| 20 | Guedon et al., 2014 (36) | * | |||
| 21 | Frosini et al., 2016 (37) | * | |||
Prerequisites for the risk management program include five sub-themes: Human resources, financial resources, culture and structure, knowledge and information, and equipment and technology. Among these prerequisites, human resources (100%), knowledge and information (71%), culture and structure (24%), equipment and technology (19%), and financial resources (10%) were the most prevalent types of prerequisites in the risk management program across the articles (Table 5).
| No. | Author Name and Year of Publication | Prerequisites for Risk Management Program | ||||
|---|---|---|---|---|---|---|
| Human Resources | Financial Resources | Culture and Structure | Knowledge and Information | Equipment and Technology | ||
| 1 | Sayed et al., 2013 (20) | * | * | |||
| 2 | Guo, 2015 (17) | * | * | |||
| 3 | van Beuzekom et al., 2012 (21) | * | * | |||
| 4 | Schimpff, 2007 (22) | * | * | * | ||
| 5 | Borie et al., 2018 (23) | * | ||||
| 6 | Frabetti et al., 2005 (24) | * | * | |||
| 7 | Amghar et al., 2017 (25) | * | * | |||
| 8 | Silen-Lipponen et al., 2005 (26) | * | * | |||
| 9 | Pomerantz et al., 2011 (27) | * | * | |||
| 10 | DeRosier et al., 2019 (18) | * | * | |||
| 11 | Kavosi et al., 2017 (28) | * | * | |||
| 12 | Le Bourg and Gallois, 2011 (29) | * | * | * | ||
| 13 | Lepanluoma et al., 2013 (30) | * | * | |||
| 14 | American College of Obstetricians and Gynecologists, 2010 (31) | * | * | |||
| 15 | American Society of Anesthesiologists Task Force on Operating Room Fires et al., 2008 (32) | * | * | |||
| 16 | Bower, 2002 (33) | * | * | * | * | |
| 17 | McLain, 1980 (34) | * | * | * | ||
| 18 | Alfredsdottir and Bjornsdottir, 2008 (35) | * | * | * | ||
| 19 | Tabibzadeh and Jahangiri, 2018 (14) | * | * | |||
| 20 | Guedon et al., 2014 (36) | * | * | |||
| 21 | Frosini et al., 2016 (37) | * | * | |||
Facilitators of the risk management program include nine sub-themes: Use of modeling, use of expert opinions, teamwork, use of quality approach, use of equipment with good performance and adequate supervision, presence of a person as a risk manager, use of records, use of monitoring technologies to identify and report faults and identifying and monitoring safety indicators. Among the facilitators, the use of monitoring and detection technologies (57%), teamwork (38%), the use of equipment with good performance and adequate supervision (14%), the use of expert opinions (10%), the use of modeling, using a qualitative approach, and using records and identifying and monitoring safety indicators (5%) were most frequent in risk management program facilitators among the articles (Table 6).
| No. | Author Name and Year of Publication | Risk Management Program Facilitator | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Use of Modeling | Use of the Opinions of Experts | Teamwork | Use of a Qualitative Approach | Having an Individual as a Risk Manager | Use of Records and Documents | Monitoring, Detection, and Error Reporting Technologies | Identifying and Monitoring Safety Indicators | Equipment with Good Performance and Adequate Supervision | ||
| 1 | Sayed et al., 2013 (20) | * | * | |||||||
| 2 | Guo, 2015 (17) | * | ||||||||
| 3 | van Beuzekom et al., 2012 (21) | * | ||||||||
| 4 | Schimpff, 2007 (22) | * | ||||||||
| 5 | Borie et al., 2018 (23) | * | ||||||||
| 6 | Frabetti et al., 2005 (24) | * | ||||||||
| 7 | Amghar et al., 2017 (25) | * | ||||||||
| 8 | Silen-Lipponen et al., 2005 (26) | * | * | * | ||||||
| 9 | Pomerantz et al., 2011 (27) | * | ||||||||
| 10 | DeRosier et al., 2019 (18) | * | * | |||||||
| 11 | Kavosi et al., 2017 (28) | * | * | |||||||
| 12 | Le Bourg and Gallois, 2011 (29) | * | * | |||||||
| 13 | Lepanluoma et al., 2013 (30) | * | ||||||||
| 14 | American College of Obstetricians and Gynecologists, 2010 (31) | * | * | |||||||
| 15 | American Society of Anesthesiologists Task Force on Operating Room Fires et al., 2008 (32) | * | * | |||||||
| 16 | Bower, 2002 (33) | * | * | |||||||
| 17 | McLain, 1980 (34) | * | * | |||||||
| 18 | Alfredsdottir and Bjornsdottir, 2008 (35) | * | ||||||||
| 19 | Tabibzadeh and Jahangiri, 2018 (14) | * | ||||||||
| 20 | Guedon et al., 2014 (36) | * | ||||||||
| 21 | Frosini et al., 2016 (37) | * | ||||||||
5. Discussion
The present study attempted to identify the characteristics of risk management programs in the operating rooms of hospitals in different countries. A total of 21 studies that were the same in terms of purpose and data collection methods were included in the study. After analyzing the findings, the characteristics of risk management programs were classified into six main factors and 35 sub-factors.
The highest number of studies on risk management in the operating room was in the United States (42%). The oldest study was conducted in 1980, and the most recent one was performed in 2019. Eleven articles have mentioned all the errors that can happen in the operating room. Six of the articles are related to clinical errors, and two of the articles are related to fire in the operating room. Also, one of the articles is related to human errors, and one is related to equipment failure. Most articles have used the FMEA, root-cause analysis (RCA) model, and WHO safety guidelines as risk management models.
One of the important features of risk management programs in hospitals is the goals of these programs. Many hospitals plan and implement risk management programs to address the risks involved. The existence of an incident registration system is an active approach to risk management, which is opposed to a passive approach. In the proactive approach, their repetition can be prevented by recording incidents and learning from mistakes (38, 39). The next main goal is to improve safety in the operating room. There is a strong link between risk management and safety promotion (40). In an organization with a positive safety culture, all employees at different levels value safety and consider it the organization’s main priority (41). In such an organization, the likelihood of dangerous events and even healthcare costs are significantly reduced (42). Attention to prospective risk management approaches will be very effective in increasing safety in the hospital (43). Quality improvement has also been one of the goals of the risk management program in the operating room (40). Due to the increasing competition in the field of medicine, one of the approaches of hospital managers to increase the quality of care is to apply the risk management process comprehensively and efficiently (44). So, in all quality improvement programs, the risk management approach is one of the main axes of creating, deploying, and using management systems in organizations (45). Risk prevention and reduction are also among the main goals of risk management programs in the operating room. In general, risk management means preventing the occurrence of the hazard, reducing risks and injuries, and managing risks after an event (44, 46). Therefore, by implementing this program, hospitals tend to prevent risks and reduce their error rate. The next goal is to protect against financial losses and reduce operating room costs. Hospitals can take steps to reduce clinical error-related loss by using a risk management approach (44). The ultimate goal of implementing a risk management program is to improve satisfaction. According to studies in this field, risk management, in turn, will lead to improved satisfaction (46).
The next feature of operating room risk management programs is the program’s components. What are the components of risk management programs designed and implemented for hospital operating rooms? The first and most important component of communication risk management programs is communication. Effective risk management programs require open lines of communication (47). According to studies, increased cooperation between operating room staff and staff communication has reduced patient risks and mortality (30). To carry out the risk management program in the operating room correctly, it is necessary to form a team and communicate effectively between the teams to identify and manage the risks through these communications. The next important component of the risk management program is monitoring. Until the monitoring is done, it will not be determined how well the program will work. Risk and emergencies can be reduced by applying and monitoring clear preventive policies with specific frameworks and roles in the operating room (30). Therefore, establishing hospital monitoring programs to implement a risk management program is necessary (48). Resources are also a component of risk management programs. Managing human, financial, material, support, and system resources is critical for each resource before, during, and after an unforeseen event. Undesirable hidden risk is designed to help improve patient safety in the operating room (49). The next pillar of the risk management program is leadership. Leaders in every hospital must be aware of the critical need for patient safety programs and strive to reduce risks, and make safety champions of change (50). Encouraging commitment in employees to implement the program, the teamwork of members, execution of orders, information transfer, case reporting, etc., align with the concept of leadership (51).
Organizational culture is also a component of the risk management program. As explained above, successful organizations implementing risk management programs have a positive safety culture, and all employees at different levels value safety and consider it the organization’s main priority (41). Studies in this field consider a culture of prevention and protection against hazards by nursing staff in the operating room to be crucial in increasing safety (52). The last component of the risk management program is training. Training is one of the human resources approaches requiring extensive internal training for properly implementing the error reporting system and error management steps in the operating room (47).
The next important feature is the implementation of the risk management program in the hospital. In general, four models for risk management in the operating room were identified, the most common of which are related to the steps: (1) preoperative evaluation during (logging); (2) evaluation during surgery; (3) post-surgery evaluation (logout). In this model, which can also be called pre-test/post-test evaluation (49), using different methods, the hospital first identifies the risks before surgery and then performs its proposed interventions during surgery to identify errors. Finally, after surgery, the effectiveness of the measures is re-evaluated. Other models of risk management (creating an environment, identifying, analyzing, evaluating, risk elimination, consulting, monitoring, creating and informing prevention programs, creating a channel for error reporting, training, and obtaining feedback) among the steps used in the operating room risk management have been reported to reduce the risks after implementing a risk management program in the operating room.
The next feature of risk management programs is the results of the program. What are the results of the implemented risk management programs for the hospital or the operating room? According to the findings, the highest results obtained from implementing risk management programs were the achievement of effective methods in reducing errors. For example, the use of a safe surgical checklist (46), the use of well-functioning equipment under adequate supervision (31), and systematic reporting to assist in decision-making in the areas of risk management (53) were among the effective methods in reducing errors. The next important result of implementing a risk management program in the operating room is achieving effective methods for reporting errors. A safety notification system, which is a system for monitoring the safety status (periodic repairs and recorded failures) of operating room devices and facilitating information about failures (36), a web-based monitoring dashboard (37), and automatic collection of computer data using technology (54) were among the methods of reporting errors. Identifying the main causes of errors is also one of the main results of implementing a risk management program. In a study, 204 errors were reported for 36 sub-processes, with the highest frequency related to human and organizational errors and the lowest to technical errors (28). In another study, nurses identified the most common causes of the error, including lack of knowledge, information, and supervision, heavy workload, and poor judgment, which may lead to active and hidden errors (52). Another study identified the necessity of obtaining informed consent. The importance of completing and clarifying surgical satisfaction for the patient or one of the patient’s relatives, which is done by increasing the level of communication between surgeons and patients and discussing the conditions and possible results of surgeries, will lead the hospital to be safe against possible financial and legal consequences and risks (55).
The next feature of risk management programs is the prerequisites of the risk management program. Prerequisites are a set of factors that are required to run the program. Human resources are the most important prerequisite for implementing a hospital risk management program. In the absence of human resources, no management program will be feasible because the implementers of this program are human resources. In most articles, discussing human resources and teamwork in the operating room is recognized as a necessity of risk management programs (29, 30). The next prerequisite is the discussion of knowledge and information. Some sources believe that risk management in an organization cannot be successfully implemented without knowledge and information (56). Leaders and officials need the necessary knowledge to deal with the crisis at the right time and place. The next prerequisite is culture and structure. In most articles, culture and structure are the basic principles for implementing a risk management program (51, 57). Unless there is a clear structure for staff in a hospital and the staff does not follow a certain culture, one cannot expect to implement a risk management program in the operating room. The next issue is equipment and technology. In risk management, using technologies and equipment, especially in the communication and information for organizations involved in operations, is very important. Collecting data from the risk area using these technologies will be much faster and more reliable and help better implement the risk management program, for example, the automatic collection of computer data using technology to monitor infections in the operating room (54), the use of a safety status system to monitor the safety of operating room equipment (36), and use of a monitoring dashboard to collect information from devices in the room action (37). Financial resources are the last prerequisite for implementing risk management programs in the operating room. The implementation of any program requires financial resources to be operational. In implementing a risk management program in the operating room, the provision of financial resources such as human resources and knowledge is of particular importance (49).
Risk management program facilitators are the final feature of operating room risk management programs. Facilitators are tools that facilitate the implementation of these programs. Among the facilitators, the use of monitoring technologies and error detection and reporting are recognized as the most important types of facilitators of risk management program implementation. These technologies could be prerequisites for any program, making receiving errors easier and taking timely action. The next facilitator is teamwork. Operating room teamwork means combining complementary skills, overlapping team members, and mutual understanding while caring for patients undergoing surgery (58). Evidence has shown that teamwork in healthcare systems improves patient safety (59). For this reason, most studies have used the workforce required in the risk management program as a team. The next case is using equipment with good performance and adequate supervision, which facilitates control and reduces the occurrence of hazards in the operating room (31). Using experts’ opinions also facilitates risk management in the operating room; for example, advice based on a combination of scientific literature and analysis of expert opinions to facilitate patient care in the face of risks (31). Subsequent facilitators include modeling that provides a framework for presenting causal relationships and enables possible inference among a set of variables (25). It is necessary to act with reflection and commitment at all times with the aim of permanent improvement (29), the use of records and documents such as medical history or any particular medical condition (55), and identifying and monitoring safety indicators that are used to assess and monitor internal and external social and technical factors in a health care setting (16).
5.1. Conclusions
Based on the results of the current study, we identified six main factors as features of the risk management program in the operating room. The operators of the risk management program in the operating room should pay special attention to these factors during planning in order to get the most effectiveness from the implementation of the program. The conceptual framework of any risk management program should include at least the objectives: Risk eradication, safety promotion, quality improvement and prevention and reduction of risks, component: communication and monitoring; steps: (1) preoperative evaluation during (logging); (2) evaluation during surgery; (3) post-surgery evaluation (logout); and the results: Achieving effective methods in reducing errors, prerequisites: Human resource, knowledge and information, and facilitators such as the use of monitoring technologies and error detection and reporting in the operating room. Using this framework, any risk management program operator can adapt their conditions to the program objectives, the components that the program must have, the steps it must go through, the prerequisites and facilitators, and the results it wants to achieve, and, as a result, take the appropriate route to reduce hazards in the operating room.
These results help health insurance organizations and health policymakers get information about the risk management frameworks and the status of the operating rooms of the hospitals to carry out managerial and policy interventions for the effective implementation of the developed framework. The results will also help the health system achieve its set goals to improve people’s health, meet their reasonable expectations, and receive safe and line-free service for patients and a safe work environment for personnel.
5.2. Limitations
The main limitation of this research was conducting very limited studies in the field of risk management, especially in the operating room of hospitals worldwide. However, we tried to deal with this limitation using organizational reports, published government documents, websites, and other gray information sources for obtaining information.