1. Background
The coronavirus disease of 2019 (COVID-19) has caused a staggering impact on global health and economics since its emergence at the end of 2019, with the loss of 2.63 million lives worldwide (WHO, 2021). Vaccination is one of the most important public health measures in history, preventing infectious diseases (1, 2). Therefore, effective vaccination, along with effective public health measures, such as social distancing, wearing face masks, washing hands, avoiding closed, crowded spaces, and educating the general public, is crucial to reducing the epidemic of COVID-19 (3). COVID-19 vaccine development has advanced, with 105 vaccines currently in clinical testing and 18 approved for emergency use. Globally, 40 million doses of the COVID-19 vaccination have been distributed, with only a small proportion going to developing nations (4). The COVID-19 vaccines are being developed in four categories: nucleic acid vaccines, complete virus vaccines, viral vector vaccines, and protein-based vaccines (5).
The efficacy of the COVID-19 vaccine depends entirely on how many people receive it. There will be a reduction in the coverage of vaccinations if some individuals are reluctant to receive vaccines. Vaccine hesitancy is defined by the World Health Organization's (WHO) Strategic Advisory Group of Experts (SAGE) as “the refusal or delay in accepting vaccinations despite the availability of vaccine service" (6). Thus, even before the COVID-19 epidemic, the WHO identified vaccine reluctance as one of the top ten global health risks (7). The WHO and the United Nations Children's Fund studied 196 nations to investigate the causes of vaccination aversion (8). Approximately 74% of respondents expressed concerns regarding the risks and benefits of vaccinations, and these reservations were the most common reasons for vaccine hesitation. There are various reasons for vaccine reluctance, in addition to safety concerns. Vaccine acceptance may be influenced by educational background, previous experiences, or economic status (7). Fear and distrust of vaccinations among the worldwide population are considered major obstacles to achieving the goal of vaccination against COVID-19. The acceptance of vaccination is influenced by confidence, practicality, and complacency. Public acceptance of vaccinations must be promoted by healthcare professionals, legislators, community leaders, and governments (9, 10). The researchers designed and conducted this study to assess the public awareness about vaccines, the severity of COVID-19 disease, acceptance and hesitancy to receive COVID-19 vaccines, and trust in government measures regarding vaccines.
2. Methods
2.1. Study Design and Participants
An online survey was conducted from August 2021 to August 2022 using social media platforms such as Facebook, WhatsApp, and telephone. A hard copy of the questionnaire was also distributed to educational institutions and healthcare facilities. The study included major cities in Pakistan, including Lahore, Multan, Faisalabad, Islamabad, Sargodha, Abbottabad, Swat, Quetta, and Mardan.
2.2. Questionnaire
The sociodemographic profile of the participants was gathered through a questionnaire. The study subjects were also asked detailed questions about COVID-19 infection and vaccine, such as the severity of COVID-19, trust in the vaccine, COVID-19 vaccination status, COVID-19 infection, reinfection after natural infection or vaccination, reinfection severity, the reason for vaccine hesitation, opinion about COVID-19 protection via natural and conventional ways, and government measurements of COVID-19 and vaccination policy.
2.3. Data Analysis
A descriptive analysis was conducted using SPSS (version 20.0), and the results were presented in tables and figures.
3. Results
3.1. Demographic Characteristics
The current study involved 1426 individuals from six major cities in Pakistan, and Table 1 shows the sociodemographic attributes of the study participants. Out of 1426 participants, 44.6% were males and 55.4% were females. Most participants were between the ages of 14 and 24, followed by those between the ages of 25 and 35, with a small percentage between the ages of 40 and 50. According to their place of residence, most study subjects (75.6%) lived in cities, while only 24.4% lived in rural areas. Most study participants (89.8%) had a university-level education, followed by a college-level education (8.7%). In total, 63.2% of participants were unemployed, 19.9% worked in the private sector, and 40.5% worked in healthcare.
| Demographic Characteristics | No. (%) |
|---|---|
| Gender | |
| Male | 636 (44.6) |
| Female | 790 (55.4) |
| Age | |
| 14 – 24 | 997 (69.9) |
| 18 – 28 | 80 (5.6) |
| 25 – 35 | 216 (15.1) |
| 29 – 39 | 48 (3.4) |
| 36 – 46 | 46 (3.2) |
| 40 – 50 | 14 (1) |
| 47 – 57 | 18 (1.3) |
| 51 – 61 | 3 (0.2) |
| ≥ 58 | 4 (0.3) |
| Rural | Area of residence |
| Urban | 348 (24.4) |
| Uneducated | 1078 (75.6) |
| School level | Education level |
| College level | 0 (0) |
| University level | 22 (1.5) |
| Yes | 124 (8.7) |
| No | 1280 (89.8) |
| Current working status | Health care workers |
| Private sector | 577 (40.5) |
| Government sector | 849 (59.5) |
| Semi government sector | |
| Unemployed | 284 (19.9) |
Demographic Characteristics of the Study Participants (n = 1426) a
3.2. COVID-19 Severity and Vaccine
Regarding the severity of COVID-19, most respondents believed it was a severe disease if contracted. At the same time, the remaining participants were either unsure or believed it was a non-severe disease, as indicated in Table 2. The COVID-19 vaccination was trusted by 78% of the subjects, hesitated by 14.4%, and was not trusted by the remaining 10%. Most participants (91.1%) had been immunized against COVID-19. Our survey showed that 92.4% of the participants favored vaccination if it was available freely. The remaining participants were either unsure or refused vaccination. Approximately 19.9% of research participants were naturally infected with COVID-19, 12% were unsure of their past infection, and 68.1% reported not being infected with COVID-19. Only 10.2% of participants had a history of reinfection with COVID-19. Among the participants, 15.9% considered the reinfection more severe than the first infection, while 20% considered it less severe (Table 2).
| Question | Responses (%) |
|---|---|
| 1. Do you think COVID-19 is a severe disease if you get infected? | |
| Yes | 1095 (76.8) |
| No | 178 (12.5) |
| Not sure | 153 (10.7) |
| 2. Do you trust the vaccines? | |
| Yes | 1112 (78) |
| No | 109 (7.6) |
| Not sure | 205 (14.4) |
| 3. Are you vaccinated against COVID-19? | |
| Yes | 1299 (91.1) |
| No | 127 (8.9) |
| 4. If the vaccine were easily available, would you take it? | |
| Yes | 1318 (92.4) |
| No | 53 (3.7) |
| Not sure | 55 (3.9) |
| 5. Are you naturally infected with COVID-19? | |
| Yes | 284 (19.9) |
| No | 971 (68.1) |
| Not sure | 171 (12) |
| 6. Have you had COVID-19 reinfection despite vaccination, or have you previously been naturally infected with COVID-19? | |
| Yes | 145 (10.2) |
| No | 1044 (73.2) |
| Not sure | 237 (16.6) |
| 7. Was the second infection more severe than the first infection? | |
| Yes | 23/145 (15.9) |
| No | 29/145 (20) |
| Not applicable | 93/145(64.1) |
| 8. In your opinion, will you be protected from COVID-19 in natural and traditional ways? | |
| Yes | 697 (48.9) |
| No | 326 (22.9) |
| Not sure | 403 (28.3) |
| 9. Do you think the government should enforce COVID-19 vaccination and make the vaccine mandatory? | |
| Yes | 1041 (73) |
| No | 161 (11.3) |
| No comments | 224 (15.7) |
Study Participants' Responses About COVID-19 and Vaccination
3.3. COVID-19 Vaccine Hesitancy and People's Perception
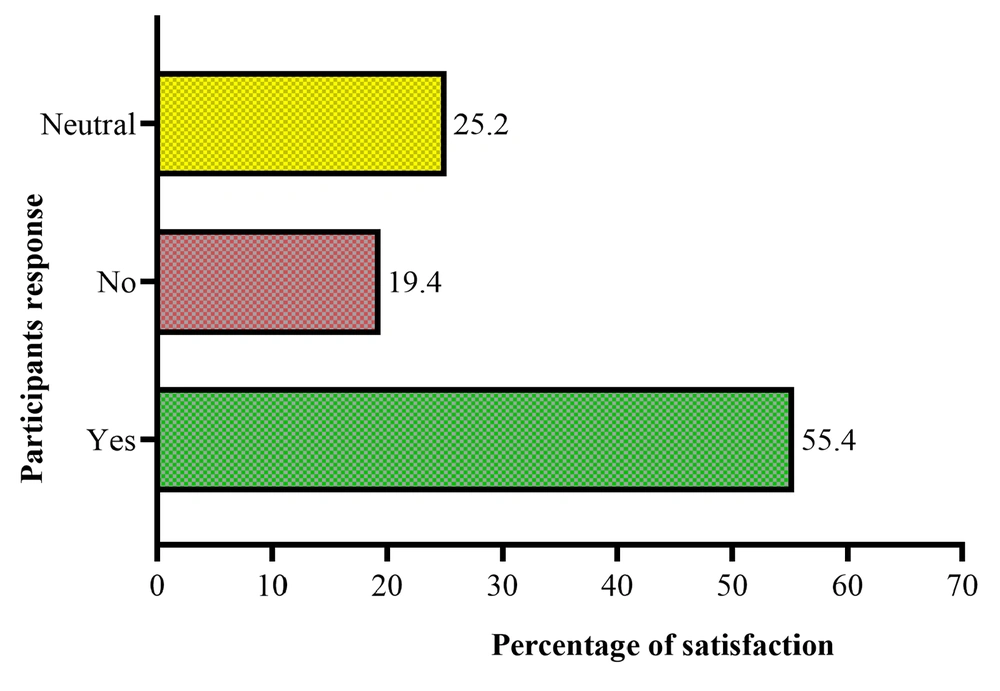
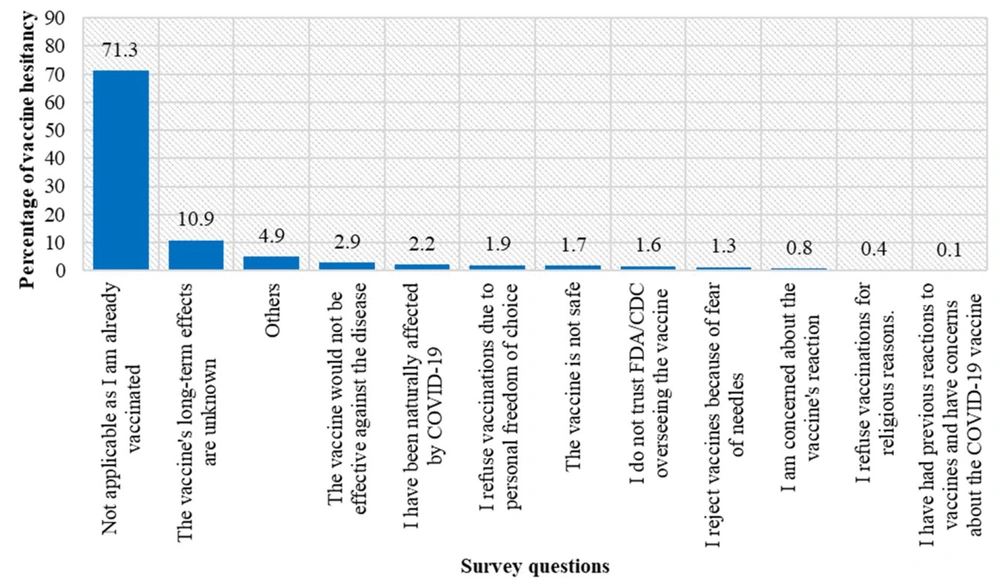
The main concern expressed by research participants regarding vaccination reluctance was; “the vaccine may have unanticipated negative effects in the future." Additionally, vaccine hesitancy was attributed to the following: they were naturally infected with COVID-19, and the vaccine would not be of any benefit; they were free to choose and did not wish to be vaccinated for religious reasons; they did not trust the FDA/CDC for vaccine development; they feared needles and did not wish to be vaccinated. Figure 1 shows the percentage distribution of participants' satisfaction with government measures for controlling COVID-19 infection. Figure 2 illustrates the hesitancy of participants in receiving the COVID-19 vaccine.
4. Discussion
Past experiences have demonstrated the importance of vaccination in preventing pandemics (11, 12). The prior research on vaccine impact and dynamic models for vaccine acceptability in the public has increased. However, the COVID-19 vaccination has raised numerous concerns among the people of different countries around the world (13-16). Population trust in COVID-19 vaccinations is as crucial as their efficacy, accessibility, and immunization reliability. Legislators must act immediately to communicate with community members to build faith in vaccines and combat incorrect information and speculation regarding the COVID-19 vaccination. Even during vaccination, post-marketing surveillance is critical for building trust. Recognizing the social and historical impacts of vaccination reluctance and denial is necessary for creating compelling regional solutions (17).
The current study showed that 76.8% of people in Pakistan believed that COVID-19 was a severe disease, and about the same percentage (78%) of people also trusted vaccines. Despite the low belief in the severity of COVID-19 (76.8%) and trust in vaccines (78%), an unexpectedly high percentage (92.5%) said they would get the COVID-19 vaccination if it were readily available. A previous study found that 66.8% of respondents trusted vaccines and that 70.8% would accept the COVID-19 vaccine if available. This difference may be explained by the fact that most of the subjects in the current study were from schools (1.4%), colleges (8.7%), and universities (89.8%), and no participant was uneducated. Most of the enrolled subjects in this study belonged to urban areas (n = 1077; 75.6%) as opposed to rural areas (n = 348; 24.4%). As a second point, the high acceptance rate of the COVID-19 vaccine in the current study might be attributed to the high percentage of enrolled subjects (n = 577; 40.5%) who were directly or indirectly affiliated with the healthcare profession. Moreover, a third reason for Pakistan's high vaccination rate may be that all government and private sector institutes must follow COVID-19 standard operating procedures (SOPs), including vaccinations. Furthermore, trust in vaccines grows yearly, and more people are willing to receive the COVID-19 vaccine every year. Similarly, a study from China reported that 88.02% of participants were willing to receive the COVID-19 vaccination, and the same study predicted that this percentage would increase in the future (18).
Epidemiological studies are essential for managing infectious diseases and assessing immunity in studied populations. They can provide us with an indication of how far a particular population is from herd immunity (19). The results of the current study revealed that 19.9% (n = 284/1426) of subjects were naturally infected with COVID-19, and 12% (n = 171/1426) were unsure about their status. An earlier study on 15,000 healthcare workers randomly selected from Pakistan found that 33% of the subjects tested positive for the COVID-19 IgG antibody (20). RT-PCR studies on HCW from the Netherlands and the United Kingdom showed that 11.2% and 18% of the subjects were positive for COVID-19, respectively (21, 22). An Italian study showed that 9% of subjects tested positive for COVID-19, confirmed by RT-PCR (23).
In this study, the prevalence of COVID-19 natural reinfection or reinfection following COVID-19 vaccination was 10.2% (n = 145). Among the remaining subjects, 73.2% were not re-infected with COVID-19 or were unsure (16.6%) of their status. In a recent follow-up study from Bangladesh, the reinfection rate after nearly one year of follow-up was 5.7% (24). Similarly, a study on 5865 COVID-19 patients reported that 5% (n = 284) of subjects were re-infected with COVID-19. Moreover, it was demonstrated that reinfection cases were lower at the start of COVID-19, but with time, reinfection cases increased in number (25). A study conducted by the CDC has even shown that during the Omicron period, the percentage of reinfection increased up to 50%, which requires stringent policy to hold up the impact of these infections (26-28).
It has been reported that COVID-19 reinfection is less severe and lethal than the primary infection (29). The current survey study in Pakistan shows that 16 % of the enrolled subjects considered reinfection more severe than the primary infection, while 20 % considered it less severe. A previous study about the reinfection severity has shown that 68.8% (11/16) experienced similar severity, 18.8% (3/16) experienced worse symptoms, and 12.5% (2/16) experienced milder symptoms with the second episode (30). A study of 473 re-infected COVID-19 patients from Bangladesh revealed that 11.9% experienced severe symptoms, 12.9%, 8.9%, and 66.3% were asymptomatic, mild, and moderate, respectively. Almost 13% of subjects had oxygen saturation levels below 90% (31).
Natural products possess anti-infectious properties with tolerable toxicity and have been used against infectious agents for centuries (32). Traditional and natural methods for preventing infectious diseases are practical and more common in Eastern Countries. Lemongrass was considered a traditional medicine in Southwest Asian countries considering its healing ingredients such as ketones, terpenes, aldehydes, and esters (33-35). There is a high demand for herbal medicine against COVID-19 in developed and underdeveloped countries. More than 125 plant species have been reported to be used in formulations against COVID-19 infection in China as herbal medicines against COVID-19 (36). Additionally, micronutrients are pivotal in preventing and treating COVID-19 (37, 38). The current study found that 48.9% of participants believed traditional and natural methods would protect them against COVID-19, 22.8% did not trust traditional methods, and 28.3% were unsure. A survey study conducted in Jordan on 386 subjects revealed that more than half of the participants used one or more natural products. It was found that citrus fruits, honey, ginger, cinnamon, star anise, and cloves were the most commonly used natural products (39). Pakistan also took several preventative measures to control the COVID-19 pandemic, such as lockdown periods, public gatherings bans, and closing markets, schools, and other institutions, despite relying on e-learning as an alternative during the pandemic (40).
Additionally, awareness and vaccination programs were launched in the country. In the current study, 73% (1047) of respondents were satisfied with government measures, while 11.3% were unsatisfied with vaccination and preventive measures. An analysis of 200 participants from Saudi Arabia revealed that 55% were satisfied with the preventive measures, and 24% opposed the COVID-19 restrictions (41).
4.1. Conclusions
The current survey conducted across major cities in Pakistan revealed that most respondents trusted the COVID-19 vaccine and demonstrated high confidence and acceptance of vaccination. Re-infected patients experienced almost similar degrees of reinfection severity. Half of the study subjects, similar to those in other countries worldwide, believed in traditional and herbal medicines specifically for treating COVID-19 infections. Furthermore, most respondents were satisfied with the government's initiatives for COVID-19. To fully understand the numerous reasons for vaccine hesitancy, more studies are needed, which will enhance the vaccine's acceptability and practicality.