1. Background
Pregnancy involves numerous physiological changes that may pose serious risks to maternal and fetal health (1). The most common and health-threatening problems related to pregnancy are improper weight gain, iron deficiency anemia, gestational diabetes mellitus (GDM), preeclampsia, eclampsia, and gestational hypertension (2, 3). Maternal weight gain during pregnancy is an important indicator of maternal and fetal health (4).
The risks of inadequate weight gain include preterm birth, low birth weight, small-for-gestational-age infants, perinatal mortality, and failure to initiate breastfeeding. The risks of excessive weight gain include Cesarean delivery, GDM, pre-eclampsia, postpartum weight maintenance for the mother, large-for-gestational-age infants, macrosomia (birth weight >4000 g), and childhood overweight or obesity for the infant (5, 6).
Anemia is a common pregnancy disorder (7), with a prevalence estimated at 17% in Iran. The highest (23%) and lowest (12%) prevalence rates were observed in the center and west of the country, respectively (8). In addition, the prevalence of anemia in pregnant women in Zahedan, Iran (2016) was reported to be 46.6% (9).
Maternal anemia is accompanied by side effects for the newborn, such as the increased risk of preterm birth or birth weight (10, 11), and complications for the mother, such as death (12). Iron deficiency is the most common nutritional deficiency and the most prevalent cause of gestational anemia. It is defined as a hemoglobin concentration in the peripheral blood lower than 11 g/100 mL (13).
Gestational diabetes mellitus is defined as any degree of dysglycemia with onset or first recognition during pregnancy. GDM can adversely impact perinatal outcomes, cause potential adverse maternal and neonatal sequelae, increase the risk of obesity in the infant, and the subsequent development of diabetes in the mother (14, 15). The prevalence of GDM in Iran was reported to be 7.9%. The lowest prevalence was observed in Ardabil Province (1.3%) and the highest in Tehran (23.9%) and Mazandaran (23.1%) provinces (16). The prevalence of GDM in Zahedan (2022) was reported to be 37.7% (17).
Preeclampsia is a multifactorial pregnancy disorder observed in 1.5 - 5% of pregnancies in the form of edema, hypertension, and proteinuria. It is accompanied by high risks of preterm delivery, intrauterine growth, premature placental abruption, and maternal illness and death (18-20). In several studies conducted in Iran, the prevalence of preeclampsia has been reported as 1 - 8% (21); in Zahedan, the prevalence of preeclampsia was reported to be 7.8% (22).
Normal maternal thyroid function during pregnancy is essential to prevent negative consequences for the mother and fetus (23). In a systematic review and meta-analysis on thyroid disorders in Iranian pregnant women, the prevalence of thyroid dysfunction was estimated at 18.1%. Moreover, the prevalence of hypothyroidism and hyperthyroidism was respectively 13.01% and 3.31% (24).
Pregnancy hypothyroidism has adverse effects, including gestational hypertension, preeclampsia, anemia, low fetal birth weight, miscarriage, congenital circulation system malformations, respiratory distress, and fetal death (25, 26). Unconjugated hyperbilirubinemia (jaundice) is common in the first days after birth in 50% of full-term infants and 80% of premature infants (27). Heme catabolism produces bilirubin, and at low amounts, it works as an antioxidant. Higher concentrations can be toxic to the infant's nerve cells (28).
Some studies have evaluated the prevalence of pregnancy-related complications and their relationship with neonatal complications in Tabriz (29) and Mashhad, Iran (30). However, socioeconomic levels and cultural and conventional beliefs can influence this relationship.
2. Objectives
The identification of problems and factors threatening the health of mothers and paying more attention to health and nutritional care during pregnancy help prevent and control neonatal complications related to pregnancy and the future health of mothers and infants. Therefore, this study aimed to investigate the prevalence of pregnancy-related problems and their relationship with neonatal complications in pregnant women referring to the health care centers of Zahedan.
3. Methods
This cross-sectional study was conducted in 2019 on 630 women selected using systematic random sampling from women referring to the health care centers of Zahedan.
This study aimed to investigate several problems in pregnant women and their relationship with neonatal complications. Besides, the most frequent problem in previous studies was anemia in pregnant women, with a prevalence of 17% (31). To cover other problems, P=0.2 was considered, and the sample size was determined as follows:
The above formula suggested a sample size of 558 based on the acceptable ratio and error of the results of the sample against the population. However, we finalized the sample size at 630 to increase the value of the study.
For participant selection, the city of Zahedan was divided into five geographical regions: North, south, east, west, and center. Then, two healthcare centers were randomly selected in each region (10 centers in total). In each center, the data of 63 participants were randomly collected.
Demographic and anthropometric data were collected and recorded in a gestational and neonatal care form. Age, weight, height, body mass index, and gestational complications were recorded for mothers. In addition, the height, weight, head circumference, and neonatal complications such as hypothyroidism, underweight, jaundice, macrosomia, and microcephaly were recorded for infants.
Inclusion Criteria: Mothers who had recently delivered and visited health care centers for newborn screening tests were recruited if they met the following criteria: Iranian nationality, no history of diseases before pregnancy, no smoking, no narcotic and alcohol use, and no consumption of nutritional supplements before pregnancy.
Exclusion Criteria: If there was no full access to the required information, the mother and newborn were excluded from the study and replaced by other participants.
The data were analyzed in SPSS v. 22 (IBM, Chicago, IL, USA) using descriptive statistics and the chi-square test. The significance level was P < 0.05.
This study was approved by the Ethics Committee of Zahedan University of Medical Sciences (IR.ZAUMS.REC.1397.166; project code: 8837).
4. Results
A total of 630 women were enrolled. The mothers' mean age was 28.35 ± 6.3 years. Among the newborns, 51.9% and 48.1% were male and female, respectively. Table 1 shows the findings of descriptive data analysis.
| Variables | Mean ± SD | Range |
|---|---|---|
| Mothers | ||
| Mother's age, y | 28.35 ± 6.3 | 15 - 45 |
| Number of pregnancies | 2.8 ± 1.8 | 1 - 9 |
| Number of children | 2.6 ± 1.6 | 0 - 9 |
| Height, cm | 158 ± 6 | 138 - 180 |
| Weight, kg | 65.1 ± 14.4 | 35.5 - 115 |
| Infants | ||
| Birth weight, gr | 3100.75 ± 495.25 | 1280 - 5000 |
| Birth height, cm | 49.35 ± 2.21 | 40 - 57 |
| Head circumference at birth, cm | 34.17 ± 1.24 | 28 - 37.5 |
| Total | 630 |
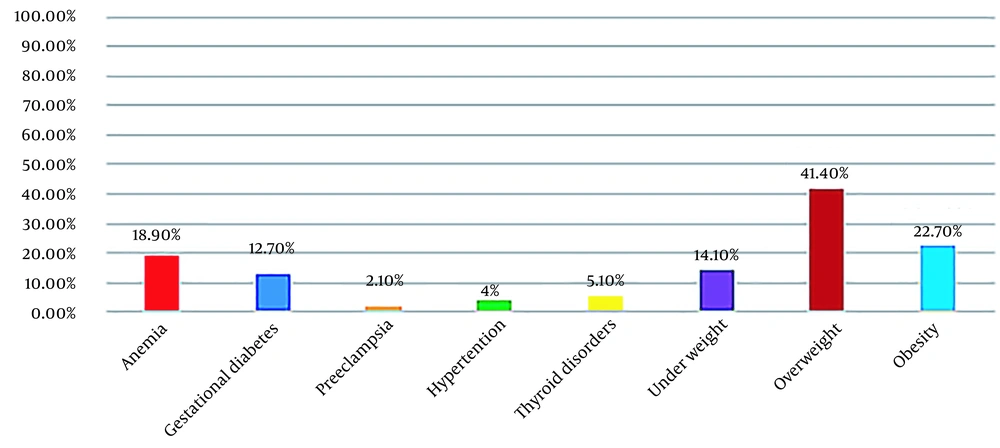
Figure 1 depicts the frequency distribution of pregnancy-related complications in pregnant women referring to healthcare centers.
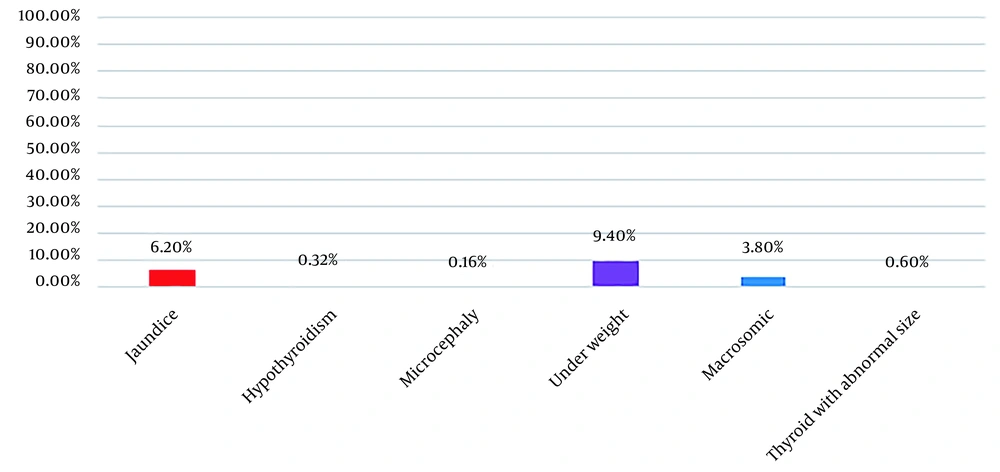
Figure 2 also shows the frequency distribution of complications in the neonates of mothers referring to healthcare centers in Zahedan.
The results showed that 7.3% of the boys were low birth weight, and 4% were macrosomic, while 11.6% of the girls were low birth weight and 3.6% were macrosomic.
Table 2 presents the relationship between the birth weight index and the maternal body mass index.
a Values are expressed as No. (%). Significance level: P < 0.05
b Body mass index.
c Chi-square test.
There was a significant relationship between the infant's birth weight and maternal body mass index (P < 0.05); underweight mothers had 12.4% and 1.1% underweight and macrosomic infants, respectively. However, obese women had 4.9% and 7.7% underweight and macrosomic infants, respectively.
There was a significant relationship between maternal iron deficiency anemia and the infant's birth weight (P < 0.05), so mothers with iron deficiency anemia had 13.4% underweight infants. Maternal iron deficiency anemia had no significant relationship with head circumference, hypothyroidism, and neonatal jaundice (P > 0.05).
The relationship between birth weight and maternal GDM was also assessed, and the results are shown in Table 3.
a Values are expressed as No. (%). Significance level: P < 0.05
b Gestational diabetes mellitus.
c Chi-square test.
There was a significant relationship between maternal GDM and the infant's birth weight (P < 0.05), so mothers with GDM had 5% and 10% underweight and macrosomic infants, respectively.
There was also a significant relationship between maternal GDM and neonatal jaundice (P < 0.05), so mothers with GDM had 11.3% of infants with jaundice.
Our findings did not show any significant relationship between the infants' head circumference indices and hypothyroidism on the one hand and maternal GDM on the other hand (P > 0.05).
However, in mothers with preeclampsia, 7.7% of the infants were underweight, and a significant relationship was observed between maternal preeclampsia and neonatal jaundice indices (P < 0.05). Among the mothers with preeclampsia, 23.1% had newborns with jaundice. Also, there was not a significant relationship between birth weight and head circumference on the one hand and maternal preeclampsia on the other hand (P > 0.05).
The findings showed a significant relationship between birth weight indices and maternal hypertension (P < 0.05); mothers with hypertension had 32% and 8% underweight and macrosomic infants, respectively. We did not observe any significant relationship between neonatal head circumference at birth and neonatal jaundice on the one hand and maternal hypertension on the other hand (P > 0.05). Furthermore, 16.7% of the underweight infants and 17.60% of the infants with jaundice were born to mothers with hyperthyroidism. In mothers with hypothyroidism, 5% of the infants were underweight, and 20% had jaundice. The results did not show any significant relationship between birth weight, neonatal head circumference, neonatal hypothyroidism, jaundice, and maternal thyroid disorders (P > 0.05). Moreover, there was no association between birth weight, neonatal circumference, neonatal hypothyroidism, and jaundice based on the infants' sex (P > 0.05).
5. Discussion
This study examined pregnancy-related complications and their relationship with neonatal complications among mothers referring to healthcare centers in Zahedan. The findings revealed a significant relationship between the infant's birth weight and the mother's body mass index, hypertension, GDM, and iron deficiency anemia. There was also a significant association between infant jaundice and the mother's GDM and preeclampsia.
The results showed that 14.1%, 41.1%, and 22.7% of the mothers were underweight, overweight, and obese, respectively. The mothers' anthropometric characteristics, such as weight, show adequate energy intake and body size, which affect the size of the placenta and the infants' weight (32). In accordance with the present study, Zhang et al.'s study in China showed that women who did not properly weight gain during their pregnancy had a higher risk of preterm delivery, low birth weight, and small fetuses based on their pregnancy age (33). Sharma et al. conducted a study in Nepal on low-birth-weight infants and reported that factors such as hard physical activity during pregnancy, the mother's young age, iron deficiency anemia, and nutrient deficiency during pregnancy had significant relationships with low birth weight (34). Ahmadzadeh Sani et al. carried out a study on 180 Iranian pregnant women and found a significant relationship between maternal obesity and the infant's low birth weight and also pregnancy complications such as preeclampsia, hypertension, and gestational diabetes (35). Thus, appropriate maternal weight gain during pregnancy can be an important factor in avoiding low-birth-weight infants. The results obtained by Nourbakhsh et al. on 163 nondiabetic pregnant women indicated a direct relationship between maternal body mass index during pregnancy and the infant's birth weight. They also showed that maternal overweight and obesity increase the probability of overweight infants (36).
The present study did not find a significant relationship between sex, weight, and head circumference at birth. This finding was in agreement with the results reported by Akbarzadeh and Zare on 180 Iranian pregnant women (37) and in contrast with the results reported by Judipour et al. on 1712 Iranian women (38). This difference in findings may be explained by socioeconomic differences.
The present study indicated that 18.9% of the mothers had anemia. Navidian et al. reported the prevalence of anemia during pregnancy to be 12.9% in Zahedan (39). Moreover, in the study by Gorgani et al., the prevalence of anemia in pregnant women referring to healthcare centers affiliated with Zahedan was 46.6% (9).
The present study revealed a significant relationship between maternal iron deficiency anemia and the infant's birth weight. In agreement with our results, Saberi et al. conducted a study on 504 Iranian pregnant women and showed a significant relationship between the infant's birth weight and maternal anemia. Anemia in the second and third trimesters of pregnancy was responsible for weight loss in infants (40). Organogenesis mostly occurs in the first trimester, and fetal weight increases in the second and third trimesters, which explains the effect of maternal anemia on infant weight in the second and third trimesters.
In the current study, 12.7% of the mothers had GDM. Noori et al. reported the prevalence of GDM in pregnant women referring to the health care centers affiliated with Zahedan to be 37.7% (17).
We observed a significant relationship between macrosomic neonates and maternal GDM, such that mothers with GDM had 10% macrosomic neonates. The results concur with the findings reported by Koyanagi et al. on 373 pregnant women in 23 developing countries (41). Since GDM is associated with an increased risk of adverse consequences such as macrosomia, thus glucose monitoring, maternal weight management, and having a proper diet, physical activity, and medication can reduce the complications related to GDM.
The present study showed a significant association between birth weight and maternal hypertension. Extensive epidemiological and biological evidence supports this observation. Gestational hypertension reduces uteroplacental flow and amniotic fluid, which increases the risk of low birth weight (42-44).
This study demonstrated a significant relationship between the prevalence of neonatal jaundice and GDM, which is in agreement with the findings reported by Boskabadi et al. (45). The reasons for neonatal jaundice who have diabetic mothers include the increased concentrations of free fatty acids after hypoglycemia, polycythemia, and weak maternal glucose control (46).
Our study also revealed a significant relationship between maternal preeclampsia and neonatal jaundice, which is similar to the results reported by Boskabadi et al. (47).
Although preeclampsia can increase the risk of intrauterine growth restriction and low birth weight due to decreased uterine placental blood flow (48), our study did not observe any significant association between low birth weight and maternal preeclampsia. This result is in contrast with that reported by Wahyuni and Puspitasari on 298 low-birth-weight infants in Indonesia (49).
The present study demonstrated a significant relationship between neonatal jaundice index and maternal thyroid disorders, such that neonates with jaundice had mothers with hyperthyroidism and/or hypothyroidism. Mojtahedi et al. showed that thyroid-stimulating hormone (TSH) and thyroxine (T4) have a close relationship with jaundice, i.e., a higher level of TSH leads to a higher risk of jaundice in infants (50).
The present study did not find any significant relationship between maternal hemoglobin level and neonatal bilirubin. Nevertheless, Tavakolizadeh et al., in their study of newborns in Iran, reported a significant relationship between these factors (51).
Since the promotion of the health of newborns as a vulnerable group is of special importance, the health assessment of pregnant women in all levels of health care services should be a fundamental policy.
5.1. Conclusions
Considering the prevalence of pregnancy-related complications such as anemia, GDM, underweight, overweight, obesity, thyroid disorders, and hypertension in the studied mothers, and the effect of these complications on the fetus, it is essential to identify the problems threatening the health of the mother and fetus. The early identification of pregnancy-related complications and the administration of health and nutritional interventions before and during pregnancy can greatly prevent neonatal complications caused by pregnancy.
Future studies should simultaneously investigate the relationship between various factors related to pregnancy complications and their effect on maternal and neonatal complications.
5.2. Study Limitations and Strengths
The potential limitations of this present study include a lack of accurate and complete information recording (an uncontrollable limitation), data collection from different healthcare centers, and the possibility of measurement errors.
The study's strengths are that it examined numerous pregnancy-related complications and their relationships with neonatal complications concurrently; as such, the findings can be used in research and in prenatal care planning by health care centers.