1. Background
According to the World Health Organization, approximately 732.9 million COVID-19 cases and 6.7 million COVID-19-related deaths were reported worldwide from the start of the pandemic until the end of 2022, with the largest global peak in COVID-19 transmission in December 2022. More than three years into the pandemic, countries worldwide continue to face many challenges in responding to the evolving and recurring challenges of COVID-19 while maintaining other Essential Health Services (EHS) (1). As of 2021, there are more than 257 million confirmed cases of COVID-19 worldwide and more than 6 million in Iran (2).
COVID-19 is characterized by death anxiety, which is among the psychological problems caused by this viral infection (3). Death anxiety is defined as an irrational, intense fear of death, recognized as the terror of death or having apprehensive thoughts about death or the events that ensue (4). Several factors contribute to the development, persistence, and responses to death anxiety, the most important of which include innate personality tendencies such as Early Maladaptive Schemas (EMSs) (5). Cognitive schemas are mental structures formed in the individual's psyche and personality from birth. The individual's relationships and responses to different events and phenomena are rooted in these structures (6). People's responses to health anxiety and death anxiety seem to mostly arise from their EMSs (5, 7). Further, the researchers observed that individuals with high levels of COVID-19 fear and anxiety were at a higher risk of psychiatric disorders (8).
Faustino et al.'s (9) study showed that early maladaptive schemas are related to COVID-19 anxiety and mental health. Another study by Silva et al. (10) aimed to assess the correlation between COVID-19 anxiety, death-related concerns, and their effects on psychological well-being. The results indicated that individual differences in the fear of death were associated with their psychological well-being and its correlation with disease anxiety due to COVID-19. On the other hand, bringing the idea of death to prominence through manipulated news did not affect this correlation (10).
Compared to other students, clinical medical students, as a whole, are in closer contact with COVID-19 patients in health centers (11). Therefore, they are more susceptible to disease anxiety and death anxiety, which can largely influence their educational performance and mental health.
The present study aimed to determine COVID-19 anxiety among university students and its correlation with death anxiety and EMSs. The researchers intended to provide a comprehensive overview of disease anxiety, death anxiety, and the frequency of EMSs in students and precisely analyze the correlations between these parameters. Our findings can be used to elucidate effective solutions to manage COVID-19 anxiety in social groups (especially among university students), prevent a decline in students' academic performance, and improve their quality of life.
Previous studies in this field, especially during the COVID-19 pandemic, have documented that anxiety related to COVID-19 may be associated with EMSs and death anxiety; however, these findings cannot be generalized as only a limited number of studies have explored different manifestations of COVID-19 anxiety. Accordingly, further investigations are required to clarify how EMSs are associated with death anxiety in nursing or medical students, which schemas correlate strongly with COVID-19 anxiety, and how some demographic variables affect the severity of COVID-19 anxiety. More studies are also needed to confirm the previous evidence and reach an agreement in this regard.
2. Objectives
The current research aimed to determine the relationship between EMSs, COVID-19 anxiety, and death anxiety during the COVID-19 pandemic among Zahedan University of Medical Sciences (ZAUMS) students in Iran.
3. Methods
3.1. Study Subjects
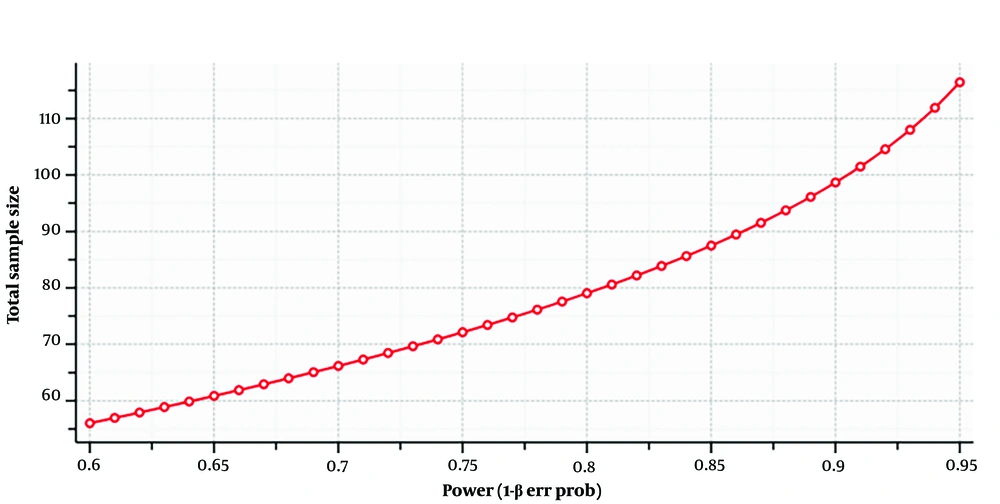
The present descriptive-analytical cross-sectional study recruited a sample of ZAUMS students in 2022. Based on G*power, the software, we selected 120 ZAUMS students as the research sample using purposive and convenience sampling (Effect size f2 = 0.20, α err proB = 0.05, Power (1-β err prob) = 0.95, Total sample size = 117, Actual power = 0.9511212) (Figure 1).
The participants responded to a questionnaire to collect data, and convenience sampling was also used to select the sample population. The inclusion criteria were 18 - 45 years old, studying nursing or medicine at the ZAUMS, and informed consent to participate in the study. The exclusion criteria were suffering from a mental disability, having symptoms of psychosis, and suffering from a disease inhibiting cooperation in the study.
3.2. Data Collection Tools
Data collection was performed using standardized questionnaires for the Iranian population. The participants first completed a demographic questionnaire regarding age, gender, history of COVID-19 contraction, contact with a COVID-19 patient, discipline, place of residence, and participation in educational courses.
3.2.1. COVID-19 Anxiety Scale
This 18-item scale was used to assess the level of COVID-19 anxiety. The COVID-19 Anxiety Scale was developed and validated to measure COVID-19-related anxiety in Iran. The items of this scale are scored based on a four-point Likert scale (Never=0, Sometimes=1, Very Often=2, and Always=3). Construct validity showed a moderately negative correlation (Pearson's r = −0.417) with self-rated mental health (12). In this study, the reliability of this test is reported as 0.87 using Cronbach's alpha method.
3.2.2. Templer Death Anxiety Scale
This scale was developed by Templer in 1970 to measure the level of death anxiety. The Templer Templer Death Anxiety Scale (DAS) is a simplified tool widely applied in research studies. It is a self-report questionnaire consisting of 15 true/false questions. Tavakoli and Ahmadzadeh showed that this scale has appropriate validity (13). In this study, the reliability of this test is reported as 0.76 using Cronbach's alpha method.
3.2.3. Young Schema Questionnaire (YSQ)
This scale assesses 15 EMSs. Each schema is measured by answering related questions among 75 questions. The scale items are scored based on a six-point Likert scale ranging between Completely False (=1) and Completely True (=6). Fata and Fata et al. showed that this scale has appropriate validity (14). In this study, the reliability of this test is reported as 0.82 using Cronbach's alpha method.
3.3. Ethical Considerations
The research objectives were clearly explained to the participants. They signed informed consent forms.
The study was registered with the Research Ethics Committee of ZAUMS in Iran with the code IR.ZAUMS.REC.1401.086).
3.4. Study Procedure
After obtaining the required permit from the Vice-Chancellor of Research and the ethics code from the Ethics Committee of ZAUMS, the participants were selected from the students of ZAUMS by convenience sampling. Convenience sampling was done in such a way that there were medical and nursing students studying at ZAUMS, and after reading the invitation letter from the medical school to participate in the research, they called the number on the poster.
They were medical and nursing students studying at ZAUMS who contacted the number on the poster after reading an invitation to the medical school to participate in the research. Then, the participants completed questionnaires distributed by a clinical psychologist with a master's degree from the same university. This was done individually with the researcher in a quiet room. The researcher explained the objectives and procedures of the research to the participants. After obtaining informed consent from the participants, the questionnaires were distributed to them. Notably, the participants were assured that their information would be kept confidential. There was no time constraint for completing the questionnaires.
3.5. Data Analysis
Data analysis was performed in SPSS version 22 using descriptive statistics (mean, standard deviation, frequency, and percentage) and inferential statistics (Pearson's correlation coefficient and multiple regression analysis).
4. Results
The mean age of the participants was 23.71. The research sample included 120 ZAUMS students (39.3% men). We found that 69.3% of the participants were infected with the virus. Also, 34.3% had a history of COVID-19. The field of study for 54.3% of the participants was medicine, while 45.7% were nursing students. The participants' courses were as follows: 64.3% were stagers, 23.6% were interns, and 12.1% were in other courses.
The descriptive results were as follows: COVID-19 anxiety (M = 90.27, SD = 92.6), death anxiety (M = 65.69, SD = 20.75), disconnection and rejection schema domain (M = 47.20, SD = 17.68), impaired autonomy and performance (M = 31.93, SD = 11.30), impaired limits (M = 26.24, SD = 9.45), other-directedness (M = 24.37, SD = 8.05), and over vigilance and inhibition (M = 28.27, SD = 11.49). The results indicated that the skewness value was within the range of ±1.96, and the data were adequately normal.
Evaluation of the beta coefficients showed that the standard coefficients were significant for the EMSs without the moderating role (B = 0.09, t = 1.99, P < 0.05, R2 = 0.09) or with the moderating role of a history of contact with a COVID-19 patient (B = 0.10, t = 2.69, P < 0.05, R2 = 0.09) only in the case of the social disconnection and rejection schema. Therefore, this component can be a reliable predictor of coronavirus anxiety (Table 1).
| Predictor | B | Std. E | β | T | P-Value | 95% Interval Confidence for B | |
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| Disconnectionand Rejection | |||||||
| Without a moderator | 0.09 | 0.05 | 0.252 | 1.991 | 0.04 | ||
| (Constant) | 21.09 | 27.615 | |||||
| Disconnectionand rejection | 0.01 | 0.14 | |||||
| History of contact with a COVID-19 patient as a moderator | 0.10 | 0.03 | 0.48 | 2.699 | 0.008 | ||
| (Constant) | 22.717 | 27.553 | |||||
| Disconnectionand rejection | 0.01 | 0.08 | |||||
Results of Multiple Regression Analysis Regarding the Correlation Between EMSs and COVID-19 Anxiety
The beta coefficients were also significant for the components of impaired autonomy and performance (B = 0.31, t = 2.17, r < 0.05), indicating that this schema can reliably predict death anxiety with the moderating role of the study period in university students (R2 = 0.06). The significant beta coefficient for impaired autonomy and performance showed that with the moderating role of a history of contracting COVID-19 (B = 0.24 t = 2.12, r < 0.05), this schema can also reliably predict death anxiety (R2 = 0.10). The significant beta coefficient for impaired autonomy and performance showed that with the moderating role of a history of contracting COVID-19 patients (B = 0.31; t = 2.14, P < 0.05), this schema can also reliably predict death anxiety (R2 = 0.09) (Table 2).
| Predictor | b | Std. E | β | t | P-Value | 95/0% Interval Confidence for B | |
|---|---|---|---|---|---|---|---|
| Lower Bound | Lower Bound | ||||||
| Impaired Autonomy and Performance | |||||||
| Without a moderator | 0.56 | 0.20 | 0.30 | 2.681 | 0.008 | ||
| (Constant) | 21.738 | 28.654 | |||||
| Impaired autonomy and performance | -0.01 | 0.187 | |||||
| History of contact with a COVID-19 patient as a moderator | 0.31 | 0.14 | 0.34 | 2.142 | 0.034 | ||
| (Constant) | 23.603 | 28.517 | |||||
| Impaired autonomy and performance | -0.008 | 0.096 | |||||
| History of contracting COVID-19 as a moderator | 0.24 | 0.11 | 0.32 | 2.124 | 0.03 | ||
| (Constant) | 24.12 | 29.26 | |||||
| Impaired autonomy and performance | -0.02 | 0.06 | |||||
| Discipline as a moderator | 0.31 | 0.14 | 0.32 | 2.202 | 0.029 | ||
| (Constant) | 22.33 | 27.71 | |||||
| Impaired autonomy and performance | 0.01 | 0.11 | |||||
| Study period as a moderator | 0.31 | 0.14 | 0.42 | 2.179 | 0.03 | ||
| (Constant) | 25.20 | 29.75 | |||||
| Impaired autonomy and performance | -0.03 | 0.05 | |||||
| Over-vigilance | |||||||
| Without a moderator | 0.42 | 0.21 | 0.23 | 0.014 | 0.04 | ||
| (Constant) | 23.96 | 29.96 | |||||
| Over-vigilance | -0.06 | 0.13 | |||||
| Discipline as a moderator | 0.41 | 0.13 | 0.42 | 2.936 | 0.004 | ||
| (Constant) | 23.62 | 28.45 | |||||
| Over-vigilance | -0.006 | 0.10 | |||||
Results of Multiple Regression Analysis Regarding the Correlation Between EMSs and Death Anxiety
5. Discussion
EMSs, specifically the disconnection and rejection schema, can predict COVID-19 anxiety only with the moderating role of contact history with a COVID-19 patient or without any moderators. On the other hand, EMSs, specifically the domains of over-vigilance and impaired autonomy and performance, can predict death anxiety. Additionally, the impaired autonomy and performance schema domain can predict death anxiety by considering the moderating role of the field of study, contact history with a COVID-19 patient, history of infection with COVID-19, and training course. Similarly, the domain of over-vigilance schema can predict death anxiety by considering the moderating role of the field of study. Our findings are consistent with previous studies from Portugal (9) and Poland (15). A previous study showed that home quarantine during the COVID-19 pandemic can activate the abandonment schema. It should be noted that this schema plays a role in creating anxiety (16). Therefore, it can be concluded that by controlling the moderating role of contact history with a COVID-19 patient, or in other words, in quarantine conditions where there is no contact with a COVID-19 patient, this schema can predict COVID-19 anxiety. One schema of disconnection and rejection schema domain is mistrust/abuse. A prior study showed that mistrustfulness relates to COVID-19 anxiety. This finding confirms our results about the predicting role of disconnection and rejection schema domain. Also, disconnection schemas can lead people to isolate themselves more, avoiding social interactions and support networks. This isolation can amplify feelings of loneliness and fear, making it harder to cope with the anxiety associated with the pandemic.
Neta et al. demonstrated that in situations characterized by ambiguity, such as the Threat of Shock (TOS), both cognitive and affective functions are impacted, leading to increased vigilance (17). On the other hand, research displayed that tolerance of ambiguity can predict death anxiety (18). We suppose that during the COVID-19 pandemic, individuals' over-vigilance schema domain is activated, so when they confront dangerous ambiguous situations, such as an infected environment, it evokes their death anxiety.
One of the over-vigilance schema domains is negativity/pessimism. The studies showed that pessimism is negatively associated with death anxiety (19). This finding aligns with our results about the predicting role of the over-vigilance schema domain.
Another study found a negative relationship between behavioral inhibition and the over-vigilance schema domain. On the other hand, behavioral inhibition is a mediator in the relationship between fear of COVID-19 and death anxiety (20). Therefore, we can conclude that the over-vigilance schema domain is related to death anxiety through behavioral inhibition.
5.1. Limitations
Purposive and convenience sampling could have affected the reliability of our research. Also, our sample size was small. Relying on the self-report questionnaire was another limitation of our study. This study has some strengths. It addresses a relevant and timely topic related to the COVID-19 pandemic, which was a major global concern during the study period. The use of multiple regression analysis allows for a deeper exploration of the relationships between variables, providing a more nuanced understanding of the factors influencing coronavirus anxiety and death anxiety.
5.2. Conclusions
Our results showed that the disconnection and rejection schema predicts COVID-19 anxiety (B = 0.25, t = 1.99, P < 0.05). Also, over-vigilance (B = 0.23, t = 2.01, P < 0.05) and impaired autonomy and performance schema domain (B = 0.30, t = 2.68, P < 0.001) predicted death anxiety. Disconnection and rejection schema domain could predict COVID-19 anxiety only with the moderating role of contact history with a COVID-19 patient. Our findings on death anxiety differ from the previous study because of the COVID-19 pandemic. These new results may help examine the effects of the COVID-19 pandemic on death anxiety and contribute to meta-theoretical conceptualization and clinical decision-making. From a clinical perspective, assessing EMSs may be especially relevant when psychological factors related to anxiety are identified. In order to apply these findings into clinical practice, further replications and expansion of the results are, however, needed. Future research in this area could consider Longitudinal Studies, Diverse Populations, Mental Health Interventions, and Resilience Factors.