1. Context
In late December 2019, some mysterious cases of pneumonia with unknown etiology were reported in Wuhan, China. The contagious virus has caused public health concerns worldwide, and the World Health Organization (WHO) declared the disease a pandemic on March 11, 2020 (1). The global crisis caused by the COVID-19 pandemic has posed many challenges to policymakers and health officials, forcing them to adopt emergency policies across a range of sectors to control the disease (2). Vaccination is one of the most important public health measures in history (3, 4), and effective vaccination, along with effective public health measures, is crucial to reducing the epidemic of COVID-19 (5). The duration of symptoms in COVID-19 patients is usually 2 weeks for mild cases and 3 - 6 weeks for severe cases. The clinical problems may continue long after the acute stage of the disease. Depending on the severity of the disease, they are called "long–COVID-19 syndrome" (symptomatic for 4 to 12 weeks) or “post–COVID-19 syndrome" (symptomatic for more than 12 weeks) (6). "Long COVID" or "post-acute COVID-19 syndrome" is characterized by persistent symptoms that may fluctuate over time and occur after contracting SARS-CoV-2. Many complain about fatigue, brain fog, and mental difficulties, and ~200 symptoms are described (7). Common symptoms include headache, joint pain, myalgia, weakness, insomnia, impaired balance and gait, neurocognitive issues, diarrhea, rash or hair loss, fatigue, breathlessness, cough, chest pain, and palpitations (8). PTSD, speech impairments, and difficulties with swallowing and nutrition can reduce daily activities and overall health-related quality of life (QOL) (6, 9). According to studies, the incidence rate of 10 - 30% of non-hospitalized cases, 50 - 70% of hospitalized cases (10), and 10 - 12% of vaccinated cases have been reported (11). Management of long-COVID patients needs a multidisciplinary approach, which includes assessment, treatment of symptoms, physiotherapy, occupational therapy (OT) (12), and psychological support (8). Occupational therapy is an essential member of the rehabilitation team, with a focus on maximizing patient function and independence. The primary goal of occupational therapy is to increase patient autonomy and prevent further functional decline by utilizing meaningful activities and occupations that can positively impact their participation in daily life. The therapy aims to assist individuals in regaining physical, cognitive, and emotional abilities, enabling them to engage in meaningful activities and improve their overall QOL. Common interventions used for symptom management include energy conservation, work simplification, pulmonary rehabilitation, compensatory strategies, sleep hygiene, and strategies for returning to previous activities (13). ‘Long COVID’ is a major dilemma, difficult to diagnose and even more challenging to treat. Occupational therapy plays a significant role in promoting independence in activities of daily living (ADLs) and improving patients' QOL; however, the areas where OT can be effective in these conditions are not clear. The aim was to conduct a scoping review that would identify the specific areas covered in previous studies on the role of OT in managing post-COVID symptoms.
2. Evidence Acquisition
The research was a scoping review that adhered to the writing principles recommended by Arksey and O'Malley for this type of review. The review framework comprised five stages. This involves the identification of the research question and relevant studies, as well as the selection of appropriate studies, itemizing the data found, clustering, providing a brief overview, and presenting the findings. By adhering to this framework, the study was able to conduct a thorough and comprehensive review of the literature on the topic under investigation (14).
2.1. Research Questions
In this research, the fundamental inquiries to be addressed were as follows:
How does occupational therapy intervene in post-COVID symptoms, including cognitive and physical symptoms, and what benefits does it offer to enhance overall QOL by managing these symptoms?
To identify relevant studies on interventions or approaches within the scope of OT intervention in post-COVID Symptoms, several databases were searched from 2019 to April 2023. These databases included Google Scholar, PubMed, SCOPUS, ISI Web of Science, and Elsevier. Inclusion and exclusion criteria were applied for article selection to focus the literature further and answer the research question. The inclusion criteria were: Papers published in the determined interval, papers published in English or Persian, studies investigating the use of occupational therapy, and both individual and group interventions were included. The terms that were utilized were: Occupational therapy, long-COVID, and post-COVID syndrome; the exact term used in databases was: (("occupational therapy") AND (("post-COVID") OR ("long-COVID"))) AND ((intervention) OR (exercise)).
2.2. Study Selection
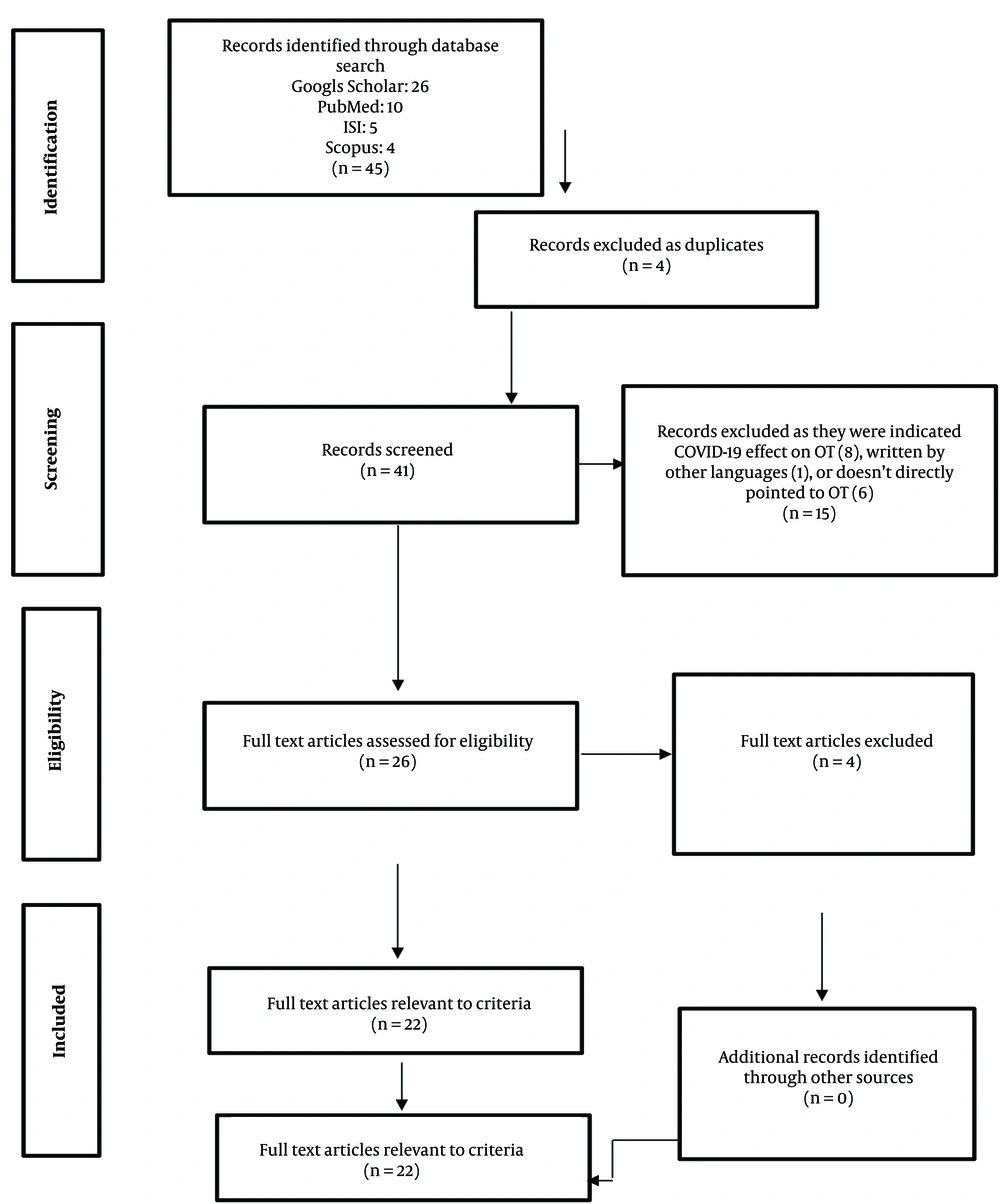
To be included in the review, papers should cover effective information regarding the aim of this article. Articles written in English and published between late 2019 and 2023 were included. The article incorporated a range of sources, including randomized clinical trials, reflective articles, performance guides, review articles, and cohort studies. A hand search was completed to find articles not identified in the databases but referenced in a journal article. Key authors were noted, and an electronic search of their peer-reviewed and published papers was conducted. The review excluded data from presentations, conference proceedings, non-peer-reviewed research literature, dissertations, and theses. The preferred reporting items for systematic reviews and meta-analyses extension for scoping reviews (PRISMA-ScR) checklist (15) was used to enhance reporting and provide a visual of the article selection process (Figure 1).
2.3. Itemizing the Data Found
The articles found in the search were judged first by the study’s title, aim, and summary. Articles without the eligibility criteria were excluded. When the first judgment was made, the relevant information was listed after completing the studies. For each determined category, a table including the title, authors, publication year, results, and a simple summary was provided to give a quick review to the readers.
Titles and abstracts of the retrieved papers were screened by one author (S.Z.) to identify relevant literature. Full-text copies of retained papers were then reviewed, and reference lists were searched by this author to identify any further relevant literature. In addition, two authors (A.R. and S.Gh.) each reviewed half of the full texts. Disagreements regarding inclusion, quality, and relevance were resolved through discussions involving all reviewers.
The research was granted approval by the Ethics Committee of Shiraz University of Medical Sciences (SUMS) with the code (IR.SUMS.REHAB.REC.1401.025), indicating that ethical considerations were taken into account during the research.
3. Results
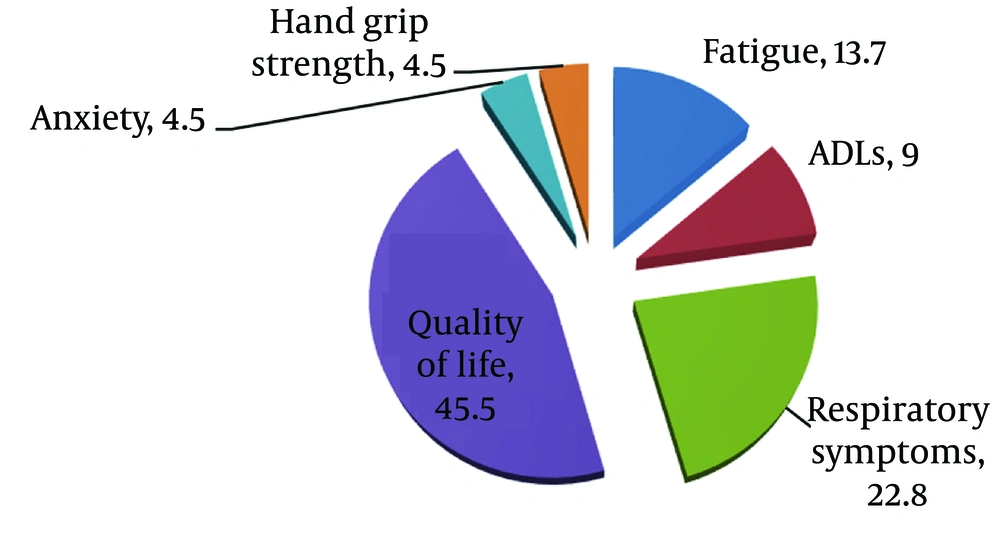
Out of 45 articles, 22 were chosen according to the established inclusion and exclusion criteria, and the results were discussed in a continuous manner. From the total of extracted articles, the details according to databases are as follows: 26 in Google Scholar, 10 in PubMed, 5 in ISI, and 4 in Scopus. Table 1 was created to provide readers with quick access to important information and a brief overview of the included articles, including their aims and results. The distribution of studies carried out based on the role of occupational therapy intervention is depicted in Figure 2. The overall importance and effectiveness of occupational therapy exercises were discussed in different classifications, such as physical, cognitive, QOL, and return to daily life, which confirmed the role of OTs in post-COVID symptoms.
| Title | Author | Year | Country | Type of study | Summary | Result |
|---|---|---|---|---|---|---|
| Multidisciplinary collaborative consensus guidance statement on the assessment and treatment of fatigue in PASC patients | Herrera et.al. (16) | 2021 | USA | Practical guideline | Assessment and treatment role of rehabilitation team in management of fatigue through a program depended on fatigue severity and Energy conservation strategies, Encourage patients following healthy diets and to be hydrated during the day, Pharmacologic therapy and supplements, and focus on health equity. | Develop an activity-based program for individuals with mild to moderate fatigue. For mild fatigue, patients are advised to gradually resume household and community activities, following the "rules of ten," before progressing to more intensive activities and exercise. For moderate fatigue, patients are encouraged to continue with tolerated household and limited community activities. For severe fatigue, patients should only engage in tolerated household activities that do not exacerbate their symptoms. |
| Occupational therapy-based energy management education in people with post-COVID-19 condition-related fatigue: Results from a focus group discussion | Hersche and Weise (17) | 2022 | Switzerland | Qualitative research | The study aimed to examine the initial encounters of OTs who utilized the EME protocol to aid individuals experiencing long COVID-related fatigue. Additionally, the research sought to collect feedback from OTs on how to improve and modify the EME protocol. EME is a structured self-management education that has been integrated into new services. | According to a report by nine OTs working in different settings in Switzerland, the energy management education protocol is appropriate for both inpatient and outpatient contexts. Nevertheless, they recommended that the EME materials could be improved. |
| Exploring the ability to perform activities of daily living and cognitive status after hospitalization with COVID-19: A multiple case study | Christensen et.al. (18) | 2022 | Denmark | Case study; sample size: 3 | The aim is to assess the clients' capacity to carry out their daily activities and cognitive function upon discharge and three months post-discharge. | The study included eleven patients, of which 75% demonstrated a noteworthy improvement in motor ability, and 27% showed a significant improvement in process ability during follow-up. Moreover, 67% of the cases displayed mild cognitive impairment, particularly in executive function and memory. |
| Occupational therapy interventions in pulmonary rehabilitation–an update in the COVID-19 ERA | Ciubean et.al. (13) | 2021 | Romania | Review | The primary goal of OT in pulmonary rehabilitation is to instruct patients on breathing techniques during rest and task performance. Furthermore, OT aims to improve upper limb tolerance through exercises, simplify daily activities, teach patients to seek assistance, plan their day/week, organize their environment, and provide patient training. | To address respiratory disability-related issues, it is recommended to incorporate OT intervention as part of comprehensive pulmonary rehabilitation. Occupational tasks should be customized to specific activities and related symptoms. However, there is a dearth of standardized protocols and outcome definitions for occupational therapy intervention during pulmonary rehabilitation. |
| Occupational therapy productions in times of pandemic: A systematic review of occupational therapeutic actions against the new coronavirus (COVID-19) epidemic | Ramos Ataide et.al. (19) | 2021 | Brazil | Review | The objective is to conduct a review of the available resources concerning OT during the pandemic and to offer support and improve professional practices. | The results showed that the authors were quick to respond to the challenges and barriers presented by the COVID-19 pandemic in the realm of occupational therapy. |
| Post-COVID-19 syndrome: Improvements in health-related QOL following psychology-led interdisciplinary virtual rehabilitation | Harenwall et.al. (12) | 2021 | UK | Pilot; sample size 200 | To understand the needs of the "Recovering from COVID" program, a biopsychosocial approach is necessary, with a particular emphasis on PVF that requires an interdisciplinary team. This team includes a clinical psychologist, physiotherapist, OT, dietitian, speech and language therapist, assistant psychologist, and a personal support navigator, with the support of a team administrator. | Following the rehabilitation program, 76 individuals were evaluated and exhibited noteworthy progress in PVF, sleep optimization, nutrition, swallowing, activity management, energy conservation, stress management, breathing optimization, managing setbacks, and signposting. |
| Postdischarge symptoms and rehabilitation needs in survivors of COVID‐19 infection: A cross‐sectional evaluation | Halpin et.al. (9) | 2020 | UK | Cross sectional; sample size 100 | The information available on the nature and frequency of post-COVID-19 symptoms is limited. | Fatigue was the most commonly reported symptom associated with the disease, followed by breathlessness and distress. |
| Return to work after COVID-19: An international perspective | Asaba et.al. (20) | 2022 | Sweden | Review | The aim is to identify the factors that influence the return to work of adults in various countries. | The article emphasized the importance of evidence-based knowledge in occupational therapy regarding factors that impact return to work (RTW), including social insurances and guidelines for employers. |
| Pulmonary tele-rehabilitation in patients (post COVID-19) with respiratory complications: A randomized controlled trial | Pratibha et.al. (21) | 2022 | India | RCT; sample size 30 | Tele-rehabilitation is recognized as a valuable service for COVID-19 patients, enabling them to undergo rehabilitation from the comfort of their homes. | Clients had a positive perception of tele-rehabilitation and found it to be a feasible and cost-effective solution. |
| Persistent COVID and a return to sport | Giusto et.al. (22) | 2022 | USA | Discuss a framework for athletes | The aim is to suggest a framework that primary care physicians and sports medicine professionals can utilize to evaluate COVID long-haulers and support their re-entry into sports. | Fatigue and cardiopulmonary symptoms are the primary limiting factors, and once they are reduced, exercise can be resumed. |
| Addressing the post-acute sequelae of SARS-CoV-2 nfection: A multidisciplinary model of care | Parker et.al. (23) | 2021 | Different countaries | Clinical model | PASC is characterized by a range of complex and multifactorial impairments, including fatigue, dyspnea, cough, headache, loss of taste or smell, and cognitive or mental health issues. Managing these symptoms requires a coordinated and multidisciplinary approach. | Post-acute care programs that involve multiple disciplines can offer assistance to patients in both hospital and non-hospital settings as they recover. |
| Canadian thoracic society position statement on rehabilitation for COVID-19 and implications for pulmonary rehabilitation | Beauchamp et.al. (24) | 2022 | Canada | Guideline | The aim of this article is to present a summary of the CTS's position on the rehabilitation of patients with persistent symptoms of COVID-19 infection. | Therapists can safely and effectively provide pulmonary rehabilitation through virtual means. |
| A single session of virtual reality improved tiredness, shortness of breath, anxiety, depression and well-being in hospitalized individuals with COVID-19: A randomized clinical trial | Rodrigues et.al. (25) | 2022 | Brazil | RCT; sample size 44 | During hospitalization, therapists have employed various strategies to improve patients' well-being, including the use of VR. | VR is a tool that can improve fatigue, breathlessness, anxiety, and depression in patients. |
| Short-term effects of a three-week inpatient Post-COVID-19 pulmonary rehabilitation program-a prospective observational study | Hayde et, al. (26) | 2021 | Germany | Prospective observational study; sample size 120 | Pulmonary rehabilitation was customized to meet the specific needs of each patient, in accordance with the latest recommendations. | Dyspnea was the first symptom, followed by cough and sputum, which impacted physical capacity, lung function, fatigue, QOL, depression, and anxiety. |
| Post-COVID-19 chronic fatigue and the role of energy conservation and work simplification techniques: An occupational therapy approach | Bhavna and Kirti Sundar (27) | 2022 | India | Approach | Many of the symptoms experienced by post-COVID survivors can be effectively managed, with fatigue being the most prevalent. | Energy conservation, work simplification, and assistive and adaptive technologies can enhance the QOL of patients who have recovered. |
| A multidisciplinary NHS COVID-19 service to manage post-COVID-19 syndrome in the community | Parkin et.al. (28) | 2021 | UK | Approach | A rehabilitation system consisting of three tiers has been implemented to match the patient's needs with suitable services and interventions. | This service was established to meet the needs of patients and integrate the most recent information on post-COVID-19 syndrome. |
| Rehabilitation at the time of pandemic: Patient journey recommendations | Negm et. al. (29) | 2022 | Canada | Review | Enhance rehabilitation recommendations during the COVID-19 pandemic. | The recommendations underscore the importance of assessing neurorehabilitation, speech, musculoskeletal, respiratory, and cardiac rehabilitation individually, in accordance with established protocols. |
| Behavioral interventions in acute COVID-19 recovery: A new opportunity for integrated care | Jaywant et al. (30) | 2021 | USA | Report | Patients receive medical supervision and engage in daily physical therapy and occupational therapy to achieve their rehabilitation goals. | Behavioral interventions may lead to a reduction in long-term psychiatric morbidity and the utilization of outpatient care. |
| Characteristics of physical, occupational, and speech therapy received by COVID-19 patients in a skilled nursing facility: A retrospective cohort study | Canter et al. (31) | 2023 | USA | Retrospective Cohort study sample size 248 | The study details the length and regularity of occupational, physical, and speech therapy sessions administered to long-term and post-acute care patients with COVID-19. | Patients in post-acute care environments were more likely to receive rehabilitation than those in long-term care settings. |
| Systematic review of post-COVID-19 syndrome rehabilitation guidelines | Marshall-Andon et al. (32) | 2023 | UK | Systematic review | The objective of this systematic review was to offer clinical leads and commissioners a comprehensive summary of clinical and service guidelines for post-COVID-19 syndrome rehabilitation, with the aim of identifying optimal practices for the rehabilitation of patients impacted by this condition. | There was a lack of clarity regarding management options, outcome measurement, and discharge criteria. |
| Rehabilitation of post-COVID-19 musculoskeletal sequelae in geriatric patients: A case series study | Cevei et. al. (33) | 2022 | Romania | Case series study; sample size 91 | This case series study focused was on evaluating the effectiveness of an early program using goal-oriented rehabilitation in elderly people after acute COVID-19. The complex rehabilitation treatment, continued for 4 weeks, and included: Exercise therapy, robotic gait training, occupational therapy, and massages. Evaluations performed by the Barthel Index and functional independence measure for ADLs. | Early complex and combined rehabilitation program enhanced functional independence and autonomy in very old patients, post-COVID-19 to perform ADLs. |
| Hand grip strength in post-COVID-19 individuals: Comparison of two approaches in occupational therapy | Roldão (34) | 2022 | Portugal | Cross-sectional | The objective of this study was to compare two Occupational Therapy interventions to achieve improvements in hand grip strength, in post-COVID-19 individuals, who experienced an inpatient situation. Interventions include conventional Occupational Therapy or the Biometrics E-link® G200 dynamometer with game interface. | OT interventions can show improvements in hand grip strength in post-COVID-19 individuals. |
Abbreviations: PASC, postacute sequelae of SARS CoV‐2 infection; OT, occupational therapy; PVF, post-viral fatigue; RTW, return to work; PASC, post-acute sequelae of SARS-CoV-2 infection; CTS, Canadian Thoracic Society; VR, virtual reality; QOL, quality of life; ADLs, activities of daily living
4. Discussion
Numerous scholarly articles have explored OT structures and guidelines, particularly in the context of COVID-19 recovery. The Royal College of OTs (35) and the Philippine Academy of Occupational Therapy (36) have both published guides emphasizing the role of OTs in promoting functional recovery and patient-centered care. The Royal College of OT utilized the person-environment-occupation (PEO) model to understand evolving needs over time and across different environments, while the Philippine Academy of Occupational Therapy emphasized supporting OTs in promoting individuals' participation through OT, even in epidemic situations, and ultimately preventing the spread of disease (35, 36). Studies have used various assessment tools, like the Montreal Cognitive Assessment (MoCA) and the Assessment of Motor and Process Skills (16), to evaluate patient progress post-COVID-19 (18). Interventions include motor interventions (27, 28, 34), cognitive therapies (18, 23, 28, 29, 37), energy management education (EME) (17), and pulmonary rehabilitation (21, 28, 38), addressing fatigue, breathlessness, and psychological distress (12, 20-23, 26, 28, 36, 39, 40). Strategies such as energy conservation, adaptive equipment, and tele-rehabilitation have proven effective in most studies (16, 17, 21, 27, 28, 40). Research highlights the importance of OT in enhancing the QOL and functional abilities in post-COVID patients (27, 28) and the effective role of occupational therapy in helping these patients return to work and daily functioning (19, 23, 27-30, 37).
Occupational therapy plays a crucial role in managing post-COVID-19 conditions by improving functional independence, cognitive abilities, and overall QOL. Occupational therapy's multifaceted role includes restoring mobility, strength, coordination, and functional independence, as well as managing cognitive impairments and fatigue. Interventions such as sleep hygiene, cognitive strategies, and virtual reality help alleviate symptoms and enhance daily functioning. The importance of a multidisciplinary approach in patient care, involving collaboration among various specialists, including OTs, is also emphasized. A multidisciplinary approach, involving collaboration among various healthcare specialists, is essential for comprehensive patient care and rehabilitation. These efforts collectively aim to restore patients' abilities and promote their well-being and engagement in everyday activities.
The novelty and applicability of the subject, considering the Coronavirus crisis and post-COVID symptoms, especially in rehabilitation and the role of occupational therapy in improving the health and independence of clients, are some of the strengths of this study. On the other hand, some aspects of post-COVID symptoms are just being recognized, and perhaps this issue has been overlooked by researchers. Consequently, this scoping review may have limitations in collecting all aspects of occupational therapy interventions in post-COVID cases.
4.1. Conclusions
We concluded from studies that OTs have been effective in managing post-COVID syndrome. Results revealed that OTs can employ performance-based assessments to identify the rehabilitation needs of patients and provide treatment and training for self-management of symptoms, resulting in substantial improvement in the QOL for individuals who have recuperated from COVID-19 infection. In general, OTs can leverage their expertise in various areas such as health promotion, activity analysis, energy conservation, and lifestyle modification to facilitate engagement in occupations that help clients overcome the sequelae of COVID-19 infection.